Abstract
Backgrounds/Aims
Synchronous liver metastases (SLMs) are found in 15-25% of patients at the time of diagnosis with colorectal cancer, which is limited to the liver in 30% of patients. Surgical resection is the most effective and potentially curative therapy for metastatic colorectal carcinoma (CRC) of the liver. The comparison of simultaneous resection of primary CRC and synchronous liver metastases with staged resections is the subject of debate with respect to morbidity. Laparoscopic surgery improves postoperative recovery, diminishes postoperative pain, reduces wound infections, shortens hospitalization, and yields superior cosmetic results, without compromising the oncological outcome. The aim of this study is therefore to evaluate our initial experience with simultaneous laparoscopic resection of primary CRC and SLM.
Methods
Currently, laparoscopic resection of primary CRC is performed in more than 53% of all patients in our surgical department. Twenty-six patients with primary CRC and a clinical diagnosis of SLM underwent combined laparoscopic colorectal and liver surgery. Six of them underwent laparoscopic colorectal resection combined with major laparoscopic liver resection.
Results
The surgical approaches were total laparoscopic (25 patients) or hybrid technique (1 patients). The incision created for the extraction of the specimen varied between 5 and 8cm. The median operation time was 223 minutes (100 to 415 min.) with a total blood loss of 180 ml (100-300 ml). Postoperative hospital stay was 6.8 days (6-14 days). Postoperative complications were observed in 6 patients (22.2%).
Go to : 
Laparoscopic liver and colorectal resections, including large-volume surgical procedures, are performed by experienced surgeons and after careful selection of patients with colorectal carcinoma. Laparoscopic resections are accepted therapeutic methods that are appropriate, safe and oncologically equivalent to conventional surgery.123 Nevertheless, there is still no consensus regarding the feasibility of combined resections in cases of primary colorectal carcinoma with synchronous colorectal metastases.345678910111213 The aim of the current study is to determine the feasibility of laparoscopic resections of different tissue volumes in selected patients with primary colorectal carcinoma and synchronous colorectal metastases. The study will be performed at two highly-specialized centers of hepato-biliary surgery where a broad spectrum of laparoscopic colorectal interventions are performed.
Go to : 
Twenty-seven combined liver and colorectal resections were performed during the period from August 2012 to December 2015 at the Clinic of Hepato-pancreato-biliary and Transplantology at the Military Medical Academy, Sofia and Surgical Department of Eurohospital, Plovdiv. The medical histories of patients were compiled and included co-morbidity, tumor characteristics (as the primary and metastatic localization), neoadjuvant therapy administered, types of surgical interventions and intraoperative parameters, blood loss volume, surgery time, postoperative complications (in particular anastomosis insufficiency, transient hepatic failure, postoperative hemorrhage), mortality, and postoperative hospital stays. Follow-up observations included control examinations, medical imaging, and examination of tumor markers at postoperative months 1, 6, 12, 18, 24, 36, etc.
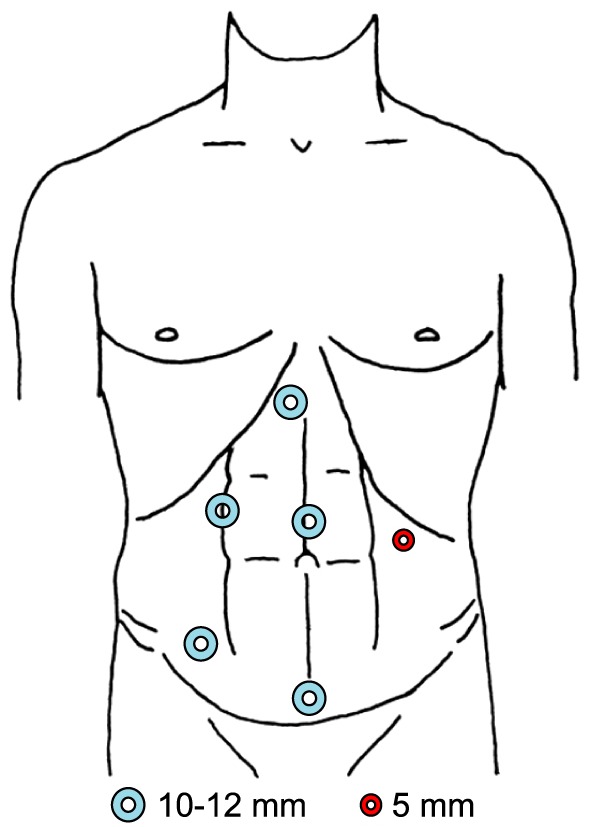
Patients were evaluated by a multidisciplinary health care team. The indications for combined liver and colorectal laparoscopic resection were based on the localization and local status of primary carcinomas, number and localization of liver metastases, co-morbidity, and anesthesiological and cardiac status. The feasibility of combined laparoscopic resection was based on individual examinations, while the criteria for selection were based on the recommendations of Louisville (2008) and Morioka consensuses (2014).1,2 The surgical intervention was performed after acquiring a written informed consent from the patient. A single surgeon performed the combined laparoscopic colorectal and liver resections. The localization of trocars and number of ports were in conformity with the planned intervention and underwent small corrections from the standardized positioning of colorectal surgery (Fig. 1). Every laparoscopic procedure began with a thorough inspection of the abdominal cavity and intraoperative ultrasonography of the liver to verify preoperative findings and the actual correlation to vascular structures to confirm the planned surgical strategy.
The surgical procedure began with the liver resection, followed by the colorectal resection. During the liver resection, a higher pressure of pneumoperitoneum was maintained (14-16 mm Hg), as well as a combined low venous pressure <5 mm Hg. The latter was normalized to 12 mm Hg during the colorectal resection. In contrast to open surgical procedures, a tourniquet was not placed for the Pringle maneuver regardless of the resection volume. Alternatively, selective clamping was preferred. The parenchymal transection was performed by means of an ultrasonic dissector (Cavitron ultrasonic aspirator: CUSA), while hemostasis and cholestasis was performed by bipolar coagulation, clipping, suturing, and application of vascular staplers depending on the diameter of blood vessels. The colorectal resection was performed in compliance with the classic oncological method: high ligation of blood vessels, medio-laterally oriented dissection and total mesorectal excision in the context of low anterior resection. While the double-staple technique is preferred for total intracorporeal anastomosis, an upper midline laparotomy was used only in a patient with a left hemicolectomy combined with a right hepatectomy. An upper midline laparotomy was used with a hybrid approach for two right hepatectomies for extraction of specimens. In contast, the Pfannenstiel approach was used for both specimens in the other patients. Drainages were inserted towards both the hepatic resection surface and the anastomosis.
Go to : 
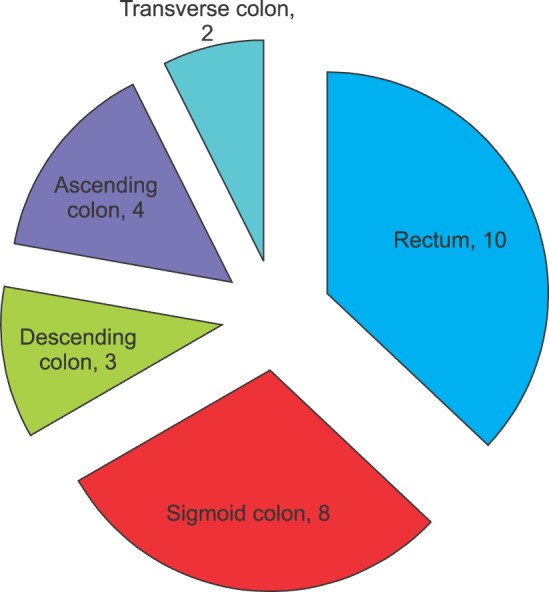
The primary location of colorectal carcinoma was the colon in seventeen patients, and the rectum in ten patients (Fig. 2). Single metastases were diagnosed in sixteen patients, and multiple metastases in eleven patients.
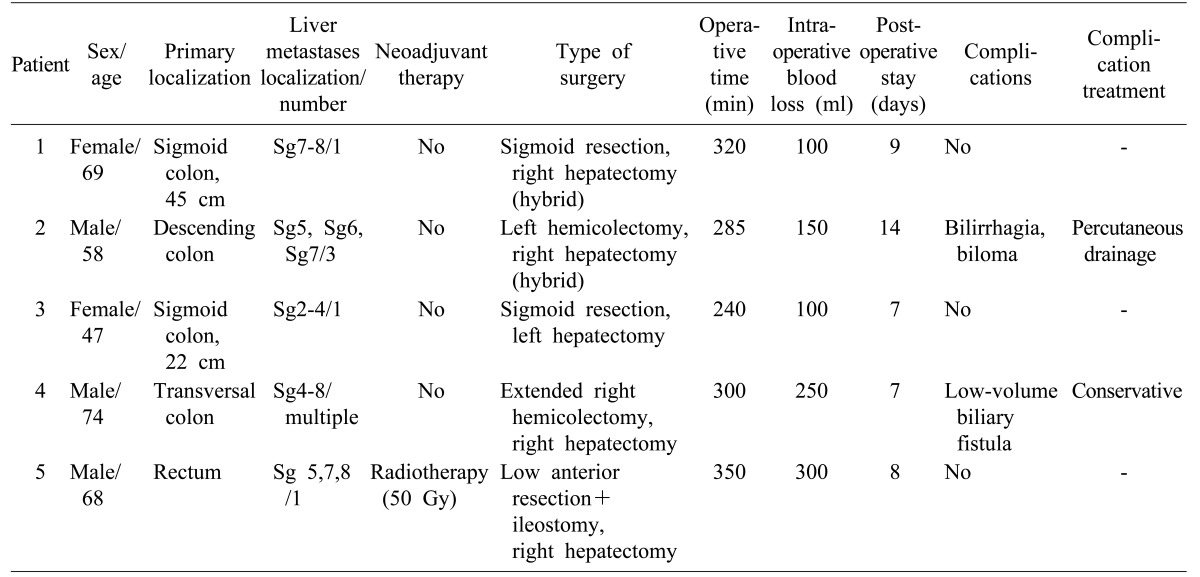
Most procedures were performed completely laparoscopically. Three of the major hepatic resections (right hepatectomies were performed with the hybrid technique. Other major liver resections included four right hepatectomies and one left hepatectomy combined with resection of the sigmoid colon (n=2), a left hemicolectomy (n=1), an extended right hemicolectomy (n=1), and one low anterior resection combined with a protective ileostomy. There were 22 minor liver resections, from solitary metastasectomy to left lateral sectionectomy, combined with right hemicolectomy (n=5), sigmoid resection (n=6), left hemicolectomy (n=2), and anterior resection of the rectum (n=9). The average surgery time was 223 minutes (100 to 415 minutes).
The average intraoperative blood loss was 180 ml (100-300 ml) for the surgical operations combined with major liver resections, and 110 ml (50-200 ml) for the surgical operations combined with minor liver resections. The average postoperative hospital stay was 6.8 days (6-14 days).
Postoperative complications were observed in 6 patients (22.2%). These were bilirrhagia and formation of a biloma after a right hepatectomy (n=1) (Dindo-Clavien grade IIIa), insufficiency of the anastomosis after a low anterior resection (n=1) (grade IIIb), a low-volume bilirrhagia after a left lateral sectionectomy (n=1) (grade II) and resection of the segment 5 (grade II) (n=1), a surgical site infection after sigmoid resection and resection of segment 4b (grade I) (n=1), and one case of postoperative ileus in a patient with sigmoid resection which was managed successfully with conservative treatment (grade II). Complications grade IIIa and IIIb were managed by minimally invasive procedures. A percutaneous pigtail catheter was placed in the patient with biloma, and the latter catheter was removed 30 days later. A repeated laparoscopy placing a suture at the defect was performed in the patient with insufficiency, creating a temporary bi-truncular ileostomia.
R0-resection was achieved in all patients. In one patient with multiple synchronous metastases, the first stage of a two-stage hepatic resection was performed, a metastasectomy from the left lobe, and ligation of the right branch of the portal vein. During an average follow-up period of 12.3 months (from 1 to 40 months) four patients relapsed during the course of receiving adjuvant chemotherapy. One patient underwent a laparoscopic R0 liver resection for 5 metastatic lesions in the segment 5-6 30 months after an extended right colectomy and segment 5 metastasectomy. A second patient had a resectable liver metastasis in the segment 6 8 months following the combined left hemicolectomy and segment 3 metastasectomy. The third patient had multiple non-resectable metastases on a changed chemotherapy regimen, and the fourth patient had multiple liver and pulmonary metastases 36 months after the primary operation of sigmoid resection and left lateral sectionectomy with resection of the segment 4b. The main characteristics of patients with major hepatectomies are summarized in Table 1.
Go to : 
Colorectal carcinoma is a leading cause of mortality globally with 15-20% of patients having synchronous liver metastases at the time of their initial diagnosis.1415 Surgical treatments of synchronous liver metastases include several approaches: the “classic” approach with initial colorectal resection and adjuvant chemotherapy followed by liver resection; simultaneous resection with neo-adjuvant or adjuvant chemotherapy; and the “liver-first” (“reverse”) approach (with or without neo-adjuvant systematic chemotherapy), in which the primary tumor is removed at the last stage of treatment.
The optimal strategy remains open to discussion with markedly individualized approaches. Some authors recommend a staged approach because of reported higher levels of postoperative complications and mortality in synchronous operations.161718 In addition, disruption of protein synthesis by liver resection may lead to increased risk of infection and anastomosis insufficiency.19 Other factors which may have negative implications for combined resections are transient portal hypertension from application of the Pringle maneuver, and possible compromising the intestinal anastomosis due to edema,1820 in addition to inadequate exploration and insufficiently safe vascular control of the inferior vena cava and hepatic veins.18
A series of current publications including a meta-analysis, 21 support the advantage of simultaneous, open, combined resection of the colorectal and liver pathology over the conservative staged approach.212223 The selective clamping of the portal pedicle and rare use of the Pringle maneuver decrease the possibility for anastomosis complications.24 Another meta-analysis referred to the extent of the metastatic disease and indicated that the primary difference is in the criteria by which patients are selected for the combined approach or the staged approach. The staged approach demonstrates better results for intraoperative parameters, postoperative complications, and survival. The shorter hospital stay for simultaneous resections is associated with the lower tumor burden in these patients. In the absence of prospective studies comparing patients with similar tumor burdens, the conclusion is that the application of the simultaneous approach currently provides advantages only for patients with limited liver metastatic disease.25
The laparoscopic resection in colorectal carcinoma and the laparoscopic liver resection in malignant diseases, considered separately, are widely adopted and applicable therapeutic methods. The first randomized control study, the Oslo-CoMet Study, is presently ongoing. It is expected to provide level 1 of authenticity regarding the benefits and advantages of laparoscopic resection compared to open liver resection in cases of colorectal metastases. The comparative substantiated characteristics include 30-days postoperative morbidity, resection lines, postoperative pain, quality of life, inflammatory response, 5-year survival (general, disease-free and relapse-free), and “price-effectiveness”.26 With advances in laparoscopic surgery, the simultaneous resection of colorectal carcinoma with synchronous liver metastases is becoming a therapeutically interesting option. An increasing number of publications are indicating the feasibility of totally laparoscopic and “hand-assisted” approaches in selected patients.5 These publications emphasize the advantages of the low percentage of morbidity, short hospital stay and “price-effectiveness” correlation, as well as good short-term and longterm oncological outcomes.69 The small number of publications is related mainly to the technical difficulty of laparoscopic liver resection, as well as the lack of surgeons experienced in simultaneous laparoscopic colorectal and liver surgery. Some authors emphasize the need for a medical team with separate individuals having experience in colorectal and liver surgery for the successful application of this approach.724
One surgical department, which specialized in hepato-biliary and pancreatic surgery, also widely practiced laparoscopic colorectal surgery. Before beginning to perform simultaneous liver and colorectal laparoscopic resections, more than 100 separate laparoscopic liver and colorectal resections were performed. Expertise in performing separate resections contributes to the application and development of the combined resection method, improves the present surgical knowledge, and increases the eventuality of a single surgeon performing the combined surgical intervention. With advancements in the multimodal approach for treatment of colorectal carcinoma, life span of patients with colorectal carcinoma will gradually increase, with a probable need for subsequent, repeated surgical interventions.27 Indeed, one patient in this study was operated on for a second recurrence 30 months following an initial combined extended right hemicolectomy and segment 5 metastasectomy for synchronous colorectal metastases. R0-liver laparoscopic resection was achieved with no intraoperative or postoperative complications. The likelihood of repeated surgeries supports advancing the laparoscopic approach, and further indicates that planning individual therapeutic strategies for patients with synchronous liver metastases must be considered.28
A systematic analysis of combined laparoscopic colorectal and liver resections published in 2014 reported a total of 39 published cases including 9 (23%) major liver resections.3 A left lateral sectionectomy was performed in 26 (67%) of patients. The colorectal resections included anterior and low anterior rectal resections with a total mesorectal excision, right and left colectomies. Despite the absence of a high level of reliability, the combined laparoscopic procedures were determined to be feasible and safe, even those that included major liver resections. An appropriate selection of patients and adequate experience of the surgeon plays a key role for success. As an example of a routine combined intervention, the simultaneous colorectal resection with left lobectomy was suggested.3 Hoekstra et al.10 determined that patients with solitary, peripherally localized metastases in segment 2-6 (in correspondence with Louisville-consensus) were “ideal” candidates for simultaneous resection. Other studies also described colorectal resections and major liver resections with good intraoperative and early postoperative results.1112 Spampinato et al.11 reported three laparoscopic right hepatectomies and one left hepatectomy, combined respectively with simultaneous resections of the sigmoid colon (n=3) and one resection of the rectum. The average surgery time was 495 minutes with average postoperative hospital stay of 6 days. The average intraoperative blood loss was 465 ml (300-630 ml), and no postoperative complications and mortality were described. R0-resection was achieved in all patients. One liver recurrence was reported for an average follow-up period of of 14 months (7 to 20 months). Tranchart et al.28 reported a combined right hemicolectomy and right hepatectomy in a 36 year old female patient,and a resection of the sigmoid colon with left hepatectomy in a 78 year old male patient with a partial response to the neo-adjuvant therapy. The average surgery time was 317 minutes (310-345), and the average postoperative hospital stay - 5 days (4-6); no postoperative complications and mortality were reported. These authors emphasized that selective extra-hepatic vascular control is the key for minimal blood loss in performing parenchymal transsection and intestinal anastomosis with no initial portal hypertension or edema of the intestinal wall. Ferretti et al.13 in a multicenter study covering 142 synchronous laparoscopic colorectal and liver resections concluded that in experienced centers, the simultaneous laparoscopic approach is technically feasible, safe, and associated with good oncological outcomes.
In our study of laparoscopic simultaneous combined resections, primary colorectal localization was a criterion for inclusion. The patient selection was rather influenced by the possibility for resection, and the number and localization of liver lesions. Patients with solitary lesions, or up to three grouped metastases were preferred, however the evaluation was strictly individual. In the last patient, with multiple synchronous bilobar liver metastases, anterior resection of the rectum was performed (following neo-adjuvant therapy and clinically proved response). This was combined with metastasectomy in the third segment and ligation of the right branch of the portal vein with elective right hepatectomy after the achieved adequate hypertrophy of the future liver remnant. Similar cases additionally extend the indications for a laparoscopic approach in synchronous liver metastases originating from colorectal carcinoma.
In conclusion, the simultaneous colorectal and liver resection of different volumes is feasible in patients with primary colorectal carcinoma and synchronous colorectal metastases while following an optimal, individually adapted, multimodal approach, providing there is an adequate preoperative selection of patients, and sufficient experience and knowledge on the part of the surgeon. Performing prospective randomized studies is required in order to provide a basis for a consensus regarding the standard application of this therapeutic option.
Go to : 
References
1. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009; 250:825–830. PMID: 19916210.
2. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–629. PMID: 25742461.
3. Lupinacci RM, Andraus W, De Paiva Haddad LB, Carneiro D'Albuquerque LA, Herman P. Simultaneous laparoscopic resection of primary colorectal cancer and associated liver metastases: a systematic review. Tech Coloproctol. 2014; 18:129–135. PMID: 24057357.

4. Qiu J, Chen S, Pankaj P, Wu H. Laparoscopic hepatectomy is associated with considerably less morbidity and a long-term survival similar to that of the open procedure in patients with hepatic colorectal metastases. Surg Laparosc Endosc Percutan Tech. 2014; 24:517–522. PMID: 25187072.

5. Lee JS, Hong HT, Kim JH, Lee IK, Lee KH, Park IY, et al. Simultaneous laparoscopic resection of primary colorectal cancer and metastatic liver tumor: initial experience of single institute. J Laparoendosc Adv Surg Tech A. 2010; 20:683–687. PMID: 20687851.

6. Kim SH, Lim SB, Ha YH, Han SS, Park SJ, Choi HS, et al. Laparoscopic-assisted combined colon and liver resection for primary colorectal cancer with synchronous liver metastases: initial experience. World J Surg. 2008; 32:2701–2706. PMID: 18843442.

7. Polignano FM, Quyn AJ, Sanjay P, Henderson NA, Tait IS. Totally laparoscopic strategies for the management of colorectal cancer with synchronous liver metastasis. Surg Endosc. 2012; 26:2571–2578. PMID: 22437957.

8. Akiyoshi T, Kuroyanagi H, Saiura A, Fujimoto Y, Koga R, Konishi T, et al. Simultaneous resection of colorectal cancer and synchronous liver metastases: initial experience of laparoscopy for colorectal cancer resection. Dig Surg. 2009; 26:471–475. PMID: 20068319.

9. Hayashi M, Komeda K, Inoue Y, Shimizu T, Asakuma M, Hirokawa F, et al. Simultaneous laparoscopic resection of colorectal cancer and synchronous metastatic liver tumor. Int Surg. 2011; 96:74–81. PMID: 21675625.

10. Hoekstra LT, Busch OR, Bemelman WA, van Gulik TM, Tanis PJ. Initial experiences of simultaneous laparoscopic resection of colorectal cancer and liver metastases. HPB Surg. 2012; 2012:893956. PMID: 23082043.

11. Spampinato MG, Mandalá L, Quarta G, Del Medico P, Baldazzi G. One-stage, totally laparoscopic major hepatectomy and colectomy for colorectal neoplasm with synchronous liver metastasis: safety, feasibility and short-term outcome. Surgery. 2013; 153:861–865. PMID: 22853855.

12. Berti S, Francone E, Minuto M, Bonfante P, Sagnelli C, Bianchi C, et al. Synchronous totally laparoscopic management of colorectal cancer and resectable liver metastases: a single center experience. Langenbecks Arch Surg. 2015; 400:495–503. PMID: 25681240.

13. Ferretti S, Tranchart H, Buell JF, Eretta C, Patriti A, Spampinato MG, et al. Laparoscopic simultaneous resection of colorectal primary tumor and liver metastases: results of a multicenter international study. World J Surg. 2015; 39:2052–2060. PMID: 25813824.

14. Leung U, Gönen M, Allen PJ, Kingham TP, DeMatteo RP, Jarnagin WR, et al. Colorectal cancer liver metastases and concurrent extrahepatic disease treated with resection. Ann Surg. 2016; [in press].

15. Siriwardena AK, Mason JM, Mullamitha S, Hancock HC, Jegatheeswaran S. Management of colorectal cancer presenting with synchronous liver metastases. Nat Rev Clin Oncol. 2014; 11:446–459. PMID: 24889770.

16. Bolton JS, Fuhrman GM. Survival after resection of multiple bilobar hepatic metastases from colorectal carcinoma. Ann Surg. 2000; 231:743–751. PMID: 10767796.

17. Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Française de Chirurgie. Cancer. 1996; 77:1254–1262. PMID: 8608500.
18. Belghiti J. Synchronous and resectable hepatic metastases of colorectal cancer: should there be a minimum delay before hepatic resection? Ann Chir. 1990; 44:427–429. PMID: 2221787.
19. Kimura F, Miyazaki M, Suwa T, Kakizaki S, Itoh H, Kaiho T, et al. Reduced hepatic acute-phase response after simultaneous resection for gastrointestinal cancer with synchronous liver metastases. Br J Surg. 1996; 83:1002–1006. PMID: 8813800.

20. Jaeck D, Bachellier P, Weber JC, Boudjema K, Mustun A, Pâris F, et al. Surgical strategy in the treatment of synchronous hepatic metastases of colorectal cancers. Analysis of a series of 59 operated on patients. Chirurgie. 1999; 124:258–263. PMID: 10429299.
21. Chen J, Li Q, Wang C, Zhu H, Shi Y, Zhao G. Simultaneous vs. staged resection for synchronous colorectal liver metastases: a metaanalysis. Int J Colorectal Dis. 2011; 26:191–199. PMID: 20669024.

22. Belev N, Takorov I, Dimov P, Vladov N, Penov V. Aggressive surgery in the multimodality treatment of liver metastases from colorectal cancer. J BUON. 2007; 12:209–213. PMID: 17600874.
23. Brouquet A, Mortenson MM, Vauthey JN, Rodriguez-Bigas MA, Overman MJ, Chang GJ, et al. Surgical strategies for synchronous colorectal liver metastases in 156 consecutive patients: classic, combined or reverse strategy? J Am Coll Surg. 2010; 210:934–941. PMID: 20510802.

24. Hillingsø JG, Wille-Jørgensen P. Staged or simultaneous resection of synchronous liver metastases from colorectal cancer--a systematic review. Colorectal Dis. 2009; 11:3–10. PMID: 18637099.
25. Slesser AA, Simillis C, Goldin R, Brown G, Mudan S, Tekkis PP. A meta-analysis comparing simultaneous versus delayed resections in patients with synchronous colorectal liver metastases. Surg Oncol. 2013; 22:36–47. PMID: 23253399.

26. Fretland ÅA, Kazaryan AM, Bjørnbeth BA, Flatmark K, Andersen MH, Tønnessen TI, et al. Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet Study): study protocol for a randomized controlled trial. Trials. 2015; 16:73. PMID: 25872027.

27. Champagne BJ, Delaney CP. Laparoscopy for metastatic colorectal cancer. Surg Oncol. 2007; 16:15–24. PMID: 17548191.

28. Tranchart H, Diop PS, Lainas P, Pourcher G, Catherine L, Franco D, et al. Laparoscopic major hepatectomy can be safely performed with colorectal surgery for synchronous colorectal liver metastasis. HPB (Oxford). 2011; 13:46–50. PMID: 21159103.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download