Abstract
Backgrounds/Aims
This study was conducted to verify and compare the safety and feasibility of single incision laparoscopic cholecystectomy (SILC) and conventional laparoscopic cholecystectomy (CLC).
Methods
A total of 2,080 patients underwent laparoscopic cholecystectomy in a single center, Konyang University Hospital, between 2010 and 2016. We retrospectively compared the demographics, perioperative outcome, and postoperative complication results between the CLC and SILC groups.
Results
Among the 2,080 patients who underwent laparoscopic cholecystectomy, 1,080 had CLC and 1,000 had SILC. When retrospectively reviewed, the SILC group had significantly higher percentages of patients who were aged under 80 years, who were women, and had the American Society of Anesthesiologist score of lower than 3 points compared to those of the CLC group. Furthermore, the CLC group had a higher percentage of patients with acute cholecystitis or empyema, whereas the SILC group had a higher percentage of patients with chronic cholecystitis. Preoperative percutaneous transhepatic gallbladder drainage insertion or H-vac insertion was more frequently conducted, bleeding loss was more common, and hospital stay was longer in the CLC group. Postoperative complications such as wound infection, biloma, bile duct injury, and duodenal perforation were not significantly different between the two groups.
Go to : 
Laparoscopic cholecystectomy is a minimally invasive surgery for the treatment of benign gallbladder disease compared to the open cholecystectomy and has been established as a gold standard because of its advantages such as less postoperative pain, better cosmetics, and shorter length of hospital stay.12 Subsequently, a minimally invasive surgery has emerged, and many attempts have been made to reduce the number of ports and incision size following the trend of Natural Orifice Transluminal Endoscopy Surgery (NOTES). Then, in 1997, single incision laparoscopic cholecystectomy (SILC) was first performed by Navarra et al.3 Compared to the conventional 4-port surgery that used one instrument per port, this is a multiport method using a transumbilical trocar. Since then, interest in SILC has increased among many surgeons, and various attempts have been made.456789 However, even though the feasibility and safety of SILC have been demonstrated in many studies comparing SILC and CLC,10111213 the feasibility and safety of SILC compared to CLC remains controversial because no clear indications or standard methods have been established due to the technical difficulty of SILC. In the midst of this controversy, our center has developed and implemented a procedure called the Konyang Standard Method (KSM) as a surgical technique for SILC since 2010,14 and KSM has been consistently progressed. Therefore, this study aimed to verify the feasibility and safety of SILC by retrospectively comparing the perioperative outcomes and postoperative complications between the CLC and SILC performed using KSM with evolution developed in our center for a large group of 2,080 patients who underwent laparoscopic cholecystectomy in the Konyang University Hospital.
Go to : 
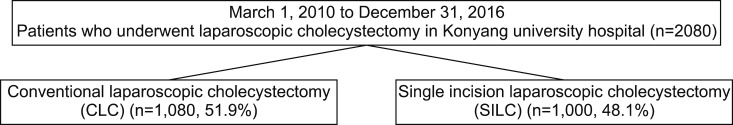
A total of 2,080 patients who underwent laparoscopic cholecystectomy at Konyang University Hospital between March 2010 and December 2016 were divided into two groups: those who underwent CLC and those who underwent SILC (Fig. 1). Then, the patient characteristics, perioperative outcomes, and postoperative complications of these two groups were retrospectively compared and analyzed. The patient characteristics included age, sex, body mass index (BMI), history of previous abdominal surgery, and the American Society of Anesthesiologist (ASA) score. The perioperative outcomes included preoperative PTGBD insertion, operation time, bleeding loss, H-vac insertion, hospital stay, and pathology. Postoperative complications included wound infection, biloma, intra-abdominal abscess, bile duct injury, incisional hernia, duodenal perforation, small bowel injury, and mortality based on the Clavien-Dindo Classification.15
CLC was performed using the conventional 3-port method including the umbilicus. For the basic procedure of SILC, the KSM was used, which had been published by our center in the Annals of Surgical Treatment and Research in 2014.14 The KSM is a 3-channel method using hand-made ports composed of a 10-mm-sized ALEXIS wound retractor and 7-sized sterile gloves, with laparoscopic instruments inserted in the glove fingertips, which allows basic traction, dissection, isolation, ligation, and dissection. Since 2010 when the SILC was first attempted in our center, the technique has evolved through increased operator skills and accumulated experiences into the modified KSM, which has improved Carlot's triangle visualization by adding a snake retractor to compensate for the limitations of the existing KSM. Thesis about KSM with evolution is recorded by Kim MK et al.16 in Annals of Surgical Treatment and Research.
Continuous variables were analyzed using Student's t-test, and categorical data were analyzed using the chi-square test or Fisher's exact test. p-values of <0.05 were considered statistically significant. Statistical analysis was performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Go to : 
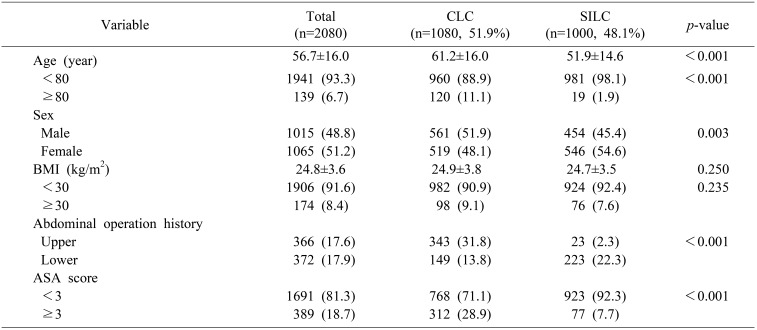
The average age of patients who underwent laparoscopic cholecystectomy at the Konyang University Hospital between March 2010 and December 2016 is 56.7±16.0 years. When comparing the average age between the two groups, the SILC group was significantly younger than the CLC group (51.9±14.6 vs. 61.2±16.0, p <0.001). Among the patients in the CLC group, 88.9% were under 80 years of age, and among the patients in the SILC group, 98.1% were under 80 years of age. Thus, patients younger than 80 years of age were significantly more likely to receive SILC than CLC (p<0.001). Furthermore, in case of female patients, 519 patients underwent CLC and 546 patients underwent SILC. Thus, the percentage of female patients who underwent SILC was statistically significantly higher than those who underwent CLC (48.1% vs. 54.6%, p=0.003). The percentage of patients with upper abdominal operation history was significantly higher in the CLC group with 23 patients (2.3%) in the SILC group and 343 patients (31.8%) in the CLC group (p<0.001). When the ASA score was compared, SILC group received a score lower than three points, which were significantly higher than those in the CLC group (92.3% vs. 71.1%, p<0.001) (Table 1).
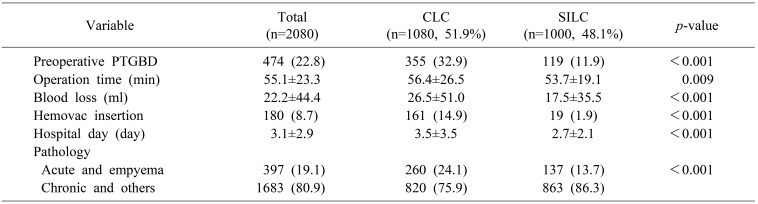
The cases of preoperative PTGBD insertion were 474 out of the 2,080 patients (22.8%), and among them, 355 underwent CLC and 119 underwent SILC. Thus, the number of patients was significantly lower in the SILC than the CLC group (32.9% vs. 11.9%, p<0.001). Compared to the CLC group, the operation time was significantly shorter (56.4±26.5 min vs. 53.7±19.1 min, p=0.009) and the blood loss was also significantly less (26.5±51.0 ml vs. 17.5±35.5 ml, p<0.001) in the SILC group. Furthermore, the cases of H-vac drain insertion in the SILC group was significantly lower (14.9% vs. 1.9%, p<0.001), and the length of hospital stay was significantly shorter in the SILC group (3.5±3.5 days vs. 2.7±2.1 days, p<0.001). The postoperative pathologic findings showed that acute cholecystitis and empyema were significantly more frequent in the CLC group (24.1% vs. 13.7%, p<0.001) (Table 2).
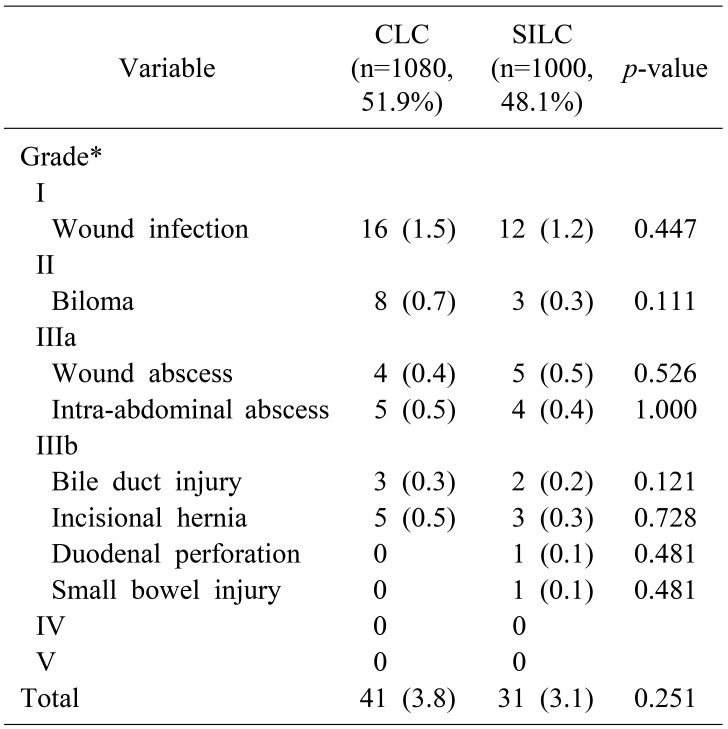
All complications were classified based on the Clavien-Dindo Classification by Grade I–V.15 When the two groups were compared, the total cases of reported postoperative complications were 41 cases (3.8%) in the CLC group and 31 cases (3.1%) in the SILC group; thus, no significant difference was observed (p=0.251). The most common complications in both SILC and CLC groups were wound infections in the umbilicus (grade 1), with 16 cases (1.5%) in the CLC group and 12 cases (1.2%) in the SILC group; thus, no significant difference was observed (p=0.447). The cases of biloma (grade 2) were 8 cases (0.7%) in the CLC group and 3 cases (0.3%) in the SILC group (p=0.111). The cases of grade 3 complications in the SILC group included bile duct injury was 2 cases, incisional hernia was 3 cases, duodenal perforation was 1 case, and small bowel injury was 1 case. The postoperative complications in the SILC group were not statistically significantly more frequent than those in the CLC group (p=0.121, p=0.728, p=0.481, p=0.481) (Table 3).
Go to : 
Since the first performance of laparoscopic cholecystectomy in 1985, it has been established as a gold standard method for gallbladder surgery, owing to its advantages such as cosmetically less surgical wounds, less postoperative pain, and shorter recovery period compared to open cholecystectomy.12 The conventional laparoscopic cholecystectomy has used a total of three or four ports for insertion including the umbilicus. However, recently, surgeons are actively attempting the SILC as they have researched new instruments and methods to reduce unnecessary port insertions following the trend of minimal invasiveness. However, due to surgeon's technical difficulty, whether SILC will be more effective in gallbladder surgery than the existing CLC remains controversial. However, whether SILC is more beneficial than conventional CLC in gallbladder surgery due to the operator's skills and technical difficulty of SILC also remains controversial. Therefore, many studies on the feasibility and safety of SILC are actively conducted along with the research on surgical instruments and technical methods.56789 Our study is significant because it compared and analyzed a large group of patients (over 2,000) in one center, which is much larger than the scales of previous studies.
SILC is a single-incision multi-port method using the umbilicus instead of using three or four ports as with the conventional method, and many surgeons have been actively trying out and publishing proprietary surgical techniques to perform a more stable operation using the existing instruments.12 Our center also has independently developed and used the KSM since 2010 and has improved the technique while complementing various limitations and published results.14 Many surgeons are having difficulties with the visualization of the Calot's triangle when performing SILC, and our center solved this problem through liver traction by adding a snake retractor. At first, we used a self-made glove port, but have commercialized it later, and now we are using it as a representative surgical technique.16
The most common postoperative complication among the 2,080 patients who underwent laparoscopic cholecystectomy in our center was wound infection (SILC 1.2%, CLC 1.5%), followed by biloma (CLC 0.7%, SILC 0.3%), bile duct injury (CLC 0.3%, SILC 0.2%), and incisional hernia (CLC 0.5%, SILC 0.3%). Duodenal perforation occurred in only one patient who underwent SILC, and mortality was 0% in all patients. All these postoperative complications did not show statistically significant differences in both SILC and CLC groups. Bile duct injury is usually caused by lack of confirmation of local anatomy and technical error. Compared to the current mean bile duct injury rate after SILC that is reported as 0.7%,17 rate of bile duct injury after SILC in our center were lower (0.2%). This result is likely to be attributed to the surgeon's surgical experience with SILC and to the use of a snake retractor as an operative method for better exposure of the carlot's triangle. Furthermore, another study reported that the incisional hernia rate after SILC was 8% and argued that we need to select patients who are younger and not obese to reduce this risk.18 In the initial period with SILC in our center, 2 cases of incisional hernia had occurred, but since then, with careful suture after surely exfoliate the skin from the fascia, the rate of incisional hernia has been dramatically reduced. Compared to this study, the incisional hernia rate in our center was very low at 0.3% for SILC and 0.5% for CLC, and no significant difference was observed between them. SILC requires surgeon's skills because several conventional instruments must be inserted into a single port, and especially for obese patients, securing the visual field of operation is more difficult; therefore, an instrument that can help to visualize is needed. Thus, SILC can be more difficult and take longer compared to the conventional CLC. In our center, the mean operation time was 55.1±23.3 min, and no statistically significant difference was observed between the two groups, with 56.4±26.5 min for CLC and 53.7±19.1 min for SILC.
According to SG Kim et al.,19 the conversion rate from SILC to CLC was significantly higher in patients with ASA score of 3 or more and who underwent preoperative PTGBD insertion, and most of the cases were acute cholecystitis or GB empyema. When performing a benign GB surgery, the patient's gallbladder is highly at risk of bleeding during surgery if the inflammation is severe enough to require PTGBD insertion, and the procedure is very likely to be converted to CLC if SILC is attempted unnecessarily. Thus, in case of acute cholecystitis or empyema before surgery, CLC should be performed rather than SILC. In other words, SILC should be performed by patient selection based on the degree of inflammation of the gallbladder.
When the SILC and CLC groups are retrospectively analyzed, patients who underwent SILC in our center were younger, included a higher percentage of women, and had more cases of chronic cholecystitis than acute cholecystitis or empyema in the postoperative gallbladder pathology. Patients who had upper abdominal surgical history prior to surgery or who underwent PTGBD insertion were more likely to undergo CLC than SILC, and acute cholecystitis and empyema were more frequently observed in the postoperative pathology. This finding suggests that patients who have good morphology, female patients who may highly regard cosmetics, and patients who do not have severe inflammation were mainly selected for SILC in our center. In fact, patients with abdominal surgical history may have severe adhesion in their abdomen and a high bleeding risk when they undergo SILC, which requires many techniques, and as a result, the operation time may become longer. Therefore, CLC may be preferred over SILC or additional port insertion may be inevitable during SILC. Sato N. et al. argued that the factors that may require additional port insertion during SILC were gender, prior history of upper abdominal surgery, and white blood cell count.20
In the present study, patients who underwent SILC after a preoperative patient selection showed less blood loss and lower ratio of H-vac drain insertion compared to those who underwent CLC. Other studies also reported that SILC shows relatively good progress during and after surgery compared to conventional surgical techniques. Tsimoyiannis et al.7 and Brody et al.8 reported that SILC was associated with less perioperative pain and lower dosage of pain medication. Furthermore, better cosmetic improvement of SILC was also reported in several studies.5621 With regard to the length of hospital stay, other studies reported that no significant change was observed in patients who underwent SILC compared to the existing surgical technique.59 However, this study showed more significant results because the length of hospital stay was significantly shorter among the patients in the SILC group (CLC 3.5±3.5 days, SILC 2.7±2.1 days). Furthermore, obesity may cause technical difficulty during SILC and may act as a relative contraindication; however, BMI was not significantly different between the SILC and CLC groups. According to Obuchi et al.,22 BMI of ≥30 kg/m2 does not have an adverse impact on the technical difficulty and postoperative outcomes of SILC, and obesity-related comorbidities did not increase the risks for SILC. However, since differences may occur depending on the actual surgeon's skills, the BMI criteria during the patient selection for SILC remain unclear.
Several studies have compared the efficacy of SILC and CLC in patients with benign gallbladder disease until recently; however, their patient pools were slightly over 100.101112 This study is significant because SILC and CLC were compared in a group of more than 2,000 patients who underwent laparoscopic cholecystectomy in a single center. This study retrospectively compared the characteristics, perioperative outcomes, and postoperative complications on a total of 2,080 patients who underwent laparoscopic cholecystectomy between 2010 and 2016 to determine whether SILC can effectively replace CLC and to assess the safety of SILC in terms of postoperative complications.
This study is a retrospective analysis based on the medical records of patients who underwent laparoscopic cholecystectomy in our center, and did not compare the postoperative pain, and cosmesis. Most papers reported that patients who underwent SILC showed higher satisfaction regarding their surgical wounds than those who underwent CLC.2324 This finding suggests that SILC can replace CLC in patients who have concerns about postoperative surgical wounds and who value cosmetics. Thus, in the future, a prospective study and a study on a scoring system that can objectify the subjective results of postoperative pain and cosmesis will be necessary.
In conclusion, if performed after preoperative patient selection such as in younger and female patients with no abdominal operation history at the time of benign gall-bladder surgery, SILC can be considered feasible and safe without additional complications when compared with CLC. This study is significant because it compared and analyzed a large group of patients (over 2,000) in one center, which is much larger than the scales of previous studies.
Go to : 
References
1. Begos DG, Modlin IM. Laparoscopic cholecystectomy: from gimmick to gold standard. J Clin Gastroenterol. 1994; 19:325–330. PMID: 7876516.

2. Chamberlain RS, Sakpal SV. A comprehensive review of Single-Incision Laparoscopic Surgery (SILS) and Natural Orifice Transluminal Endoscopic Surgery (NOTES) techniques for cholecystectomy. J Gastrointest Surg. 2009; 13:1733–1740. PMID: 19412642.

3. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695. PMID: 9171771.

4. Erhart D, Pohnán R. [55 laparoscopic cholecystectomies using single incision laparoscopic surgery--initial experience]. Rozhl Chir. 2011; 90:361–364. Czech. PMID: 22026104.
5. Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G. Laparoendoscopic single site (LESS) versus classic video-laparoscopic cholecystectomy: a randomized prospective study. J Surg Res. 2011; 166:e109–e112. PMID: 21227454.

6. Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011; 98:1695–1702. PMID: 21964736.

7. Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010; 24:1842–1848. PMID: 20174950.

8. Brody F, Vaziri K, Kasza J, Edwards C. Single incision laparoscopic cholecystectomy. J Am Coll Surg. 2010; 210:e9–e13. PMID: 20113931.

9. Joseph M, Phillips MR, Farrell TM, Rupp CC. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg. 2012; 256:1–6. PMID: 22664556.
10. Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, et al. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc. 2010; 24:2241–2247. PMID: 20198490.

11. Erbella J Jr, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010; 24:1958–1961. PMID: 20112110.

12. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010; 24:1403–1412. PMID: 20035355.

13. Hirano Y, Watanabe T, Uchida T, Yoshida S, Tawaraya K, Kato H, et al. Single-incision laparoscopic cholecystectomy: single institution experience and literature review. World J Gastroenterol. 2010; 16:270–274. PMID: 20066749.

14. Son JI, Choi IS, Moon JI, Ra YM, Lee SE, Choi WJ, et al. Single incision laparoscopic cholecystectomy using Konyang Standard Method. Ann Surg Treat Res. 2014; 86:177–183. PMID: 24783176.

15. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
16. Kim MK, Choi IS, Moon JI, Lee SE, Yoon DS, Kwon SU, et al. Evolution of the Konyang Standard Method for single incision laparoscopic cholecystectomy: the result from a thousand case of a single center experience. Ann Surg Treat Res. 2018; 95:80–86. PMID: 30079324.

17. Li T, Kim G, Chang S. Tips and tricks to avoid bile duct injury in SILC: an experience of 500 cases. Surg Endosc. 2016; 30:4750–4755. PMID: 26932550.

18. Julliard O, Hauters P, Possoz J, Malvaux P, Landenne J, Gherardi D. Incisional hernia after single-incision laparoscopic cholecystectomy: incidence and predictive factors. Surg Endosc. 2016; 30:4539–4543. PMID: 26895902.

19. Kim SG, Moon JI, Choi IS, Lee SE, Sung NS, Chun KW, et al. Risk factors for conversion to conventional laparoscopic cholecystectomy in single incision laparoscopic cholecystectomy. Ann Surg Treat Res. 2016; 90:303–308. PMID: 27274505.

20. Sato N, Yabuki K, Kudo Y, Koga A, Kohi S, Tamura T, et al. Preoperative factors predicting the need for additional ports during single-incision laparoscopic cholecystectomy. Asian J Endosc Surg. 2016; 9:192–197. PMID: 27113627.

21. van den Boezem PB, Velthuis S, Lourens HJ, Cuesta MA, Sietses C. Single-incision and NOTES cholecystectomy, are there clinical or cosmetic advantages when compared to conventional laparoscopic cholecystectomy? A case-control study comparing single-incision, transvaginal, and conventional laparoscopic technique for cholecystectomy. World J Surg. 2014; 38:25–32. PMID: 24081531.

22. Obuchi T, Kameyama N, Tomita M, Mitsuhashi H, Miyata R, Baba S. Impact of obesity on surgical outcome after single-incision laparoscopic cholecystectomy. J Minim Access Surg. 2018; 14:99–104. PMID: 28695876.

23. Haueter R, Schütz T, Raptis DA, Clavien PA, Zuber M. Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg. 2017; 104:1141–1159. PMID: 28569406.

24. Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, DeNoto G, et al. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. 2012; 26:1296–1303. PMID: 22083331.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download