Abstract
Backgrounds/Aims
Early laparoscopic cholecystectomy is considered as the standard treatment of acute cholecystitis. However, whether this procedure is desirable in elderly patients with acute cholecystitis is not clearly elucidated. In this study, we aimed to evaluate the effects of thorough preoperative assessment and consultation for complications on clinical outcomes in elderly patients over 65 and over 80 years.
Methods
We retrospectively analyzed 205 patients who were diagnosed with acute cholecystitis between January 2010 and April 2018. The patients were assigned to three groups: group A (aged <65 years), group B, (aged between 65 and 79 years), and group C (aged >79 years). Laparoscopic cholecystectomy was performed after preoperative evaluation, such as echocardiography, pulmonary function test, and consultation about past history.
Results
Significant differences were not found in the complication rate among the age groups. Open conversion was required in eight of the 114 patients in group A, seven of the 70 patients in group B, and one of the 21 patients in group C. However, no statistical significance was found. Moreover, no difference was noted in the start of the meal and the period from surgery to last visit, but hospital stay after surgery was longer in groups b and c.
Go to : 
Increasing elderly population due to development of health care and improvement of nutrition is a worldwide phenomenon. The prevalence of gallstones has been increasing with age, affecting up to 30% of individuals over 60 years and up to 80% of individuals over 90 years.12 Thus, the number of acute cholecystitis (AC) in the elderly is increasing.
In young and otherwise healthy patients, early laparoscopic cholecystectomy (LC) is considered as the standard treatment of AC.345678 However, whether early LC is desirable in elderly patients with AC remains controversial. LC for elderly patients with AC represents a complex challenge due to the increased potential risk of perioperative morbidity and mortality.9 Elderly patients may have many comorbid conditions, which are associated with increased postoperative LC complications.10
Many studies have demonstrated the advantages of LC for elderly patients, comparing perioperative outcomes of early cholecystectomy in elderly and younger patients. However, several of them showed no difference in postoperative morbidity or mortality.111213 A recent meta-analysis of systematic review has shown that careful selection of elderly patients contributes to a better perioperative outcome,14 but there is no uniform guidance on selection or preoperative assessment. In particular, few studies have investigated LC in patients older than 80 years,1516 despite the increasing prevalence.
In this study, we reviewed our experience in the management of acute AC retrospectively. We aimed to evaluate the effects of our preoperative management on clinical outcomes for patients over 65 and over 80.
Go to : 
This study was approved by the ethics committee of the National Medical Center. We performed a retrospective analysis of 207 patients who underwent LC for AC who were admitted to the National Medical Center in Korea between January 2010 and April 2018. A total of 205 patients were eligible for review. Two patients were excluded because of missing data. Patients who underwent LC were divided into three groups based on their age: group A (14 patients, <65 years), group B (70 patients, between 65 and 79 years), and group C (21 patients, >80 years).
Patients who were diagnosed with AC, gallbladder empyema, and gangrenous cholecystitis based on Tokyo Guidelines1718 and underwent LC were included in this study. By contrast, those diagnosed with gallbladder cancer, gallbladder polyps, and adenomyomatosis were excluded. Interpretation of CT scans was performed by experienced radiologists.
All surgeries were performed with the conventional 4-hole LC method. Open conversion was done in case of severe adhesion, uncontrolled bleeding, common bile duct injury, and Mirrizzi syndrome. Percutaneous transhepatic gallbladder drainage (PTGBD) was performed under local anesthesia using ultrasonography by an interventional radiologist.
Each patient was preoperatively evaluated; blood chemistry, electrocardiogram, and plain chest radiograph were obtained. Echocardiographic examination was performed on patients with diabetes, high blood pressure more than 5 years, and aged over 65 years. Pulmonary function test was carried out in patients over 65 years and with pulmonary complications. We consulted a physician about preoperative management for patients with cardiovascular disease, chronic kidney disease on hemodialysis, cerebrovascular disease, and pulmonary disease.
PTGBD was actively performed on patients with distended gallbladder, leukocytosis, and fever as a bridging treatment. After stabilization of hemodynamic state and correction of comorbidities, each patient underwent LC promptly on selected time.
Age group was the major independent variable. Other patient characteristics were American Society of Anesthesiologists (ASA) score, PTGBD, endoscopic retrograde cholangiopancreatography, WBC count, total bilirubin, aspartate aminotransferase, alanine aminotransferase, past history, history of abdominal surgery, body mass index, albumin, and gender.
Past history was also investigated. Diabetes and high blood pressure were investigated as factors increasing postoperative complications. History of cardiovascular disease, chronic kidney disease on hemodialysis, chronic obstructive lung disease, cerebrovascular disease, and liver cirrhosis was collected as serious comorbidities. They were investigated as triggers for impaired hemodynamic condition. These covariants were obtained by chart review. For comparison of clinical outcome, information about conversion, common bile duct injury, intraoperative bleeding, postoperative ileus, bile leakage, postoperative bleeding, and wound infection was collected. Intraoperative bleeding was defined as bleeding that cannot be controlled by laparoscopic procedure.
SPSS version 18.0 (SPSS, Chicago, Illinois, USA) was used for statistical analysis. The chi-square test was performed for analysis of categorical variables and ANOVA for continuous variables. p-values <0.05 were considered statistically significant in this study.
Go to : 
The number of AC in the elderly is increasing due to aging.
Old age is often associated with complications and limited functional reserve. Some studies considered aged over 80 years as a separate group because of worst outcomes.151619 A study has shown that the need for transfusions and mechanical ventilation was more than three times in patients with LC aged over 80 years.19 This study was designed to assess the suitability of LC in old age, and patients aged over 80 years were considered as a separate group. Thus, the outcomes of LC in elderly patients could be viewed in detail by age group.
A total of 205 patients underwent LC for AC participated in this study. Group A included 114 patients younger than 65 years; group B, 70 patients aged between 65 and 79 years; and group C, 21 patients older than 80 years.
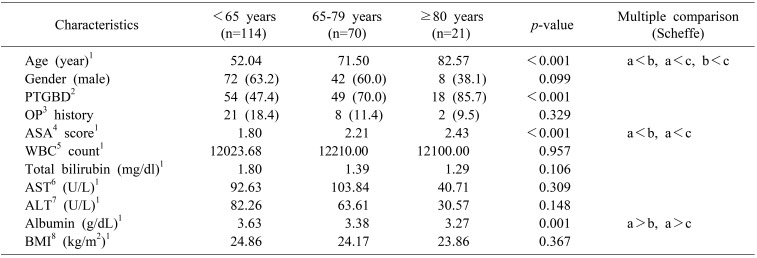
Table 1 shows the preoperative characteristics of the participants. Gender distribution was not significantly different among the three groups. For assessment of physical status, ASA score was obtained. ASA score was significantly higher in groups B and C than in group A. Albumin was significantly higher in group A than in groups B and C. Body mass index was not significantly different among the three groups.
Preoperative PTGBD was performed more frequently in old age groups. The chi-square test showed a significant difference among the groups. However, no significant difference was found in endoscopic retrograde cholangiopancreatography frequency. Laboratory values, WBC counts, aspartate aminotransferase, alanine aminotransferase, and serum total bilirubin levels were not significantly different among the groups. Intraabdominal surgery history was also not significantly different.
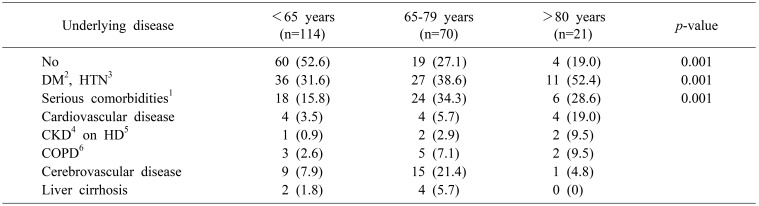
Table 2 shows the underlying disease of each group. There were significant differences in patient's underlying disease among the age groups. Diabetes and hypertension are more prevalent in group C. However, other diseases are more prevalent in group B. Eighty years old is an extremely old age; many patients with severe past history possibly die before the age of 80 years.
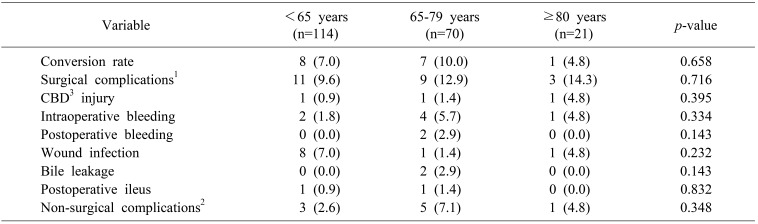
No significant difference was found in the complication rate among the groups (Table 3). Open conversion was required in 8 of the 114 patients in group A, 7 of the 70 patients in group B, and 1 of the 21 patients in group C. However, it was not statistically significant. Surgical complications showed no distributional difference among the different age groups. Eight cases of wound infection were found in group A, whereas one case each in groups B and C. Common bile duct injury, intraoperative bleeding, postoperative bleeding, and bile leakage were not statistically different among the groups. Non-surgical complication rate was 2.6% in group A, 7.1% in group B, and 4.8% in group C. These rates showed no apparent tendency according to age groups.
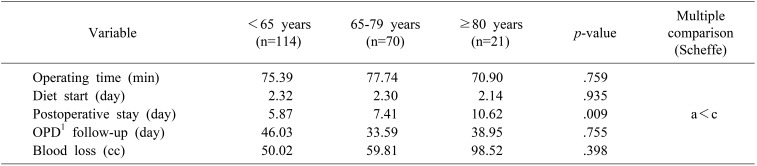
Variables for postoperative recovery are shown in Table 4. The number of days to start drinking water was about two days in each group. The period from surgery to last visit date also showed no difference among the groups. However, group C stayed longer in the hospital after surgery than group A. Operating time and blood loss were not significantly different among the three groups.
Go to : 
ASA score was significantly higher in groups B and C, and the underlying disease was also higher. These results indicate that the physical status of the elderly patients was worse. In groups B and C, more PTGBD was performed. In older patients, symptom presentation was delayed, and the severity of AC was high at admission.20 Older patients had more comorbidity, and several evaluations were performed before surgery. Thus, PTGBD was chosen more frequently as a bridging procedure.
No significant differences were found in conversion rate, surgical complications, and non-surgical complications among the age groups. Length of hospital stay showed difference among the age groups indicating that older people needed more time for postoperative recovery. No significant differences in clinical outcome were found in groups B and C owing to careful preoperative assessment and management.
In a retrospective study, complication rate and operating time are statistically significantly higher in age groups over 80 years.16 Other studies also supported poor outcomes in elderly patients who underwent LC.151921 However, assessment of preoperative patient conditions was not conducted in these studies. The poor clinical outcomes of older patients in existing studies are likely due to occult comorbidity. There is also a problem with delayed presentation of LC symptoms in the elderly.20 Our research concluded that surgery is safe if sufficient pre-operative assessment is carried out not only for people aged 65–79 years, but also for those over 80 years. A skilled laparoscopic surgeon performed each LC case by performing an elective surgery. This was possibly another cause of better operation results.
Previous studies showed that almost half of the patients undergoing PTGBD alone develop further episodes of cholecystitis within 3 years.2223 Percutaneous cholecystostomy has been utilized as a bridge to delayed LC even in patients with severe comorbidities or evidence for severe cholecystitis.2425 In this study, patients with PTGBD underwent LC after preoperative assessment and hemodynamic stabilization.
Whether the conversion rate of LC is rising in elderly patients is controversial. Sutcliffe et al.26 reported that old age is a risk factor for the conversion in LC. In our study, the conversion rate was not statistically different depending on the age group. The increase in PTGBD rate was observed as the cause of the decrease in conversion rate in old age. Ultrasound-guided percutaneous cholecystostomy has many benefits: it can identify gallstone in common bile duct and anatomical abnormality in biliary tree. We were able to lower the possibility of conversion by using this procedure. Several studies have reported lower conversion rates in LC after PTGBD.242728
Riall and Zhang20 and colleagues found significant morbidity and mortality in a cohort of patients who received non-operative treatment. There are limitations to such research, because surgeons choose the healthiest cohort of elderly patients with AC for LC.29 A recent cohort study reported better outcome for elderly patients with LC compared with patients who did not undergo surgery,30 but a possibility of selection bias still exists. In this study, instead of comparing the results according to whether or not surgery is performed on older patients, comparisons were made according to age. Surgery was performed after the assessment and correction of hidden comorbidities that prevent comparison. This helped in the assessment of the risk of old age itself, and the risks were not significant.
This study had several limitations. First, the numbers of patients aged 80 years was small (21 patients). Nevertheless, we found that adequate preoperative management was performed, and LC could be safe in patients aged over 80 years. Second, preoperative echocardiography and pulmonary function test can be costly depending on the medical environment and region. Therefore, it is important to consider including these tests in the insurance system in surgery of old age. If the results of the surgery are poor due to hidden complications, the overall cost of the medical system could increase. Third, patients who failed to perform the surgery were not included in the treatment results. A small number of elderly with underlying disease refused to undergo surgery. Fourth, our institution is a public hospital with many patients in the lower socioeconomic status. In these patients, low compliance and poor physiologic status may be observed, even under the age of 65 years. High preoperative severity and poor outcome of surgery may have been noted in younger patient population than those in other studies.
There were four options for treating AC in older patients. Based on existing findings, conservative treatment is considered inappropriate.1420 Almost half of the patients treated with PTGBD eventually undergo cholecystectomy.22 Thus, drainage alone is not the definitive treatment for AC. In young and otherwise healthy patients, early LC is the standard of choice. A recent meta-analysis of observational studies has shown that old age is associated with an increased risk of conversion.26 Another study proved that old age is independently associated with increased complications.31 In our practice, LC was performed when patients recovered to the point where the ASA score was less than four points. The treatment results of older patients in this study were not statistically significantly different compared with those of younger patients. In older patients and patients with underlying diseases, LC after PTGBD, with preoperative assessment may reduce the risk of surgery. A recent meta-analysis also supports this result.30
In conclusion, a thorough preoperative evaluation and correction of comorbidities are recommended in elderly AC patients with complications. This will help control the risk of LC for AC in old age.
Go to : 
References
1. Festi D, Dormi A, Capodicasa S, Staniscia T, Attili AF, Loria P, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008; 14:5282–5289. PMID: 18785280.

2. Lirussi F, Nassuato G, Passera D, Toso S, Zalunardo B, Monica F, et al. Gallstone disease in an elderly population: the Silea study. Eur J Gastroenterol Hepatol. 1999; 11:485–491. PMID: 10755250.
3. Papi C, Catarci M, D'Ambrosio L, Gili L, Koch M, Grassi GB, et al. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol. 2004; 99:147–155. PMID: 14687156.

4. Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev. 2013; (6):CD005440. PMID: 23813477.

5. Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010; 97:141–150. PMID: 20035546.

6. Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, Kipfmüller K, et al. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. 2013; 258:385–393. PMID: 24022431.
7. Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc. 2004; 18:1323–1327. PMID: 15803229.

8. Banz V, Gsponer T, Candinas D, Güller U. Population-based analysis of 4113 patients with acute cholecystitis: defining the optimal time-point for laparoscopic cholecystectomy. Ann Surg. 2011; 254:964–970. PMID: 21817893.
9. Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012; 380:1059–1065. PMID: 22998715.

10. Pessaux P, Tuech JJ, Derouet N, Rouge C, Regenet N, Arnaud JP. Laparoscopic cholecystectomy in the elderly: a prospective study. Surg Endosc. 2000; 14:1067–1069. PMID: 11116421.
11. Ambe PC, Weber SA, Christ H, Wassenberg D. Primary cholecystectomy is feasible in elderly patients with acute cholecystitis. Aging Clin Exp Res. 2015; 27:921–926. PMID: 25905472.

12. Fuks D, Duhaut P, Mauvais F, Pocard M, Haccart V, Paquet JC, et al. A retrospective comparison of older and younger adults undergoing early laparoscopic cholecystectomy for mild to moderate calculous cholecystitis. J Am Geriatr Soc. 2015; 63:1010–1016. PMID: 25946647.

13. Fukami Y, Kurumiya Y, Mizuno K, Sekoguchi E, Kobayashi S. Cholecystectomy in octogenarians: be careful. Updates Surg. 2014; 66:265–268. PMID: 25266894.

14. Loozen CS, van Ramshorst B, van Santvoort HC, Boerma D. Early cholecystectomy for acute cholecystitis in the elderly population: a systematic review and meta-analysis. Dig Surg. 2017; 34:371–379. PMID: 28095385.

15. Yetkin G, Uludag M, Oba S, Citgez B, Paksoy I. Laparoscopic cholecystectomy in elderly patients. JSLS. 2009; 13:587–591. PMID: 20202402.

16. Lee SI, Na BG, Yoo YS, Mun SP, Choi NK. Clinical outcome for laparoscopic cholecystectomy in extremely elderly patients. Ann Surg Treat Res. 2015; 88:145–151. PMID: 25741494.

17. Tokyo Guidelines for the management of acute cholangitis and cholecystitis. Proceedings of a consensus meeting, April 2006, Tokyo, Japan. J Hepatobiliary Pancreat Surg. 2007; 14:1–121.
18. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci. 2012; 19:578–585. PMID: 22872303.

19. Kuy S, Sosa JA, Roman SA, Desai R, Rosenthal RA. Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg. 2011; 201:789–796. PMID: 21741511.

20. Riall TS, Zhang D, Townsend CM Jr, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010; 210:668–677. PMID: 20421027.

21. Kim KH, Sung CK, Park BK, Kim WK, Oh CW, Kim KS. Percutaneous gallbladder drainage for delayed laparoscopic cholecystectomy in patients with acute cholecystitis. Am J Surg. 2000; 179:111–113. PMID: 10773145.

22. Winbladh A, Gullstrand P, Svanvik J, Sandström P. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford). 2009; 11:183–193. PMID: 19590646.

23. Ha JP, Tsui KK, Tang CN, Siu WT, Fung KH, Li MK. Cholecystectomy or not after percutaneous cholecystostomy for acute calculous cholecystitis in high-risk patients. Hepatogastroenterology. 2008; 55:1497–1502. PMID: 19102330.
24. Cull JD, Velasco JM, Czubak A, Rice D, Brown EC. Management of acute cholecystitis: prevalence of percutaneous cholecystostomy and delayed cholecystectomy in the elderly. J Gastrointest Surg. 2014; 18:328–333. PMID: 24197550.

25. Kim IG, Kim JS, Jeon JY, Jung JP, Chon SE, Kim HJ, et al. Percutaneous transhepatic gallbladder drainage changes emergency laparoscopic cholecystectomy to an elective operation in patients with acute cholecystitis. J Laparoendosc Adv Surg Tech A. 2011; 21:941–946. PMID: 22129145.

26. Sutcliffe RP, Hollyman M, Hodson J, Bonney G, Vohra RS, Griffiths EA. Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients. HPB (Oxford). 2016; 18:922–928. PMID: 27591176.
27. Na BG, Yoo YS, Mun SP, Kim SH, Lee HY, Choi NK. The safety and efficacy of percutaneous transhepatic gallbladder drainage in elderly patients with acute cholecystitis before laparoscopic cholecystectomy. Ann Surg Treat Res. 2015; 89:68–73. PMID: 26236695.

28. Merriam LT, Kanaan SA, Dawes LG, Angelos P, Prystowsky JB, Rege RV, et al. Gangrenous cholecystitis: analysis of risk factors and experience with laparoscopic cholecystectomy. Surgery. 1999; 126:680–685. PMID: 10520915.

29. McGillicuddy EA, Schuster KM, Barre K, Suarez L, Hall MR, Kaml GJ, et al. Non-operative management of acute cholecystitis in the elderly. Br J Surg. 2012; 99:1254–1261. PMID: 22829411.

30. Wiggins T, Markar SR, Mackenzie H, Jamel S, Askari A, Faiz O, et al. Evolution in the management of acute cholecystitis in the elderly: population-based cohort study. Surg Endosc. 2018; 32:4078–4086. PMID: 30046948.

31. Nikfarjam M, Yeo D, Perini M, Fink MA, Muralidharan V, Starkey G, et al. Outcomes of cholecystectomy for treatment of acute cholecystitis in octogenarians. ANZ J Surg. 2014; 84:943–948. PMID: 23910372.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download