Abstract
Backgrounds/Aims
Gallstones are being increasingly diagnosed in pediatric patients. The purpose of this study was to determine characteristics of pediatric patients who underwent cholecystectomy because of symptomatic gallstone disease unrelated to hemolytic disorder.
Methods
We reviewed cases of pediatric patients (under 18 years old) who underwent cholecystectomy between May 2005 and December 2015.
Results
A total 20 pediatric patients (under 18 years old) underwent cholecystectomy during the study period. One patient was excluded because cholecystectomy was performed due to gall stones caused by hemolytic anemia. The 19 cases comprised 9 male (47.3%) and 10 female (52.7%) subjects. The mean age was 14.9 years (range, 5-18), and 66.7% of patients were older than 12 years of age. Mean body weight was 65.0 kg (range, 13.9-93.3), and mean body mass index was 21.7 kg/m2 (range, 12.3-35.1), with 26.37% of patients being overweight. All 19 patients underwent laparoscopic cholecystectomy. There were no postoperative complications and no mortality. Comparison between overweight and non-overweight patients indicated that significantly more overweight patients had cholesterol stones (5/5 vs. 7/14, p=0.036) and were classified as complicated disease (3/5 vs. 1/14, p=0.037).
Conclusions
The more frequent occurrence of complications such as choledocholithiasis or gallstone pancreatitis, in overweight patients indicates the need for more careful evaluation and management in these patients. Pediatricians and surgeons should always consider gallstone disease in pediatric patients despite difficulty in suspecting symptomatic gallstones in cases who present with abdominal pain that is rarely clear-cut.
Go to : 
Cholecystectomy is a common surgical procedure in adults, but is relatively uncommon in children.12 However, the number of cholecystectomy in children has increased over the past two decades.34 The widespread use of ultrasonography for the diagnosis of the pediatric patients who present with abdominal pain has increased the diagnosis of symptomatic gallstones and the rate of cholecystectomy in the pediatric population.5 Some authors67 report that increasing obesity among children has increased the prevalence of gallstones in children and cholecystectomy rate.
In contrast to adults, gallbladder disease in children is usually observed primarily in patients with morbid conditions, such as hemolytic disorder.8 Recently, some reports indicated that the proportion of hemolytic disease has decreased and that of other conditions without hemolytic disease has increased.34 Although biliary dyskinesia is reported as the most prevalent cause of pediatric cholecystectomy in western populations,91011 symptomatic gallstones remain the most common cause of pediatric cholecystectomy and idiopathic etiology is estimated between 20 and 65%.81112
In Korea, the reports on pediatric cholecystectomy for gallstone disease13141516 are limited. The aim of this study was to describe our experience and characterize pediatric patients who underwent cholecystectomy for symptomatic gallstone disease unrelated to hemolytic disorder in a single center.
Go to : 
We retrospectively reviewed the medical records of pediatric patients (under 18 years old) who underwent cholecystectomy due to gallstone disease between May 2005 and December 2015 at Chung-Ang University Hospital. Patients who underwent cholecystectomy due to other diseases such as hemolytic disorder were excluded. Basic demographic characteristics included sex, age, high, body weight, body mass index (BMI). Clinical characteristics included laboratory and radiologic findings, pathologic results, and operative outcomes. BMI equal to or greater than 25 kg/m2 was considered overweight. Complicated disease were defined as choledocholithiasis, gallstone pancreatitis, or empyema.
All statistical analyses were performed using the Statistical Package for the Social Sciences version 21.0 (SPSS, Chicago, IL). Comparisons of nominal data were conducted using the Chi-square test, and continuous variables were compared using the student t-test. Statistical significance was determined at p<0.05.
Go to : 
A total 20 pediatric patients (under 18 years old) underwent cholecystectomy during the study period. One case was excluded due to gall stones caused by hemolytic anemia. Finally, 19 cases were selected as the subject group. The subjects included 9 males (47.3%) and 10 females (52.7%) with a mean age of 14.9 years (range, 5-18), with the majority (66.7%) being older than 12 years. Mean body weight was 57.3 kg (range, 13.9-93.3), and mean BMI was 21.7 kg/m2 (range, 12.3-35.1), with BMI>25 kg/m2 in 5 patients (26.4%). The majority of patients (n=16, 84.2%) presented with abdominal pain at the right upper quadrant.
Four patients were classified as complicated disease; 2 cases were choledocholithiasis, 1 was gallstone pancreatitis and the other was empyema. The choledocholithiasis cases were managed by endoscopic retrograde cholangiography (ERCP) before cholecystectomy. There were no postprocedural complications. One patient with acute pancreatitis was diagnosed as gallstone pancreatitis following comprehensive investigation; the patients' symptom resolved following cholecystectomy.
All 19 patients underwent laparoscopic cholecystectomy with no conversion to open procedure. Mean operation times and mean hospital stay was 53.2±11.0 minutes and 5.4±2.9 days, respectively. There were no postoperative complication and no mortality.
Stone analysis indicated cholesterol stones in 10 patients (55.6%), and black pigment stones in 8 patients.
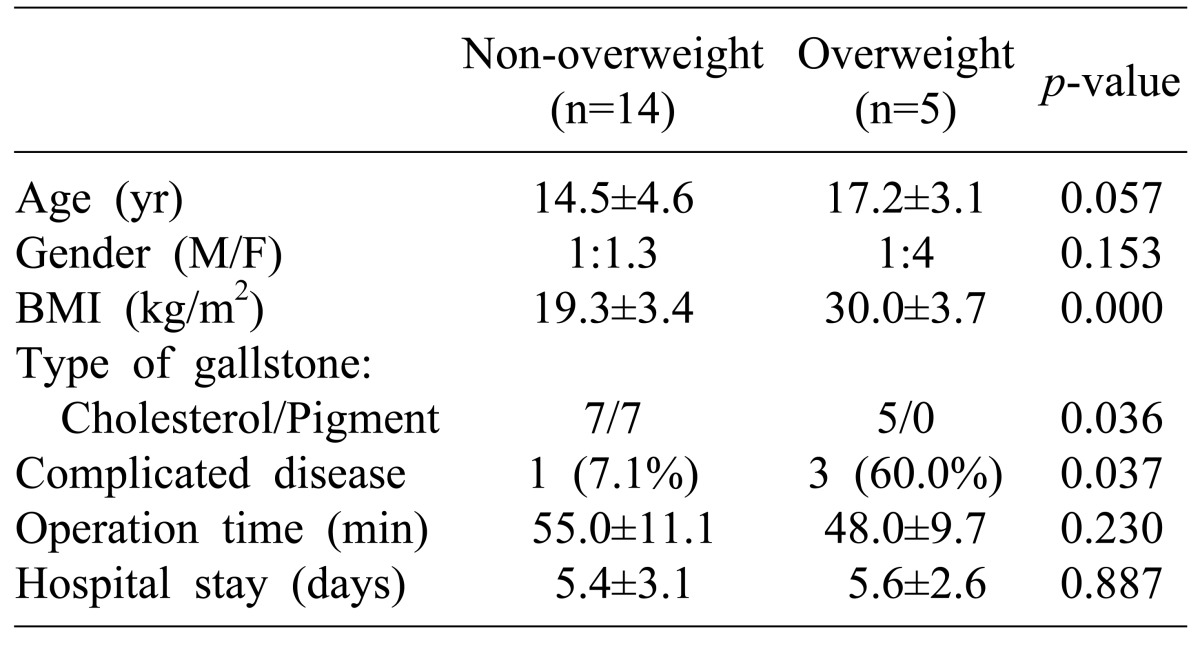
Comparison between overweight and non-overweight patients revealed that significantly more overweight patients had cholesterol stones (5/5 vs. 7/14, p=0.036) and were classified as complicated disease (3/5 vs. 1/14, p=0.037) (Table 1).
Postoperative diagnoses confirmed by pathologic examination were acute or chronic cholecystitis (17 cases), empyema (1 case), and adenomyomatosis (1 case).
Go to : 
Cholecystectomy is rarely performed in pediatric patients, but is a very common operation in adults. Recently, several studies have reported increasing cases of cholecystectomy in pediatric patients, and change in the indication for cholecystectomy from hematologic disease to non-hematologic gall stone disease.35 The reason for the increase in cholecystectomies in the pediatric population is likely multifactorial. The widespread use of abdominal ultrasound in the diagnosis of non-specific abdominal pain5 and increasing prevalence of obesity in children67 are considered as main reasons for the increased rate of cholecystectomy. However, a genuine increase in the incidence of cholelithiasis is expected from recognized predisposing factors, such as total parenteral nutrition, obesity, and prematurity, etc.1611 In western counties, there has been an increasing rate of cholecystectomy for biliary dyskinesia789 and in the United States, biliary dyskinesia is an indication in 20-50% of cholecystectomies.1718 In the present study, during study period only one patient (5%) underwent cystectomy due to gallstones related to hemolytic anemia.
While boys and girls are equally affected in early childhood, as in adults, most previous studies reported a female predominance in pediatric gallbladder disease starting from puberty.45 In the present study, we found equal sex distribution overall and even above the age of 12 years. Although the reason of the discrepancy is unclear, in Eastern countries, the female predominance is not apparent even in adults.19
There is clear association between obesity and gallstone formation, especially in early puberty.20 However, this phenomenon is only now gaining recognition in the pediatric population.212223 Compared to adults, it can be somewhat difficult to accurately evaluate childhood obesity in terms of BMI and this has led to inconsistent results in the previous reports.424 In our study, 5 patients were classified as overweight; of these, significantly more patients had cholesterol stones than the non-overweight patients (5/5 vs. 7/14, p=0.036). The result suggested that obesity is associated with the formation of cholesterol stones. In the overweight patients group, significantly more patients were classified as complicated disease (3/5 vs. 1/14, p=0.037); thus, overweight might be a potential aggravating factor in pediatric gallstone disease. Thorough evaluation and more care are recommended in obese pediatric patients with gallstones.
Acute and chronic cholecystitis, ascending cholangitis, common bile duct stones and choledocholithiasis, and pancreatitis are the major problems and complications observed in patients with gallstone. The frequency of complications varied in the published literature. Generally, choledocholithiasis is found in 8-10% of adult patients with cholelithiasis and 10% to 15% of pediatric patients with gallstones.521 Two patients with choledocholithiasis in the present study were successfully managed by ERCP without complications. However, considering the 11% complication rate that accompanies ERCP in children and the high rate of general anesthesia for the procedure,2526 effective management method of choledocholithiasis remains debatable.
In Western countries, biliary dyskinesia is an increasingly recognized diagnosis and an indication for surgery in 20-50 % of cholecystectomies.789 The diagnosis of biliary dyskinesia is defined as gallstone-like pain attacks combined with an ejection fraction below 35% during hepatobiliary iminoacetic acid (HIDA) scanning.27 Supportive scientific evidence for cholecystectomy in cases of biliary dyskinesia is not adequate. Further prospective randomized trials with long-term follow-up are needed to determine the true efficacy of surgical treatment of biliary dyskinesia.
In conclusion, because overweight patients can experience complications such as choledocholithiasis or gallstone pancreatitis, more careful evaluation and management for overweight patients is needed. It is difficult to suspect symptomatic gallstones in pediatric patients who present with abdominal pain due to symptoms that are rarely clear-cut. However, because the rate of symptomatic gallstones has increased in the pediatric population, pediatricians and surgeons should have a high suspicion for gallstone disease.
Go to : 
References
1. Bailey PV, Connors RH, Tracy TF Jr, Sotelo-Avila C, Lewis JE, Weber TR. Changing spectrum of cholelithiasis and cholecystitis in infants and children. Am J Surg. 1989; 158:585–588. PMID: 2511775.

2. Kang JY, Ellis C, Majeed A, Hoare J, Tinto A, Williamson RC, et al. Gallstones--an increasing problem: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003; 17:561–569. PMID: 12622765.
3. Balaguer EJ, Price MR, Burd RS. National trends in the utilization of cholecystectomy in children. J Surg Res. 2006; 134:68–73. PMID: 16650434.

4. Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics. 2012; 129:e82–e88. PMID: 22157135.

5. Wesdorp I, Bosman D, de Graaff A, Aronson D, van der Blij F, Taminiau J. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr. 2000; 31:411–417. PMID: 11045839.

6. Kaechele V, Wabitsch M, Thiere D, Kessler AL, Haenle MM, Mayer H, et al. Prevalence of gallbladder stone disease in obese children and adolescents: influence of the degree of obesity, sex, and pubertal development. J Pediatr Gastroenterol Nutr. 2006; 42:66–70. PMID: 16385256.

7. Garey CL, Laituri CA, Keckler SJ, Ostlie DJ, Stagg HW, Little DC, et al. Laparoscopic cholecystectomy in obese and non-obese children. J Surg Res. 2010; 163:299–302. PMID: 20537352.

8. Kaye AJ, Jatla M, Mattei P, Kelly J, Nance ML. Use of laparoscopic cholecystectomy for biliary dyskinesia in the child. J Pediatr Surg. 2008; 43:1057–1059. PMID: 18558182.

9. Hofeldt M, Richmond B, Huffman K, Nestor J, Maxwell D. Laparoscopic cholecystectomy for treatment of biliary dyskinesia is safe and effective in the pediatric population. Am Surg. 2008; 74:1069–1072. PMID: 19062663.

10. Al-Homaidhi HS, Sukerek H, Klein M, Tolia V. Biliary dyskinesia in children. Pediatr Surg Int. 2002; 18:357–360. PMID: 12415355.

11. Palasciano G, Portincasa P, Vinciguerra V, Velardi A, Tardi S, Baldassarre G, et al. Gallstone prevalence and gallbladder volume in children and adolescents: an epidemiological ultrasonographic survey and relationship to body mass index. Am J Gastroenterol. 1989; 84:1378–1382. PMID: 2683739.
12. Nomura H, Kashiwagi S, Hayashi J, Kajiyama W, Ikematsu H, Noguchi A, et al. Prevalence of gallstone disease in a general population of Okinawa, Japan. Am J Epidemiol. 1988; 128:598–605. PMID: 3046339.

13. Kim HS, Nam SH, Kim DY, Kim SC, Kim IK. Laparoscopic cholecystectomy in children. J Korean Assoc Pediatr Surg. 2006; 12:213–220.

14. Eun HS, Baek SY, Chung KS. A clinical study for gall bladder stones in children. Korean J Pediatr Gastroenterol Nutr. 2005; 8:194–201.

15. Kim SY, Seo JK. Cholelithiasis in childhood. J Korean Pediatr Soc. 1994; 37:70–77.
16. Kim CS, Koo BH. Laparoscopic cholecystectomy in the pediatric patient. J Korean Surg Soc. 1993; 45:293–297.
17. Walker SK, Maki AC, Cannon RM, Foley DS, Wilson KM, Galganski LA, et al. Etiology and incidence of pediatric gallbladder disease. Surgery. 2013; 154:927–931. PMID: 24074432.

18. Lacher M, Yannam GR, Muensterer OJ, Aprahamian CJ, Haricharan RN, Perger L, et al. Laparoscopic cholecystectomy for biliary dyskinesia in children: frequency increasing. J Pediatr Surg. 2013; 48:1716–1721. PMID: 23932611.

19. Chang YR, Jang JY, Kwon W, Park JW, Kang MJ, Ryu JK, et al. Changes in demographic features of gallstone disease: 30 years of surgically treated patients. Gut Liver. 2013; 7:719–724. PMID: 24312714.

20. Stender S, Nordestgaard BG, Tybjaerg-Hansen A. Elevated body mass index as a causal risk factor for symptomatic gallstone disease: a Mendelian randomization study. Hepatology. 2013; 58:2133–2141. PMID: 23775818.

21. Holcomb GW Jr, Holcomb GW 3rd. Cholelithiasis in infants, children, and adolescents. Pediatr Rev. 1990; 11:268–274. PMID: 2408028.

22. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006; 295:1549–1555. PMID: 16595758.

23. Luo J, Hu FB. Time trends of obesity in pre-school children in China from 1989 to 1997. Int J Obes Relat Metab Disord. 2002; 26:553–558. PMID: 12075583.

24. Bogue CO, Murphy AJ, Gerstle JT, Moineddin R, Daneman A. Risk factors, complications, and outcomes of gallstones in children: a single-center review. J Pediatr Gastroenterol Nutr. 2010; 50:303–308. PMID: 20118803.

25. Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. 2004; 60:367–371. PMID: 15332025.

26. Metreweli C, So NM, Chu WC, Lam WW. Magnetic resonance cholangiography in children. Br J Radiol. 2004; 77:1059–1064. PMID: 15569653.

27. Langballe KO, Bardram L. Cholecystectomy in Danish children--a nationwide study. J Pediatr Surg. 2014; 49:626–630. PMID: 24726126.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download