INTRODUCTION
A choledochal cyst is a rare benign disease of the biliary tract.
1 Almost 80% of cases are diagnosed in the first decade of life, and this disease is four times more common in women. This disease is also known to be more prevalent in Asian countries.
234 The choledochal cyst was first described by Vater and Ezler in 1723 and classified by Todani in 1977 in accordance with its anatomical location and morphology.
5
Although choledochal cysts are classified as benign, malignant transformation, cholangitis, pancreatitis and other complications may occur if they are not treated.
6 Surgical resection is the standard treatment method because a malignant transformation rate of 10–30% is possible.
78910 The standard surgical procedure is a complete excision of the cyst with Roux-en-Y hepaticojejunostomy anastomosis and laparoscopic surgery has been increasingly used since it was first described by Farello et al.
11 in 1995. This is still a challenging way to perform a hepaticojejunostomy due to the small diameter of the bile duct and the possibility of bile leak or stricture.
As robotic surgery has continued to develop, it has become possible to perform complex minimal access procedures using these systems. Robotic surgical systems can overcome the shortcomings of laparoscopic surgery. By providing a three-dimensional view, magnification of the area in question, articulated instrumentation and an increased freedom of movement of the surgical instruments.
1213 Moreover, robotic systems are ergonomically better for the surgeon. Also, since choledochal cysts are common in young women,
1415 the improved cosmetic outcomes when using robotic equipment are desirable and have led to these surgeries becoming more widespread to treat this disease.
Despite many reports on robotic procedures for hepatectomy and pancreatic surgery, there have not been many previous studies of the use of robotic-assisted excision for choledochal cysts in adults. We have used laparoscopic surgery at our institute since 2009 to treat these cysts but started to perform robotic surgery for these cases from January 2014. The aims of our current study were to evaluate the safety and feasibility of using robotic procedures to treat a choledochal cyst, and to compare the robotic approach with our early and late experiences with the laparoscopic procedure.
Go to :

MATERIALS AND METHODS
Patient selection
We try in principle at our institute to apply a minimally invasive approach to treating a choledochal cyst if there is no suspicion of biliary tract malignancy. We here performed a retrospective analysis of adult patients (≥18 years) who underwent a robotic and laparoscopic procedure for cyst excision and Roux-en-Y hepaticojejunostomy at our hospital, Asan Medical center, Seoul, Korea, between January 2014 and December 2017. We received appropriate informed consent from all patients and we received IRB approval.
We previously reported in 2012 our initial experiences with the laparoscopic approach to treating a choledochal cyst in adults.
16 Since that time, a large number of laparoscopically-based pancreaticoduodenectomy and choledochal cyst operations have been conducted in our center and the technical skill and knowledge of these procedures has therefore developed and evolved. In our study, we divided our choledochal cyst patients into 3 treatment groups: Robotic (Group 1), late laparoscopic (Group 2), and early laparoscopic (Group 3) cyst excision with hepaticojejunostomy.
According to surgeon's preference and status of patient's private insurance, the approach choice of robotic or laparoscopic procedure was determined. There were no hybrid procedures, which mix the laparoscopic and robotic procedure, among the Group 1 cases. The extent of cystic involvement, anomalous pancreatobiliary ductal union (APBDU), biliary stone or malignancy was evaluated through CT, MRCP or ERCP, and classified according to the Todani classification.
Robotic surgical technique
The surgical techniques used at out hospital for choledochal cyst excision are similar between the robotic and laparoscopic approaches, and our laparoscopic procedure has been fully described in a previous report that described early experience of laparoscopic surgery for choledochal cyst.
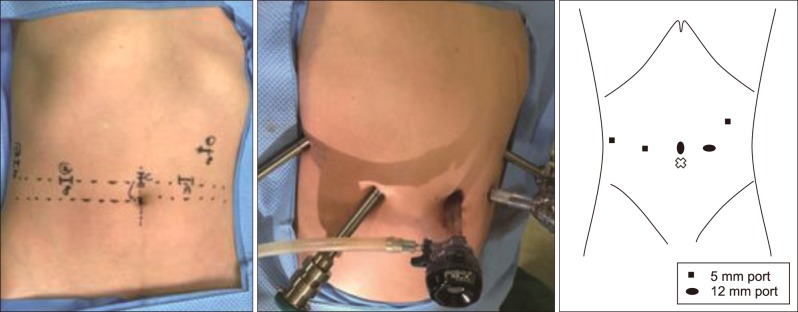
16 Briefly, the patients were placed in a reverse Trendelenburg position with the table tilted towards the left side, so that right side was elevated by about 15–20 degrees. In the robotic procedure, the da Vinci Robotic Surgical System (Si and Xi model, Intuitive Surgical, Sunnyvale, CA) was used. Five ports (4 robotic trocars including a 12-mm camera port , and 12-mm accessory port) were used and the port site is shown in the
Fig. 1. The abdominal cavity was inflated with CO
2 gas to a pressure of 10–12 mmHg to generate a pneumoperitoneum.
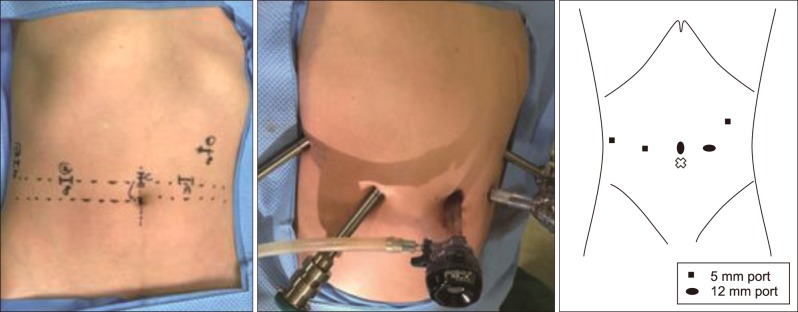 | Fig. 1Site and size of the trocars in robotic procedure.
|
After docking was completed, the dilated cyst was carefully separated from the hepatic artery and portal vein using a bipolar Maryland dissector on robotic arm 2 and monopolar hook or scissor and harmony scalpel on arm 1. Cadiere forceps on robotic arm 3 helped to create a better visual field to accomplish liver or duodenum traction. After circumferential dissection of the dilated choledochal cyst, the cyst was dissected down from the hepatic hilum to the intrapancreatic portion of the common bile duct until the transitional area with downward traction of duodenum (
Fig. 2A). The distal portion of the cyst was safely ligated and divided using hemo-loc or endo- stapler (
Fig. 2B). Using the distal stump of the cyst as a retractor, further upward dissection was performed until the hepatic ducts were sufficiently observed with identification of the right hepatic artery and main portal vein. The bile duct was then transected just below the hilum and the cyst and gallbladder were placed into a LapBag (Sejong Co., Paju, Korea). After dedocking, the specimen including the bile duct and gallbladder, was removed through extension of the periumbilical port site (about 2.5–3 cm). The jejunum at 40 cm distal to the Trieitz ligament was then exteriorized through the periumbilical port site and was divided using an EndoGIA linear stapler.
 | Fig. 2Operative photographs. (A) Robotic view of choledochal cyst. (B) Distal portion of the choledochal cyst being ligated and resected. (C) A hepaticojejunostomy was performed intracorporeally.
|
Jejunojejunostomy anastomosis was performed extracorporeally by manual suturing or an EndoGIA stapler. The da Vinci system continued to be used after the bowel was repositioned into the peritoneal cavity. A hepaticojejunostomy was performed intracorporeally using a needle holder on robotic arms 1 and 2 (
Fig. 2C). Interrupted sutures were made with 2 or 3 mm intervals using 5-0 PDS (Ethicon, Somerville, NJ) at the posterior wall. For the anterior wall, 5-0 Prolene (Ethicon) was used in the same manner. We preferred interrupted suturing at the posterior wall as this helps to for prevent anastomosis stricture, but we applied a continuous suture using 4-0 V-Loc (Covidien, Norwalk, CT) when the diameter of bile duct was greater than 10 mm or when it was decided that running suture was appropriate. After the hepaticojejunostomy was completed, a Jackson-Pratt drain was inserted through the port on robotic 3th arm and placed posteriorly to the hepaticojejunostomy.
Postoperative management and follow-up
Patients were commenced on water on postoperative day 1, followed by a soft diet on day 2. The Jackson-Pratt drain was removed on postoperative day 3 or 4 if no bile leak or intraabdominal complicated fluid was seen. At 2 weeks after discharge, patients visited the outpatients department and checked a liver function test and an evaluation for any complications. If there were no abnormal findings, the patients were followed up every 6 or 12 months at the discretion of the surgeon. In this study, the overall follow-up period ranged from 5 months to a maximum of 100 months.
Statistic analysis
The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to test the normality of the data in the three groups. One way ANOVA was applied to compare the differences between the three groups for factors that satisfy the normality. And the post-hoc analysis was perfomed through Tukey's HSD(honest significant difference) test for the operation time, which is the difference between groups. p-value of <0.05 was considered statistically significant.
On the other hand, the Kruskal-Wallis test was applied to compare the differences between the three groups for factors that don't satisfy the normality. Mann-Whitney test was used for the post-hoc analysis and statistical significance was considered when the p-value was less than 0.017 (=0.05/3) by Bonferroni's method. The data were analyzed using SPSS statistics (Version 21, IBM, USA).
Go to :

RESULTS
Clinical characteristics of patients
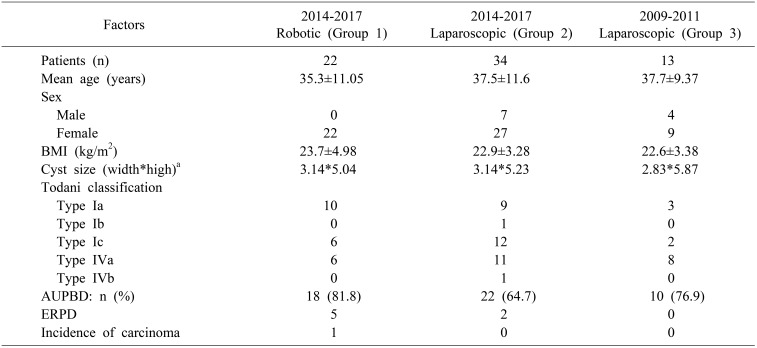
We compared 22 patients who underwent robotic surgery (Group 1) and 34 who underwent laparoscopic surgery (Group 2) from January 2014 to December 2017 for a choledochal cyst, in addition to 13 patients who underwent laparoscopic surgery from September 2009 to July 2011 for this same condition (Group 3). The characteristics of the patients included in the three groups are shown
Table 1.
Table 1
Patient demographics
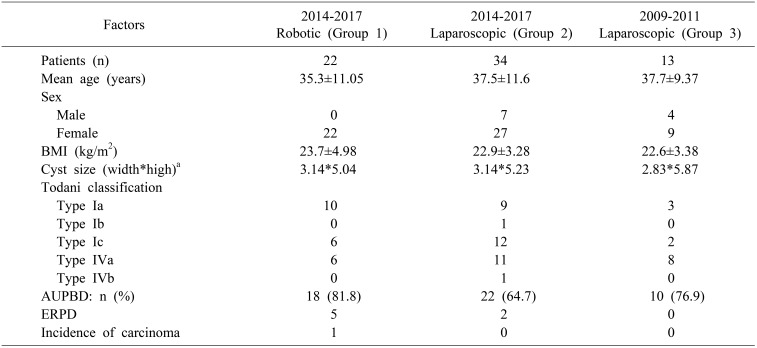

The mean age was 35.3±11.05 years in Group 1, 37.5±11.6 years in Group 2, and 37.7±9.37 years in Group 3. The ratio of males to females in the three groups was 0:22, 7:27, and 4:9, respectively. In all groups, there were more women than men.
The mean body mass index (BMI) was 23.7±4.98 kg/m2 in Group 1, 22.9±3.28 kg/m2 in Group 2 and 22.6±3.38 kg/m2 in Group 3.
The mean cyst size (width*high) was 3.14*5.04 cm2 in Group 1, 3.14*5.23 cm2 in Group2 and 2.83*5.87 cm2 in Group 3.
According to the Todani classification, the Group 1 robotic surgery patients included 10 type Ia cases, 6 type Ic cases, and 6 type IVa cases. Group 2 patients, which underwent laparoscopic surgery over the same period as the Group 1 robotic cases, included 9 type Ia cases, 1 type Ib case, 12 type Ic cases, 11 type IVa cases, and 1 type IVb case. The Group 3 patients that underwent laparoscopic surgery from September 2009 to July 2011 included 3 type Ia cases, 2 type Ic cases, and 8 type IVa cases.
As shown in
Table 1, more than 64% of the patients had AUPBD in all groups.
To prevent pancreatitis or pancreatic duct injury after surgery, the number of patients with a preoperative insertion of ERPD was 5 in Group 1 and 2 in Group 2 and none in Group 3.
Postoperatively, biopsy specimens showing GB cancer (stage I, pT1NxM0) were found only in the robotic group with no malignancies observed in the other groups.
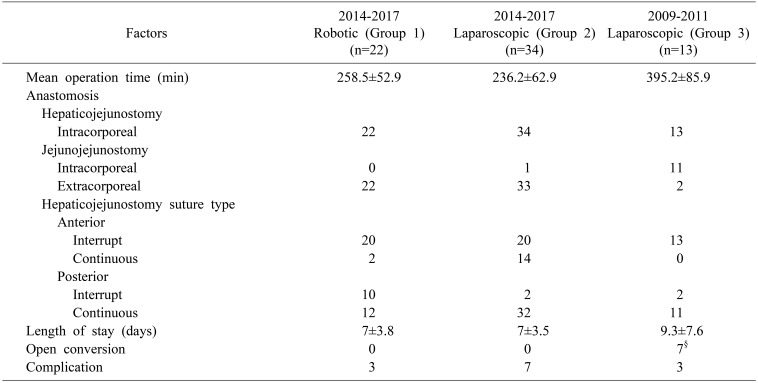
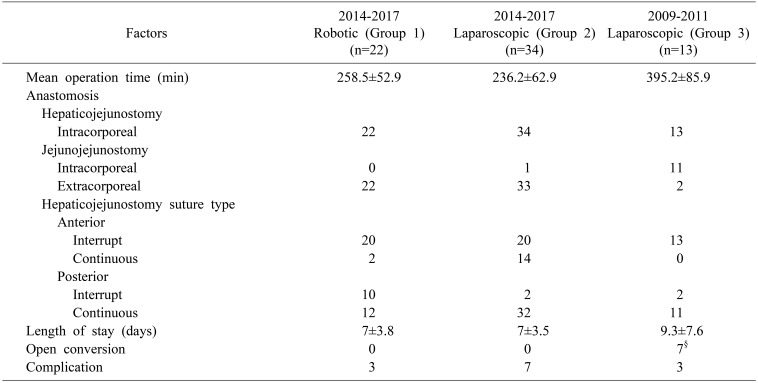
Clinical findings
The mean operative time were 258.5±52.9 min for robotic surgery (Group 1), 236.2±62.9 min for late laparoscopic surgery (Group 2), and 395.2±85.9 min for the initial laparoscopic surgery group (Group 3).
In all cases, a hepaticojejunostomy was performed intracorporeally. A jejunojejunostomy was performed intracorporeally in 11 of 13 cases and extracorporeally in only 2 cases in the initial laparoscopic surgery (Group 3).
However, for the procedures undertaken at out hospital over the last 4 years, extracorporeal anastomosis was performed in all cases in Group 1 and all but one case in Group 2.
The anterior wall suturing of hepaticojejunostomy was performed more interrupted suture than continuous suture in three groups, respectively. On the other hand, the posterior wall suturing was performed more continuous suture than interrupt suture in all groups.
The median hospital stay was 7 days for both Group 1 and 2, and 9.3 days for the initial laparoscopic surgery cases in Group 3. The mean of hospital stay was thus longer in the early group [
p=0.000 (Group 1 vs 3), 0.011 (Group 2 vs 3)]. There was no open conversion case in Group 1 and Group 2. In Group 3, 20 cases of laparoscopic procedure were performed originally, but open conversion was performed in 7 cases (
Table 2).
Table 2
Comparison of clinical outcomes by treatment group

Postoperative complications
Postoperative complications occurred in three patients who underwent robotic surgery (Group 1). This included a case of cholangitis which was resolved after conservative treatment, and bile leakage which was treated with PCD insertion.
The third case of an adverse event in Group 1 involved an umbilical herniation which was corrected by laparoscopic herniorrhaphy.
There were 7 cases of complications in the recent laparoscopic surgery patients in Group 2. These included a choledochojejunostomy site stricture & intrahepatic duct stone, choledochojejunostomy site stone due to the suture materials, jejunal branch bleeding, portal vein thrombus, acute pancreatitis, adhesive ileus and A-loop syndrome. The early laparoscopic surgery patients (Group 3) had complications in 3 cases. A hepaticojejunostomy site stricture occurred in 2 patients and a revision operation and biliary stent insertion were performed. Paralytic ileus was also observed in one case and these symptoms improved after conservative care. There were no mortality case in any of the three groups.
Go to :

DISCUSSION
A choledochal cyst is a rare disease that is usually found in children and is often observed in young women when diagnosed in adults.
5 The symptoms of this disease manifest as abdominal pain, a right upper quadrant mass and obstructive jaundice in the pediatric population, and abdominal pain and biliary or pancreatic symptoms in adults.
4 Although this disease is typically benign, surgical treatment should be considered as a priority because there is a low probability of malignancy. Long-term follow-up is therefore also needed after surgery.
17
Laparoscopic surgery to treat a choledochal cyst was first described by Farello et al.
11 in 1995, but more recently has been widely adopted and is now preferred over open surgery. Because most patients with a choledochal cyst are young women, laparoscopic surgery has become preferred to open surgery in terms of cosmetic outcomes as well as reduced pain and earlier recovery.
1415 It is generally advantageous to shorten the hospital stay after surgery and to have less postoperative pain. However, the adaptation of laparoscopic approaches to perform hepatobiliary surgery has been slow due to the technical complexities of these procedures which have led to considerable learning curve, even in experienced centers.
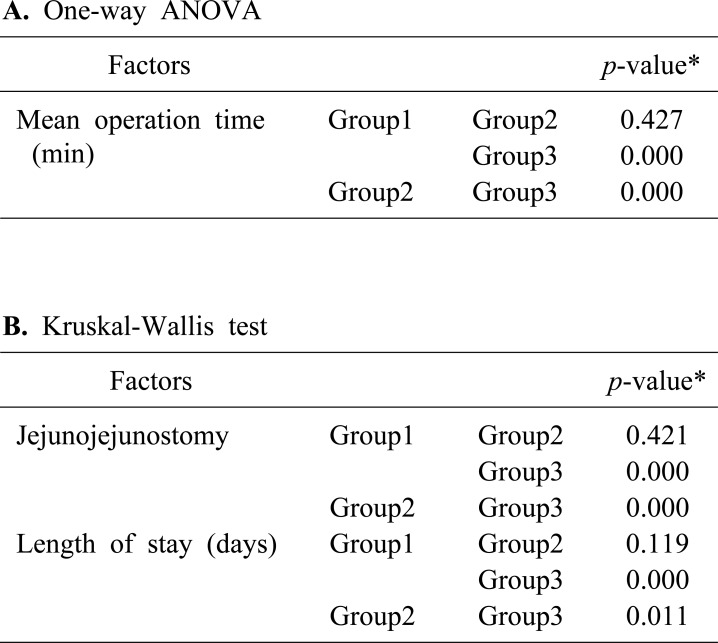
Laparoscopic procedures to treat choledochal cyst commenced in our hospital in 2009, and this method has undergone significant change and advanced since 2014. Initially, an intracorporeal jejunojejunostomy was performed in 11 out of 13 cases at our center and a total laparoscopic procedure without manual procedures was conducted in most cases. In our more recent laparoscopic surgeries for a choledochal cyst, extracorporeal jejunojejunostomy was performed in 33 out of 34 cases, which dramatically reduced the operation time from 395.2±85.9 minutes to 236.2±62.9 minutes [
p=0.000].
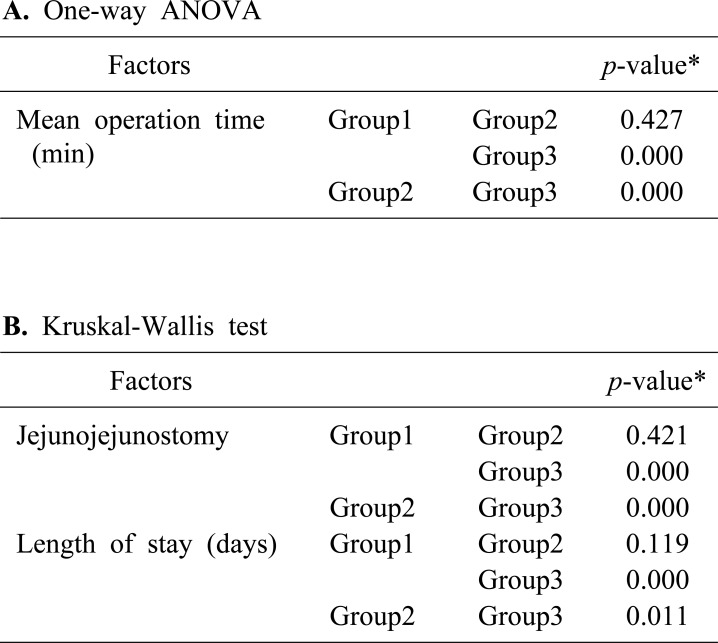
Table 3 show that there was a statistically difference in jejunojejunostomy anastomosis method between Group 1, 2 and Group 3 [
p=0.000 (Group 1 vs 3), 0.000 (Group 2 vs 3)]. Also, Group 1 (258.5±52.9 min) and Group 2 (236.2±62.9 min) were significantly shorter than Group 3 (395.2±85.9 min) in mean operation time [
p=0.000 (Group 1 vs 3), 0.000 (Group 2 vs 3)]. The hospital days were also reduced from 9.3 days to 7 days [
p=0.000 (Group 1 vs 3), 0.011 (Group 2 vs 3)].
Table 3
Statistical comparison of mean operation time in the three groups

There were two cases of anastomosis stricture among the early 13 cases, and also among the more recent 34 cases who underwent laparoscopic surgery for a choledochal cyst. Although there is no statistical significance until now, the problem of anastomosis was relatively less in the recent laparoscopic surgery patients (5.9%) compared with the early cases (15.4%). More than 180 laparoscopic pancreaticoduodenectomy procedures were performed in our center from 2009 to 2014 which has greatly enhanced the experience and skill levels among our surgeons with the dissection and anastomosis of the bile duct.
There are some noteworthy limitations with the use of laparoscopic instruments which include their rigidity and consequent reduction in the degree freedom. This is coupled with the fulcrum effect of laparoscopy and 2-dimensional view only.
1213 These drawbacks may contribute to the lack of popularity of this approach. The introduction of robotic surgical systems has overcome some of these hurdles. The principle advantages of robotic surgery are the magnified 3D imaging and the enhanced instrument control and dexterity.
18 The camera is mainly controlled by the console surgeon and has very stable vision. The robotic arms can provide intuitive manipulations with tremor filtration, motion scaling, and articulated wrists that enable a high freedom of movement.
1213 Improved ergonomics for the surgeons are also an important advantage of robotic systems which allow the surgeon to sit comfortably at the console and perform intricate dissection, and precise suturing techniques. These advantages of robotic procedures are particularly pertinent when the diameter of hilum duct is small or the level of the cyst is close upward to hilum, and intracorporeal suturing such as hepaticojejunostomy anastomosis is needed.
In our robotic procedure, Cardier forceps on the robotic 3rd arm are used to maintain traction of the liver and anterior bile duct wall during the hepaticojejunostomy, which facilitates stable movement and a better visual field. We have not experienced any open conversions or a need for reoperation when using this system. The surgical outcomes of the robotic series of choledochal cyst cases in our present study, in spite of the initial experience, were favorable in comparison with the early and late laparoscopic patients with this condition. The biliary tract-specific complication rates were similar between patients who underwent laparoscopic surgery and those who underwent robotic surgery. There were 2 cases of postoperative biliary leakage or stricture after laparoscopic surgery (5.8%) while only one case of this complication was observed after robotic surgery (4.5%). But, postoperative biliary leakage after a robotic procedure was mild and transient only, and no biliary strictures were observed after robotic excision of a choledochal cyst.
The operation time is an important practical issue for robotic procedures. The robot system and more recent laparoscopic procedure during the last 4 years for a choledochal cyst had operation times of 258.5±52.9 and 236.2±62.9 minutes, respectively. However, this extra 20 minutes required for the robotic procedure was not unfavorable considering the preparation time required for this approach such as docking.
Also, when the learning curve is taken into consideration, our initial series of robotic surgery patients have shown quite favorable results. We can expect that the operation times will be shortened for the robotic procedures in our hospital as more experience is gained with these surgeries.
This study had some limitations of note. First, it was retrospective investigation with inherent biases. Notably however, a large prospective study is not easy for diseases such as a choledochal cyst which are rare. Second, the number of robotic cases was relatively small. However, this was an initial series however and we would point to the fact that we have to our knowledge described the largest number of robotic cases in biliary and pancreatic surgery such as pancreaticoduodenectomy. Future multicenter studies with large patient populations and longer-term follow-ups are warranted to further evaluate the safety and feasibility of robotic surgery. Currently, robotic procedure is considerably more expensive than laparoscopic procedure. So cost-effectiveness of using a robotic system also should be evaluated.
A robot-assisted resection of a choledochal cyst with a Roux-en-y hepaticojejunostomy is a safe and feasible option with short-term results that are comparable to laparoscopic surgery. Compared to laparoscopic surgery, robot-assisted techniques also have distinct advantages such as better intracorporeal suturing and provision of a good 3D visual field.
It is likely that robotic surgery will soon become more widely adopted to complement the current limitations of conventional laparoscopic surgery.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download