INTRODUCTION
In the last decade, there has been global growth of diagnostic and therapeutic procedures being performed outside of traditional operating room locations.
12 Consequently, an increasing number of complex procedures are performed outside the operating room in more and more ill patients. Such an extension of anesthesiology practice beyond the operating room has led to a significant concern about the safety of non-operating room anesthesia (NORA) because of its potential problems (e.g., no fully configured anesthesia equipment, reduced availability of anesthesia manpower due to geographical dispersion, and unfamiliar working environment).
2
Perioperative mortality is a basic measure of quality of care and patient safety in surgical patients, and is generally defined as any death following surgery and anesthesia within 24 hours, 48 hours, or 30 days after surgery.
3 It is clear that anesthesia-related mortality rates of operating room anesthesia (ORA) cases have declined over time in developed countries as a result of improvements in monitoring, medications, and patient care. Two meta-analysis studies reported these rates as 0.3–0.9
4 or < 1 per 10,000 anesthetic cases
5 in developed countries. However, few studies have been performed on the relative safety of NORA cases compared to ORA cases. In particular, although many practitioners suggest that the volume of NORA cases in Korea is rapidly expanding, no research exists on the features and safety of this clinical field in Korea.
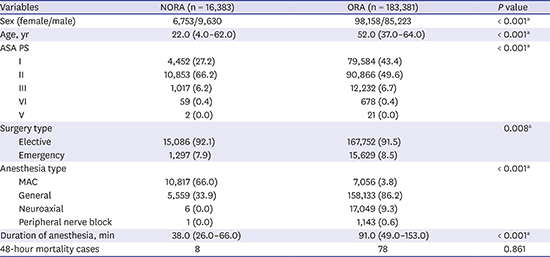
Therefore, we characterized NORA cases and compared their characteristics with those of ORA cases in the surgical population during a 59-month period at a single tertiary university hospital. Furthermore, we compared the rates and causes of deaths occurring within 48 hours of surgery (48-hour mortality) between NORA and ORA cases.
METHODS
We retrospectively analyzed the electronic medical records of patients who underwent surgical procedures under anesthesia services in and outside the operating room at a tertiary university hospital from January 2013 to November 2017. The institution (almost 2,000 beds) has provided surgical services in all areas via three operating theaters with 56 operating rooms, as well as outside operating rooms. The anesthesia services for the outside operating rooms are provided by a dedicated team of anesthesiologists with a professional career of at least 3 years.
We excluded cases of anesthesia in the obstetrics room from the NORA. Though obstetrics room is geographically located outside operating theater, obstetrics cases carry their own unique features which do not reflect typical features of NORA cases. We also excluded cases of anesthesia for cardiac surgery from the ORA group due to their inherently high mortality risk. In addition, we excluded cases of anesthesia for organ donation (i.e., American Society of Anesthesiologists physical status [ASA PS] VI).
For all of the cases, data were obtained on the procedure location, ASA PS, emergency or elective status of the procedure, length of anesthesia, and anesthesia type. A case was considered an “emergency” when designated as part of the ASA PS, even when performed during usual the working hours of 8 AM to 5 PM. Anesthesia type was classified as general, neuroaxial (e.g., spinal, epidural, or combined spinal-epidural), peripheral nerve block, or monitored anesthesia care (MAC). According to the ASA, “MAC” is defined as sedation and/or analgesia provided by an anesthesiologist.
6
The types of procedures for NORA cases were grouped into nine broad categories based on their frequency: gastrointestinal (GI) endoscopic procedures, pediatric computed tomography (CT)/magnetic resonance imaging (MRI), radiofrequency ablation (RFA) (e.g., mostly for hepatic or renal tumor and rarely for bone tumor), cardiology procedures (e.g., catheter ablation for an arrhythmia, cardiac catheterization, implantable electronic device procedures), neurointerventional procedures (e.g., stenting or coil embolization with transfemoral cerebral angiography), proton radiation therapy, electroconvulsive therapy, sclerotherapy, and others.
Mortality analyses were restricted to those patients determined to be dead within 48 hours after surgery because a patient who died later than 48 hours after surgery might have a very low cause and effect relationship with anesthesia. Three anesthesiologists independently reviewed the electronic medical charts of the 48-hour mortality cases to determine the causes of mortality. The principal causes of death were examined and assigned to one of four categories: patient's disease or condition (when comorbidities were the only or the major contributory factor), surgery (when a technical surgical problem was the only or the major contributory factor), anesthesia (when anesthesia was the only or the major contributory factor), and others (e.g., electrical malfunction, fall, or unable to decide from the information provided). In addition, mortality cases were subcategorized according to the specific mechanism causing death as sepsis, bleeding, cardiovascular events, respiratory events, neurological events, hepatic events, renal events, endocrine events, thromboembolic events, allergic or adverse drug reactions, and others. After the first review, disagreements among the three members were resolved by discussion, and agreement was reached in all of the cases when at least two of the three members agreed on the cause of the event. The cases were divided into six groups according to the patient's age to compare the 48-hour mortality rates: < 2 years, 2–11 years, 12–18 years, 19–65 years, 66–75 years, and > 75 years.
Statistical analyses
Mortality rates were expressed per 10,000 anesthetic cases with 95% confidence intervals (CIs). The reported 95% CIs around risk were not adjusted to account for the non-uniform risk introduced by patients who underwent multiple procedures. When comparing two mortality rates, the difference between rates with its 95% CI and associated P value were computed by MedCal for Windows (ver. 18; MedCal Software, Mariakerke, Belgium). In these analyses, the difference between rates was considered statistically significant if their respective 95% CIs did not overlap.
The other statistical analyses were performed with SPSS software (ver. 20; IBM Corp., Armonk, NY, USA). Categorical variables were described as numbers (%) and compared using the Pearson's χ2 test with a continuity correction or Fisher's exact test, where applicable. Continuous variables were tested for normality using the Kolmogorov-Smirnov test. Normally distributed variables were analyzed using the unpaired t-test, while non-normally distributed continuous variables and ordinal variables were analyzed using the Mann-Whitney U test. Statistical significance was set at P < 0.05.
Ethics statement
This study was registered with the Clinical Research Information Service (CRIS,
https://cris.nih.go.kr/cris/en/; No. KCT0002719) and approved by the Institutional Review Board of the Samsung Medical Center (No. SMC 2018-01-034; Approval date, January 16, 2018), who waived the requirement for written informed consent due to the retrospective nature of the study.
DISCUSSION
Perioperative mortality is an objective endpoint that can be used to evaluate anesthesia or surgical safety within and between hospitals, and to test the effectiveness of changes in clinical practice.
37 In developed countries, perioperative mortality has been estimated to vary between 1.4 and 18.9 per 10,000 anesthetic cases in non-cardiac surgery,
58 which depends on the timing of the evaluation, the patient population, hospital setting, urgency, and the patient's risk profile. Despite including all age groups and emergency operations, our 48-hour mortality rate in the ORA cases (4.3 per 10,000 anesthetic cases; 95% CI, 3.4–5.3) was within this range.
The proportion of NORA cases from January 2013 to November 2017 accounted for 8.2% of all cases provided with anesthesia services at our hospital. This is the first time the proportion of NORA cases has been reported for a Korean hospital. This proportion of NORA cases is somewhat low compared to the 12.7% at the Massachusetts General Hospital in the United States in 2006.
1 This difference may be related to our anesthesia departmental culture being reluctant to perform NORA due to a shortage of manpower, although our hospital is one of the leading Korean hospitals in the volume of NORA cases.
Several previous reports
129 commonly pointed out the typical safety hazards of NORA such as limited availability of monitoring/anesthesia equipment, reduced availability of anesthesia manpower (especially, severely limited in an emergency situation), unfamiliar environment, absence of a properly equipped recovery room, or deliberate ignorance of practitioners about the adherence to the standard of care (due to relatively less-invasive procedures or sedation). Actually, a previous ASA Closed Claims study
9 using the database with entries from 1990 to 2002 demonstrated that the proportion of mortality cases was significantly higher in NORA than in ORA cases (54.0% [47/87] vs. 28.9% [949/3,287],
P < 0.001).
However, in this study, 48-hour mortality of the NORA cases was similar to that of the ORA cases (4.9 per 10,000 anesthetic cases [95% CI, 2.1–9.6] vs. 4.3 per 10,000 anesthetic cases [95% CI, 3.4–5.3], P = 0.710). Such an unexpected result may be attributed to the improved quality control of NORA. More specifically, our safety measures for MAC, the predominant anesthetic technique (66.0% of NORA cases), may have had a favorable effect. At our hospital, an experienced anesthesiologist (one of the dedicated team of anesthesiologists for NORA) teams up with a well-trained nurse, and they have been continuously in charge of every NORA case. In addition to standardized care and monitoring, such an organization of anesthesia manpower enables the anesthesia services in a variety of remote locations to be performed as safely as in the operating room. However, considering the relatively low imbursement of MAC (nearly 85.0% of the general anesthesia fee based on 1 hour) by the Korean National Medical Insurance, it is not easy to maintain a similar degree of manpower and facilities for dispersed locations outside the operating room to those in the operating suite.
As shown by our results, it is clear that NORA cases involve healthier patients, a greater number of brief duration procedures, and a lower proportion of emergency procedures than those of ORA cases. In this regard, there may be more room for improving mortality of the NORA cases. As an anesthesia practice can be influenced by reimbursement patterns, increasing the fee for MAC up to the general anesthesia fee may be one possible governmental policy for improving patient safety in NORA.
In this study, except for the lack of a difference between patients with ASA PS I and II, the NORA cases showed a significantly increasing relationship between mortality and a higher ASA PS. These findings were similarly observed in the ORA cases. After the first introduction of the ASA PS classification system in 1941, ASA PS has been proven to be a reliable predictor of outcomes after surgery
5810 or GI endoscopic procedures.
11 The most surprising result was that all of the cases with ASA PS V in both groups resulted in death within the first postoperative 48 hours. By definition, 50% of patients with ASA PS V are not expected to survive 24 hours with or without their planned operative procedure. Lagasse
8 suggested a 48-hour mortality rate of 1:4.5 for ASA PS V. Considering a quite low proportion of ASA PS V in the present study (0.01% of ORA cases vs. 0.4% in that study), such a difference in mortality rates may be caused by underestimated ASA PS classifications (i.e., rating of ASA PS VI in patients with an actual ASA PS V) at our hospital. ASA PS misclassifications are relatively common in teaching hospitals due to all of the trainees at our hospital.
12
For further improvement of perioperative mortality in NORA cases, it is noteworthy that patients aged < 2 years showed relatively higher mortality rates compared to patients aged 2–11 years and 19–75 years in the NORA cases of this study. A previous study
13 identified extremes of age (very young and old ages) as an independent risk factor for perioperative mortality in ORA cases, which was confirmed by this study. Perioperative mortality rates in a pediatric population were 10.7 in an Indian study
14 and 40.0 in the registry of the United States
15 per 10,000 anesthetic cases for non-cardiac surgery performed in an operating suite. However, despite a recent increase in the number of pediatric NORA cases, mortality has not been quantified. In this study, MAC was performed in 80.2% (1,704/2,125) of the NORA cases in this age group. Because adherence to the standard of care is deliberately ignored during sedation (particularly for diagnostic procedures), we believe that an overall improvement of patient safety in NORA is best achieved by focusing on strict adherence to the standard of care in the MAC for this age group (e.g., provision of experienced and certified personnel, adequate preparation based on the individual patient risk profiles, and sufficient monitoring and equipment).
Perioperative mortality is associated with three major categories of risk factors: patient condition or disease, the surgical procedure itself, and risks directly related to anesthesia management. Consistent with previous studies,
16 a patient's disease or condition was the major triggering factor for perioperative mortality (76.7% of the mortality cases) in this study. More specifically, sepsis with multi-organ failure was the most common mechanism of death, which accounted for 30.2% (26/86) of all mortality cases. These findings are consistent with another study
17 demonstrating that sepsis is the leading cause of mortality in surgical patients with mortality > 50%.
In this study, anesthesia-related mortality was only identified in the ORA cases (two cases). As a result, overall anesthesia-related mortality rate was 0.1 per 10,000 anesthetic cases (95% CI, 0.0–0.4). According to a meta-analysis that quantified the global risk for anesthesia-related mortality, anesthesia-related mortality rates in 1990–2009 were estimated to be 0.3–0.9 and 1.4–4.7 per 10,000 anesthetic cases in developed countries and developing countries, respectively.
4 Despite the high patient baseline risks and complexity of surgery inherent to a tertiary hospital, patient safety during anesthesia seems to be acceptably controlled at our hospital.
This study should be interpreted in the context of the following limitations. First, this study was representative of the experience at a single tertiary hospital. Our NORA safety profiles may not represent the entire spectrum of NORA practices. In this regard, a multi-institutional NORA database will be needed to provide more insights into fatal mechanisms and to facilitate the development of universally applicable strategies. Second, excluding cardiac surgery from the ORA cases clearly influenced our perioperative mortality rates. In studies that included cardiac surgery,
16 the perioperative mortality rates were significantly higher in cardiac surgery compared to non-cardiac surgery. Contrary to our results, a recent study
18 using the large voluntary reporting system in the United States, in which cardiac surgery cases were included in ORA cases, reported that overall mortality was higher in ORA cases versus NORA cases (0.04% vs. 0.02%,
P < 0.0001). Lastly, the mortality analyses were limited to those patients who died within 48 hours after surgery. Thus, all surgery- or anesthesia-related mortalities may not have been captured in this study.
In conclusion, our results derived from a total of 199,764 anesthetic cases at a tertiary hospital demonstrated that a considerable portion (8.2%) of anesthesia services was provided outside the operating room. In addition, the 48-hour mortality rate of the NORA cases was low (4.9 per 10,000 cases; 95% CI, 2.1–9.6) and similar to those identified in the ORA cases, which should be noteworthy when considering that NORA cases involved healthier patients, less invasive briefer procedures, and a lower proportion of emergency procedures. Similar to the ORA cases, higher ASA PS and very young age (< 2 years) were significantly associated with perioperative mortality in the NORA cases. Considering the increasing demands in many hospitals for remote anesthesia services, an improved understanding of the nature and mortality due to anesthesia outside the operating room will contribute to appropriate policy-making in the setting of evolving healthcare systems for government, improved perioperative care for practitioners, and better informed decisions for patients.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download