Abstract
The feasibility of laparoscopic pancreaticoduodenectomy (LPD) in the treatment of pancreatic cancer is still disputed. However, advances in surgical technique and accumulating experience have led to the use of LPD with combined vascular resection and reconstruction as a safe and feasible procedure, especially in pancreatic cancer with major vascular involvement. A 64-year-old woman presented with obstructive jaundice secondary to pancreatic head cancer. Contrast abdominopelvic computed tomography revealed a pancreatic head tumor measuring approximately 22 mm in diameter that was abutting the first jejunal branch of the superior mesenteric vein at an angle of <180°. The patient underwent LPD, which failed to resect the pancreatic head tumor invading the superior mesenteric vein. Consequently, segmental resection of the confluence of the superior mesenteric vein, splenic vein, and portal vein (SMV/SV/PV) was completely performed in laparoscopic approach without complication. The patient recovered without any event and was discharged on postoperative day 9. LPD combined with vascular resection and reconstruction is feasible in cases involving major blood vessels. Further surgical expertise and education are required before LPD can be used as a standard procedure.
No randomized controlled studies have compared the open and laparoscopic approaches to distal pancreatectomy. Nonetheless, with advances in laparoscopic techniques and increased surgical expertise, laparoscopic distal pancreatectomy is considered safe and effective in treating benign and low-grade malignant tumors of the pancreas.12 In fact, laparoscopic radical pancreatectomy is suggested as a technically feasible and oncologically safe intervention in well-selected cases of left-sided pancreatic cancer.345
Conversely, the use of laparoscopic pancreaticoduodenectomy (LPD) remains controversial, especially in the treatment of pancreatic cancer, where it can increase the risk of cholangitis and pancreatitis, interfering with efforts to obtain a margin-negative resection. In addition, pancreatic head cancer carries a risk of unexpected major vascular involvement. In particular, the superior mesenteric vein (SMV), portal vein (PV), or confluence of the SMV, splenic vein (SV), and PV may be involved, warranting surgery for combined vascular resection and appropriate vascular reconstruction.678910
However, few studies have reported the technical and oncological feasibility of LPD combined with venous vascular resection.11121314151617 In the current report, we present the case of a patient with pancreatic head cancer who underwent successful LPD with segmental resection of the SMV–SV–PV confluence, resulting in negative surgical margins.
A 64-year-old woman presented with general weakness, poor oral intake, and jaundice. The patient had a history of hypertension and a recent diagnosis of diabetes. She also reported weight loss (−8 kg) during the previous 3 months.
The physical examination showed no abnormal findings other than those mentioned above. Her body mass index was 22.48 kg/m2, and her initial laboratory findings are summarized in Table 1.
The woman showed high levels of serum total bilirubin (6.9 mg/dL), alkaline phosphatase (1,090 IU/L), and γ-glutamyl transferase (1,079 IU/L) suggesting obstructive jaundice. Preoperative imaging (Fig. 1) revealed a pancreatic head mass and secondary dilatation of the intrahepatic and extrahepatic bile ducts, suggesting pancreatic head cancer. The finding suggested that the tumor was a resectable pancreatic cancer with no distant metastasis. To resolve obstructive jaundice, the patient underwent endoscopic retrograde cholangiopancreatoscopy with biliary drainage.
The woman underwent LPD on April 4, 2018. As a standard procedure, three 5-mm trocars and three 12-mm trocars were used in this procedure (Fig. 2). Laparoscopy confirmed the absence of clinical evidence associated with peritoneal seeding or liver metastasis, and the gastrocolic ligament was divided by dissection. The colonic mesentery was detached from the pancreatico-duodenal unit and right gastroepiploic vessels. The right gastric vessels were dissected and ligated. The duodenum was divided using an endo-GIATM stapler. The pancreatic neck was dissected and encircled using a nylon tape. The common bile duct was dissected, isolated, and divided, followed by cholecystectomy.
Next, the soft tissue around the left side of the celiac axis, common hepatic artery, and hepatoduodenal ligament was dissected. The proximal jejunum was divided using the endo-GIA stapler approximately 20 cm distal to the Treitz ligament. The proximal jejunum was passed under the mesenteric root into the patient's right side. At this point, it was found that specific parts of the SMV could not be dissected away from the pancreatic head area. Therefore, the neck of pancreas was divided using monopolar cautery. The SV was isolated, ligated, and divided, and laparoscopic bulldog clamps were applied to the proximal and distal parts of the SMV–PV system (Fig. 3A). The venous vascular structure was divided, and the tumor was excised. Using a 5-0 monofilament, vascular reconstruction was performed in an end-to-end fashion (Fig. 3B, 3C).
Subsequently, pancreaticojejunostomy (duct-to-mucosa, all interrupted, two-layer, and short stent) and hepaticojejunostomy (posterior continuous, anterior all interrupted, and single layer) were completed laparoscopically. The specimen was placed into an endo-pouch, which was then removed through a small periumbilical extension of the wound through which manual duodenojejunostomy was performed.
Bilateral, two-armed, closed suction drains were inserted around the surgical bed. All trocar insertion sites were repaired using a skin stapler. The entire procedure lasted 480 min, including 39 min of vascular clamp time. Intraoperative blood loss was estimated at 500 ml, without the need for intraoperative transfusion.
The patient's recovery was uneventful, without any pancreatic fistula. Her surgical drains were removed on postoperative day 6. A follow-up computed tomography was performed on postoperative day 7 with no PV thrombosis, stricture, or other surgical complications (Fig. 3D). The patient was discharged 9 days after the operation without any complications.
Pathological diagnosis confirmed the tumor as a moderately differentiated T2 ductal adenocarcinoma measuring 3.5×1.9 cm in size, involving the common bile duct. No lymphovascular invasion was found; however, perineural invasion was noted. A total of 18 lymph nodes were retrieved with no lymph node metastasis (N0, Stage IB). All the resection margins, including the retroperitoneal margin, were negative.
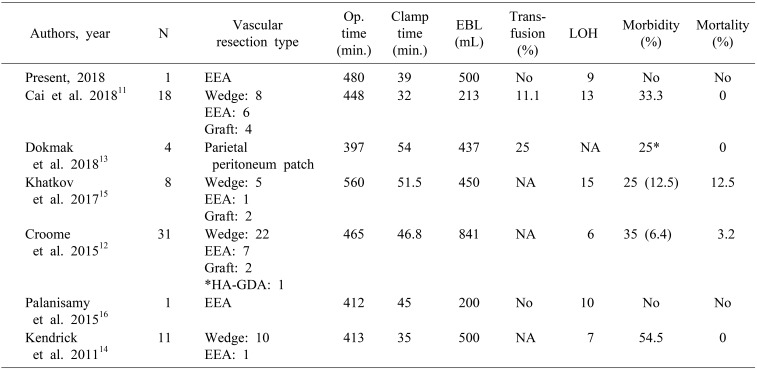
Recently, several studies have reported the feasibility and safety of LPD (Table 2). Indeed, a recent meta-analysis found that LPD has several advantages compared with open pancreaticoduodenectomy (OPD), such as reduced intraoperative bleeding, shorter hospital stay after surgery, fewer complications, and shorter time to postoperative chemotherapy.181920212223
Despite advances and increased expertise with laparoscopic surgical techniques such as LPD combined with major vascular resection, only a few studies have addressed this topic. Nonetheless, all of these studies reported that LPD is feasible and safe if conducted by an experienced surgeon, even with major vascular resection. To date, laparoscopic surgery has not usually been attempted in cases involving major blood vessels. However, the results of LPD to date have been comparable to, or better than, those of OPD. In particular, the largest study, which was published by Croome et al.,12 reported the results of LPD combined with major vascular resection. They successfully demonstrated not only the feasibility and safety of LPD with major vascular resection, but also its association with similar perioperative surgical outcomes such as OPD with major vascular resection.
However, these encouraging reports must be carefully interpreted, because technical feasibility may not be an indication for surgery. Instead, indications should be general clinical conditions that are amenable to standardized, well-documented, and validated surgical management with acceptable morbidity and mortality. In this regard, acute cholecystitis and empyema of the gallbladder may illustrate the concept of surgical indication in the laparoscopic era. In the past, acute cholecystitis was regarded as a contraindication for laparoscopic cholecystectomy.2425 However, with accumulating experience and reports showing the technical feasibility, effectiveness, and safety of the laparoscopic approach, the disease finally became an accepted surgical indication for laparoscopic cholecystectomy.26272829
In the case of LPD, the safety of the procedure is still unclear.2130 In addition, publication bias must be considered in that researchers tend to report selected cases with favorable results, but not worse perioperative outcomes that are less likely to be accepted for publication. Acceptance of LPD with combined major vascular resection as a standard technique requires additional reports and assessments. In this regard, Table 2 shows that only rare cases have been reported from specialized centers. Ideally, a randomized, controlled study is desirable. However, few surgeons are currently proficient in this technique, and its safety.
Therefore, periampullary malignant pathology cannot be regarded as an indication for LPD combined with major vascular resection. It is only indicated in selected cases and when conducted by surgeons specializing in both minimally invasive and open pancreaticoduodenectomy. Surgeons need to be able to rapidly compensate for any unexpected intraoperative event or perioperative complication. To begin with, a detailed and systematic surgical educational program for LPD must be established to ensure the safe introduction of LPD for beginning surgeons.
In summary, we have reported a successful case of LPD with segmental resection of the SMV–SV–PV confluence and end-to-end anastomosis to treat pancreatic head cancer. This case demonstrates the technical and oncological feasibility of this advanced laparoscopic approach to pancreatic cancer. However, patient selection criteria, surgical qualifications, and educational strategies need to be established before this surgical procedure can become the standard of care, to ensure patient safety.
References
1. Mehrabi A, Hafezi M, Arvin J, Esmaeilzadeh M, Garoussi C, Emami G, et al. A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: it's time to randomize. Surgery. 2015; 157:45–55. PMID: 25482464.
2. Yan JF, Kuang TT, Ji DY, Xu XW, Wang DS, Zhang RC, et al. Laparoscopic versus open distal pancreatectomy for benign or premalignant pancreatic neoplasms: a two-center comparative study. J Zhejiang Univ Sci B. 2015; 16:573–579. PMID: 26160714.

3. Nakamura M, Nakashima H. Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci. 2013; 20:421–428. PMID: 23224732.

4. Pericleous S, Middleton N, McKay SC, Bowers KA, Hutchins RR. Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas. 2012; 41:993–1000. PMID: 22836858.
5. Sui CJ, Li B, Yang JM, Wang SJ, Zhou YM. Laparoscopic versus open distal pancreatectomy: a meta-analysis. Asian J Surg. 2012; 35:1–8. PMID: 22726557.

6. Bachellier P, Nakano H, Oussoultzoglou PD, Weber JC, Boudjema K, Wolf PD, et al. Is pancreaticoduodenectomy with mesentericoportal venous resection safe and worthwhile? Am J Surg. 2001; 182:120–129. PMID: 11574081.

7. Chua TC, Saxena A. Extended pancreaticoduodenectomy with vascular resection for pancreatic cancer: a systematic review. J Gastrointest Surg. 2010; 14:1442–1452. PMID: 20379794.

8. Menon VG, Puri VC, Annamalai AA, Tuli R, Nissen NN. Outcomes of vascular resection in pancreaticoduodenectomy: single-surgeon experience. Am Surg. 2013; 79:1064–1067. PMID: 24160800.

9. Siriwardana HP, Siriwardena AK. Systematic review of outcome of synchronous portal-superior mesenteric vein resection during pancreatectomy for cancer. Br J Surg. 2006; 93:662–673. PMID: 16703621.

10. Yu XZ, Li J, Fu DL, Di Y, Yang F, Hao SJ, et al. Benefit from synchronous portal-superior mesenteric vein resection during pancreaticoduodenectomy for cancer: a meta-analysis. Eur J Surg Oncol. 2014; 40:371–378. PMID: 24560302.

11. Cai Y, Gao P, Li Y, Wang X, Peng B. Laparoscopic pancreaticoduodenectomy with major venous resection and reconstruction: anterior superior mesenteric artery first approach. Surg Endosc. 2018; 32:4209–4215. PMID: 29602996.

12. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg. 2015; 19:189–194. PMID: 25274069.

13. Dokmak S, Aussilhou B, Calmels M, Maghrebi H, Ftériche FS, Soubrane O, et al. Laparoscopic pancreaticoduodenectomy with reconstruction of the mesentericoportal vein with the parietal peritoneum and the falciform ligament. Surg Endosc. 2018; 32:3256–3261. PMID: 29349542.

14. Kendrick ML, Sclabas GM. Major venous resection during total laparoscopic pancreaticoduodenectomy. HPB (Oxford). 2011; 13:454–458. PMID: 21689228.

15. Khatkov IE, Izrailov RE, Khisamov AA, Tyutyunnik PS, Fingerhut A. Superior mesenteric-portal vein resection during laparoscopic pancreatoduodenectomy. Surg Endosc. 2017; 31:1488–1495. PMID: 27444832.

16. Palanisamy S, Deuri B, Naidu SB, Vaiyapurigoundar Palanisamy N, Natesan AV, Palanivelu PR, et al. Major venous resection and reconstruction using a minimally invasive approach during laparoscopic pancreaticoduodenectomy: one step forward. Asian J Endosc Surg. 2015; 8:468–472. PMID: 26708588.

17. Awad ZT. Totally laparoscopic pancreaticoduodenectomy for pancreatic head cancer with involvement of the superior mesenteric vein-portal vein confluence. Ann Surg Oncol. 2014; 21:3439. PMID: 24841345.

18. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 2014; 260:633–638. PMID: 25203880.
19. Mesleh MG, Stauffer JA, Bowers SP, Asbun HJ. Cost analysis of open and laparoscopic pancreaticoduodenectomy: a single institution comparison. Surg Endosc. 2013; 27:4518–4523. PMID: 23943116.

20. Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg. 2012; 215:810–819. PMID: 22999327.

21. Boggi U, Amorese G, Vistoli F, Caniglia F, De Lio N, Perrone V, et al. Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc. 2015; 29:9–23. PMID: 25125092.

22. Hakeem AR, Verbeke CS, Cairns A, Aldouri A, Smith AM, Menon KV. A matched-pair analysis of laparoscopic versus open pancreaticoduodenectomy: oncological outcomes using Leeds Pathology Protocol. Hepatobiliary Pancreat Dis Int. 2014; 13:435–441. PMID: 25100130.

23. Langan RC, Graham JA, Chin AB, Rubinstein AJ, Oza K, Nusbaum JA, et al. Laparoscopic-assisted versus open pancreaticoduodenectomy: early favorable physical quality-of-life measures. Surgery. 2014; 156:379–384. PMID: 24680859.

24. Frazee RC, Roberts JW, Symmonds R, Snyder SK, Hendricks J, Smith R, et al. What are the contraindications for laparoscopic cholecystectomy? Am J Surg. 1992; 164:491–494. PMID: 1443375.

25. Fontes PR, Nectoux M, Eilers RJ, Chem EM, Riedner CE. Is acute cholecystitis a contraindication for laparoscopic cholecystectomy? Int Surg. 1998; 83:28–30. PMID: 9706512.
26. Eldar S, Sabo E, Nash E, Abrahamson J, Matter I. Laparoscopic cholecystectomy for acute cholecystitis: prospective trial. World J Surg. 1997; 21:540–545. PMID: 9204745.

27. Cirocchi R, Del Sol A, Morelli U, Cattorini L, La Mura F, Napolitano V, et al. [Laparoscopic cholecystectomy for acute cholecystitis]. G Chir. 2008; 29:305–311. Italian. PMID: 18544271.
28. Stanišić V, Bakić M, Magdelinić M, Kolašinac H, Babić I. [Laparoscopic cholecystectomy of acute cholecystitis]. Med Pregl. 2010; 63:404–408. Croatian. PMID: 21186555.

29. Shinke G, Noda T, Hatano H, Shimizu J, Hirota M, Takata A, et al. Feasibility and safety of urgent laparoscopic cholecystectomy for acute cholecystitis after 4 days from symptom onset. J Gastrointest Surg. 2015; 19:1787–1793. PMID: 26129654.
30. Liao CH, Wu YT, Liu YY, Wang SY, Kang SC, Yeh CN, et al. Systemic review of the feasibility and advantage of minimally invasive pancreaticoduodenectomy. World J Surg. 2016; 40:1218–1225. PMID: 26830906.

Fig. 1
Preoperative imaging. (A) Magnetic resonance cholangiopancreatoscopy revealed a pancreatic head mass leading to the bile duct, as well as pancreatic duct dilatation. (B) Contrast abdominopelvic computed tomography revealed a pancreatic head tumor measuring around 22 mm in diameter that was abutting the 1st (jejunal) branch of the superior mesenteric vein at an angle of <180°. (C) Endoscopic ultrasonography revealed a solid mass in the pancreatic head measuring 26.1 mm in diameter, with a suspicious duodenal wall invasion. (D) Positron-emission tomography–computed tomography demonstrated significant fluorodeoxyglucose uptake in the pancreatic head lesion, suggesting malignancy (D).
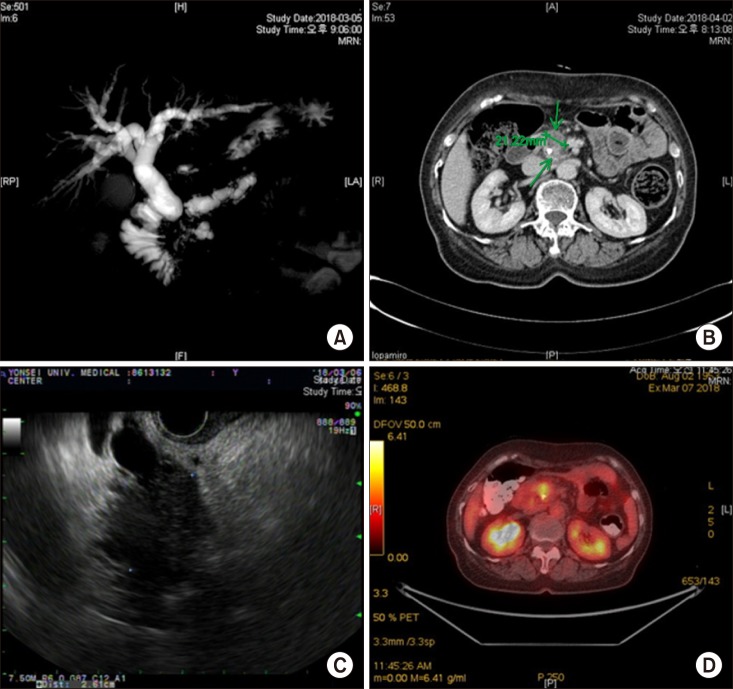
Fig. 3
Intraoperative and postoperative findings. Ao, aorta; BD, bile duct; CHA, common hepatic artery; LRV, left renal vein; PV, portal vein; RRA, right renal artery; SMA, superior mesenteric artery; SMV, superior mesenteric vein. Labels: pancreatic duct (short white arrow); anastomosis site (multiple small white arrow); vascular patency confirmed (large white arrow head).
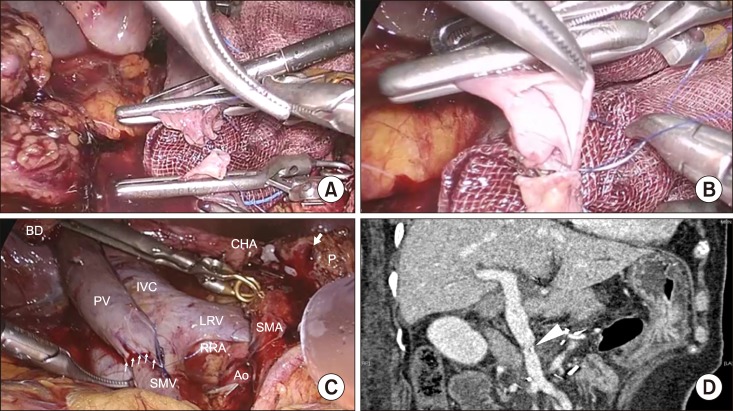
Table 1
Initial preoperative laboratory findings
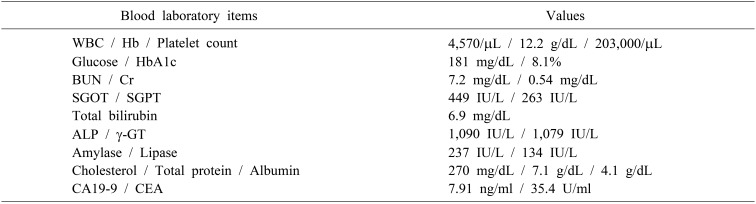
WBC, white blood cells; Hb, hemoglobin; HbA1c, glycated hemoglobin; BUN, blood urea nitrogen; Cr, creatinine; SGOT, serum glutamic oxaloacetic transaminase; SGPT, serum glutamic pyruvic transaminase; ALP, alkaline phosphatase; γ-GT, γ-glutamyl transferase; CA 19-9, cancerantigen 19-9; CEA, carcinoembryonic antigen




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download