1. McTavish D, Campoli-Richards D, Sorkin EM. Carvedilol. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy. Drugs. 1993; 45(2):232–258.
2. Keating GM, Jarvis B. Carvedilol: a review of its use in chronic heart failure. Drugs. 2003; 63(16):1697–1741.
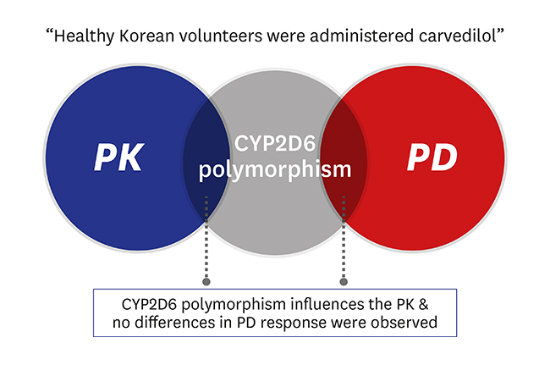
3. Zhou HH, Wood AJ. Stereoselective disposition of carvedilol is determined by CYP2D6. Clin Pharmacol Ther. 1995; 57(5):518–524.

4. Bartsch W, Sponer G, Strein K, Müller-Beckmann B, Kling L, Böhm E, et al. Pharmacological characteristics of the stereoisomers of carvedilol. Eur J Clin Pharmacol. 1990; 38:Suppl 2. S104–S107.

5. Neugebauer G, Akpan W, Kaufmann B, Reiff K. Stereoselective disposition of carvedilol in man after intravenous and oral administration of the racemic compound. Eur J Clin Pharmacol. 1990; 38:Suppl 2. S108–S111.

6. Neugebauer G, Akpan W, von Möllendorff E, Neubert P, Reiff K. Pharmacokinetics and disposition of carvedilol in humans. J Cardiovasc Pharmacol. 1987; 10:Suppl 11. S85–S88.

7. Oldham HG, Clarke SE. In vitro identification of the human cytochrome P450 enzymes involved in the metabolism of R(+)- and S(−)-carvedilol. Drug Metab Dispos. 1997; 25(8):970–977.
8. Gehr TW, Tenero DM, Boyle DA, Qian Y, Sica DA, Shusterman NH. The pharmacokinetics of carvedilol and its metabolites after single and multiple dose oral administration in patients with hypertension and renal insufficiency. Eur J Clin Pharmacol. 1999; 55(4):269–277.

9. Honda M, Nozawa T, Igarashi N, Inoue H, Arakawa R, Ogura Y, et al. Effect of CYP2D6*10 on the pharmacokinetics of R- and S-carvedilol in healthy Japanese volunteers. Biol Pharm Bull. 2005; 28(8):1476–1479.
10. Saito M, Kawana J, Ohno T, Hanada K, Kaneko M, Mihara K, et al. Population pharmacokinetics of R- and S-carvedilol in Japanese patients with chronic heart failure. Biol Pharm Bull. 2010; 33(8):1378–1384.

11. Lee SY, Sohn KM, Ryu JY, Yoon YR, Shin JG, Kim JW. Sequence-based CYP2D6 genotyping in the Korean population. Ther Drug Monit. 2006; 28(3):382–387.

12. Ghahramani P, Lennard MS. Quantitative analysis of amitriptyline and nortriptyline in human plasma and liver microsomal preparations by high-performance liquid chromatography. J Chromatogr B Biomed Appl. 1996; 685(2):307–313.

13. Taguchi M, Nozawa T, Mizumaki K, Inoue H, Tahara K, Takesono C, et al. Nonlinear mixed effects model analysis of the pharmacokinetics of metoprolol in routinely treated Japanese patients. Biol Pharm Bull. 2004; 27(10):1642–1648.

14. Huang J, Chuang SK, Cheng CL, Lai ML. Pharmacokinetics of metoprolol enantiomers in Chinese subjects of major CYP2D6 genotypes. Clin Pharmacol Ther. 1999; 65(4):402–407.
15. Nishida Y, Fukuda T, Yamamoto I, Azuma J. CYP2D6 genotypes in a Japanese population: low frequencies of CYP2D6 gene duplication but high frequency of CYP2D6*10. Pharmacogenetics. 2000; 10(6):567–570.
16. Giessmann T, Modess C, Hecker U, Zschiesche M, Dazert P, Kunert-Keil C, et al. CYP2D6 genotype and induction of intestinal drug transporters by rifampin predict presystemic clearance of carvedilol in healthy subjects. Clin Pharmacol Ther. 2004; 75(3):213–222.

17. Baudhuin LM, Miller WL, Train L, Bryant S, Hartman KA, Phelps M, et al. Relation of ADRB1, CYP2D6, and UGT1A1 polymorphisms with dose of, and response to, carvedilol or metoprolol therapy in patients with chronic heart failure. Am J Cardiol. 2010; 106(3):402–408.

18. Lymperopoulos A, McCrink KA, Brill A. Impact of CYP2D6 genetic variation on the response of the cardiovascular patient to carvedilol and metoprolol. Curr Drug Metab. 2015; 17(1):30–36.

19. Bradford LD. CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics. 2002; 3(2):229–243.

20. Cleaveland CR, Rangno RE, Shand DG. A standardized isoproterenol sensitivity test. The effects of sinus arrhythmia, atropine, and propranolol. Arch Intern Med. 1972; 130(1):47–52.

21. Tenero D, Boike S, Boyle D, Ilson B, Fesniak HF, Brozena S, et al. Steady-state pharmacokinetics of carvedilol and its enantiomers in patients with congestive heart failure. J Clin Pharmacol. 2000; 40(8):844–853.

22. Morgan T. Clinical pharmacokinetics and pharmacodynamics of carvedilol. Clin Pharmacokinet. 1994; 26(5):335–346.

23. Graff DW, Williamson KM, Pieper JA, Carson SW, Adams KF Jr, Cascio WE, et al. Effect of fluoxetine on carvedilol pharmacokinetics, CYP2D6 activity, and autonomic balance in heart failure patients. J Clin Pharmacol. 2001; 41(1):97–106.

24. Sehrt D, Meineke I, Tzvetkov M, Gültepe S, Brockmöller J. Carvedilol pharmacokinetics and pharmacodynamics in relation to CYP2D6 and ADRB pharmacogenetics. Pharmacogenomics. 2011; 12(6):783–795.








 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download