This article has been
cited by other articles in ScienceCentral.
Abstract
Backgrounds/Aims
The roles of portal hypertension (PHT) on the postoperative course after hepatectomy are still debated. The aim of this study was to evaluate surgical outcomes of hepatectomy in patients with PHT.
Methods
Data from 152 cirrhotic patients who underwent hepatectomy for hepatocellular carcinoma (HCC) were collected retrospectively. Patients were divided into two groups according to the preoperative presence of PHT as follows: 44 patients with PHT and 108 without PHT. Propensity score matching (PSM) analysis was used to overcome selection biases.
Results
There were no significant differences in morbidity (56.8% vs. 51.9%, p=0.578) and 90-days mortality (4.5% vs. 4.6%, p=0.982) between the two groups. Post-hepatectomy liver failure (PHLF) was not significantly different between the two groups (43.2% vs. 35.2%, p=0.356). Patients without PHT had a better 5-year disease-free survival than those with PHT, although the difference did not reach statistical significance (30.9% vs. 17.2%, p=0.081). Five-year overall survivals were not significantly different between the two groups (46.6% vs. 54.9%, p=0.724). Repeat analyses after PSM showed similar rates of morbidity (p=0.819), mortality (p=0.305), PHLF (p=0.648), disease-free survival (p=0.241), and overall survival (p=0.619). The presence of PHT was not associated with either short-term or long-term poor surgical outcomes.
Conclusions
Child-Pugh A and B patients with PHT have surgical outcomes similar to those without PHT. Hepatectomy can be safely performed and can also be considered as a potentially curative treatment in HCC patients with PHT.
Go to :

Keywords: Portal hypertension, Hepatocellular carcinoma, Hepatectomy, Complication, Prognosis
INTRODUCTION
The outcomes of hepatectomy in hepatocellular carcinoma (HCC) have improved greatly because of remarkable advances in surgical techniques and perioperative care. Adequate assessment of preoperative hepatic functional reserve and tailoring the extent of hepatectomy to hepatic functional reserve has reduced postoperative mortality and morbidity rates.
1 Thus, evaluation of the hepatic functional reserve is a key point in the therapeutic management of these patients.
2
Architectural and dynamic alterations of the liver due to the progression of cirrhosis lead to splanchnic vasodilation and an increase in portal blood flow, and ultimately the development of portal hypertension (PHT).
3 PHT significantly increases the risk of complications in liver resections. However, direct measurements of preoperative portal venous pressure (PVP) have not been done routinely because of several limitations including invasiveness. Usually, indirect criteria of PHT such as esophageal varix and/or splenomegaly associated with thrombocytopenia are used instead to identify poor candidates for liver resection.
34
The present study evaluated the effects of PHT on hepatectomy retrospectively through the comparison of short- and long-term surgical outcomes in patients with HCC and cirrhosis with or without PHT.
Go to :

MATERIALS AND METHODS
This study included 170 patients with compensated cirrhosis and HCC who received hepatectomy in our hospital between January 2001 and December 2010. Of these 170 patients, 152 patients who underwent curative hepatectomy as their initial treatment were selected and were divided into groups according to the presence of PHT.
Because portal venous pressure is not routinely measured directly, PHT was defined as present when patients had detectable esophageal varices on endoscopy or splenomegaly (diameter greater than 12 cm) with a platelet count less than 100,000/mm
3, according to the Barcelona Clinic Liver Cancer group criteria.
5
Clinical evaluation and routine biochemical tests were performed perioperatively. Laboratory tests included platelet count, (AST), alanine aminotransferase (ALT), prothrombin time (PT), albumin, total bilirubin, alkaline phosphatase (ALP), and indocyanine green retention rate at 15 min (ICG-R15).
Major hepatectomy was classified as the resection of two or more Couinaud sections, and minor hepatectomy as the resection of fewer than two sections.
Post-hepatectomy liver failure (PHLF) was classified according to definitions of the International Study Group of Liver Surgery (ISGLS). In brief, the ISGLS definition of PHLF is increased INR and hyperbilirubinemia on or after postoperative day 5. If INR or serum bilirubin concentration is increased preoperatively, PHLF is defined as an increasing INR (decreasing prothrombin time) and increasing serum bilirubin concentration on or after postoperative day 5 compared with the values of the previous day.
6
Mortality was defined as death within 90 days of surgery. After surgery, all patients underwent follow-up every 3-6 months. The median follow-up of the 152 patients was 56.5 (1-171) months.
Statistical analysis
Data were analyzed with SPSS statistical software (SPSS version 23.0). The differences between categorical variables were analyzed with the chi-squared test or Fisher's exact test. Continuous variables were compared between groups by the unpaired t-test or Mann-Whitney U-test, as appropriate. The overall and disease-free survival was calculated using the Kaplan-Meier method, and their comparison was performed using the log-rank test. The multivariate analysis was performed using a logistic regression analysis. A p-value<0.05 was considered significant.
Propensity score matching (PSM) was used to overcome patient selection bias and to achieve an even distribution of baseline liver function. PSM analysis was conducted using logistic regression to create propensity scores for HCC patients with or without PHT.
7 The propensity score model was generated using potential covariates that could affect clinical characteristics including age, gender, hepatic serology, Child-Pugh class, ALT, AST, albumin, bilirubin, prothrombin time, ICG-R15, tumor size, tumor number, extent of hepatectomy, and stage. The one-to-one nearest-neighbor matching method was used to generate pairs of patients with and without PHT. After PSM, 78 patients were included for further analysis (39 matched pairs of patients) (
Fig. 1).
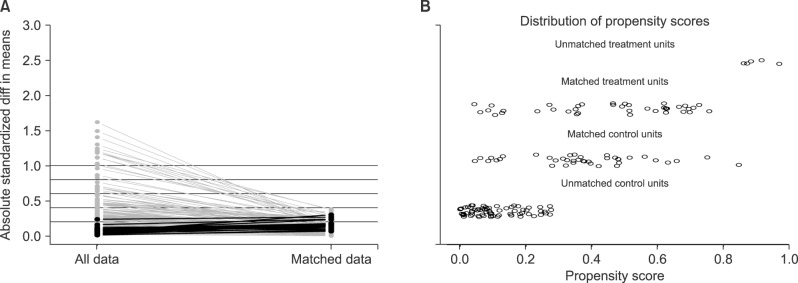 | Fig. 1Propensity score matching (PSM) process. (A) Parallel line plot of the standardized difference in means before and after PSM in hepatocellular carcinoma patients with and without portal hypertension (PHT). As the standardized difference in means was reduced, the covariate balance was improved in the matched samples. (B) Dot plot of the propensity scores of patients in the PHT and the non-PHT groups showing individual units in the dataset and whether they were matched or discarded.
|
Go to :

RESULT
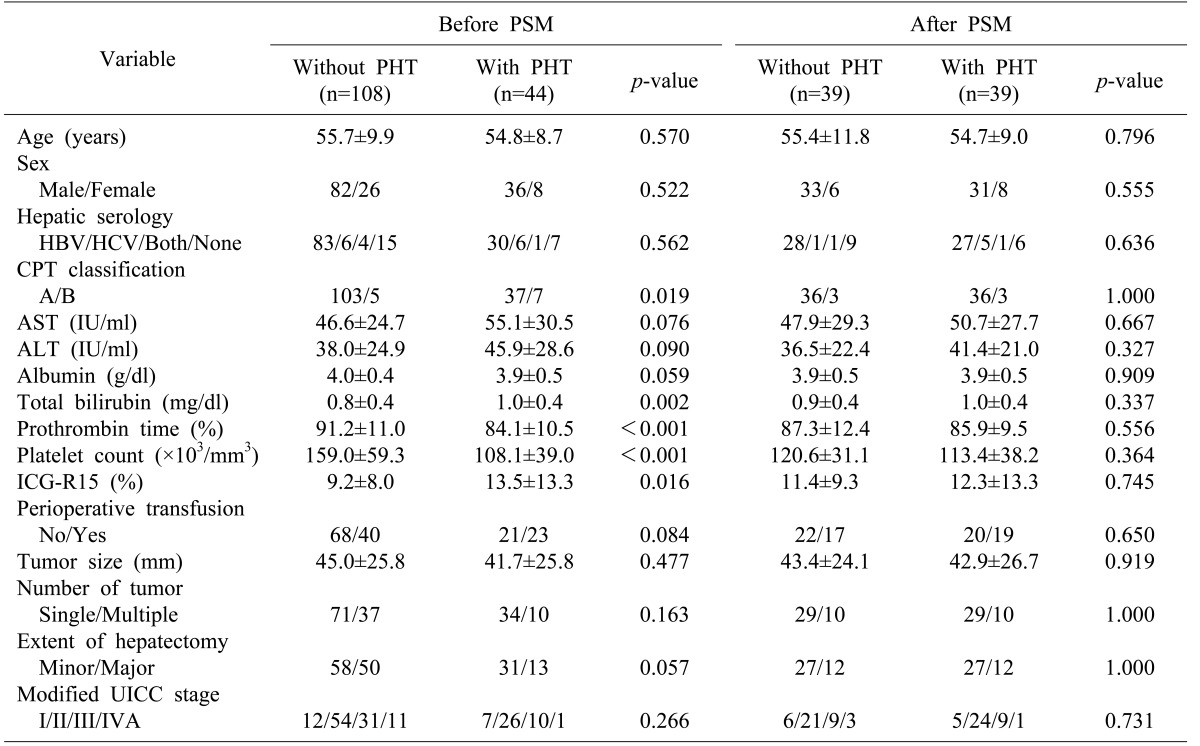
Patient profiles
Among the 152 patients enrolled in this study, 44 patients (29.0%) were preoperatively found to have clinically significant PHT. The baseline characteristics of the study population with HCC according to the presence of PHT are summarized in
Table 1.
Table 1
Clinical characteristics of patients with hepatocellular carcinoma and compensated liver cirrhosis who underwent hepatectomy
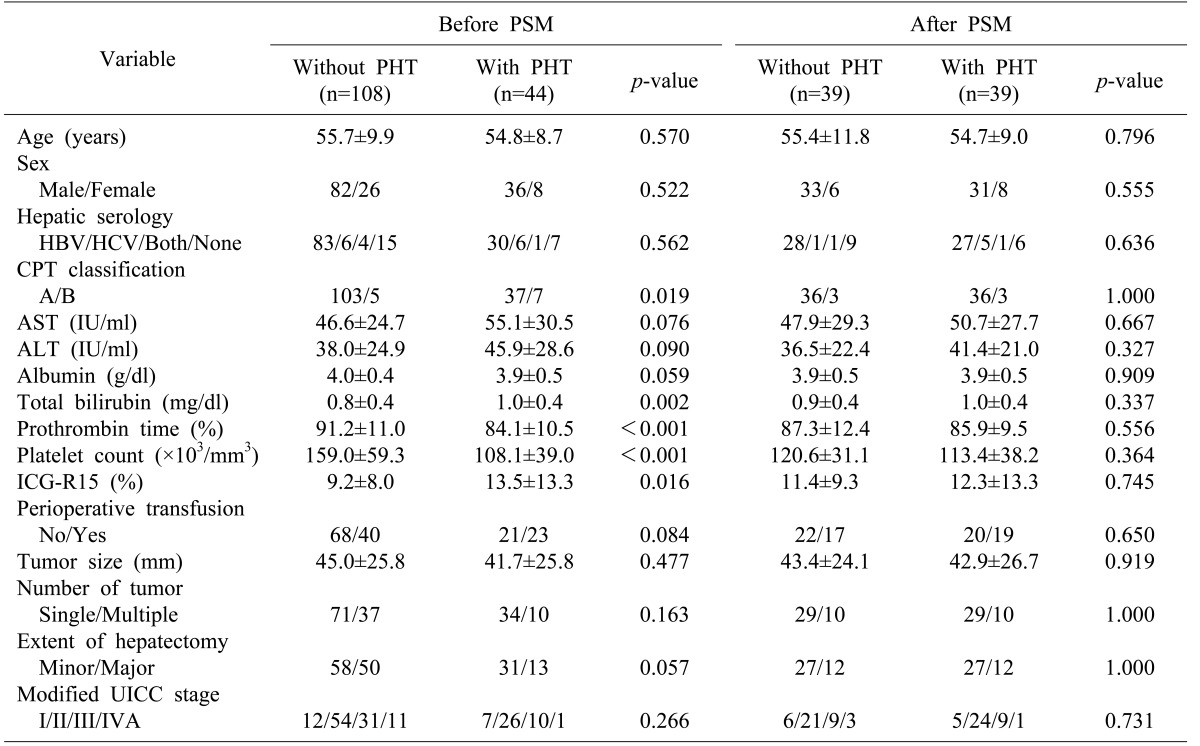

Patients with PHT had worse liver function and received less extensive resection compared to those without PHT. Patients with PHT had lower platelet counts (108.1 vs. 159.0;
p<0.001), lower percentages of prothrombin time (84.1% vs. 91.2%,
p<0.001), higher concentrations of total bilirubin (1.0 vs. 0.8,
p=0.002), higher frequencies of Child-Pugh class B (15.9 vs. 5.6,
p=0.019), and higher percentages of ICG-R15 (13.5 vs. 9.2,
p=0.016). Also, patients with PHT have lower concentrations of albumin (3.9 vs. 4.0,
p=0.059), higher concentrations of AST (55.1 vs. 46.6,
p=0.076), higher concentrations of ALT (45.9 vs. 38.0,
p=0.090), and higher frequencies of minor resection (70.5% vs. 53.0,
p=0.057) but the differences were not statistically significant (
Table 1).
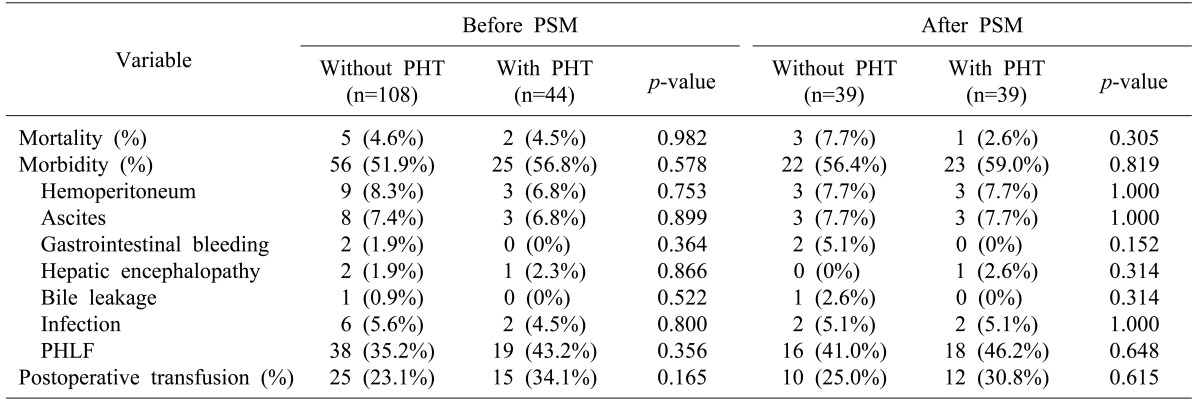
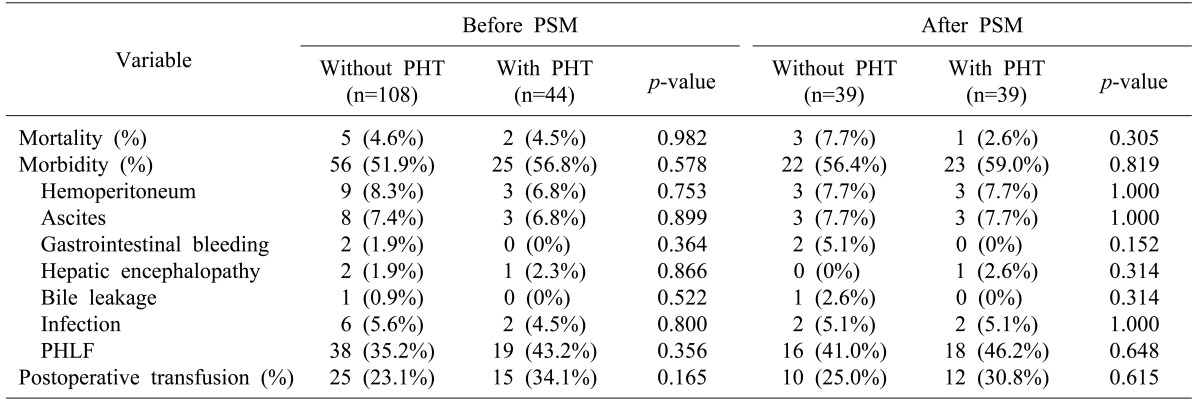
Short-term results
Of the 152 patients who underwent hepatectomy, 81 (53.3%) had postoperative complications. Of the 44 patients with PHT, 25 (56.8%) developed complications after hepatectomy, including hemoperitoneum in 3 (6.8%), ascites in 3 (6.8%), hepatic encephalopathy in 1 (2.3%), infection in 2 (4.5%), and PHLF in 19 (43.2%). Fifty-six patients (51.9%) without PHT also developed complications, with hemoperitoneum in 9 (8.3%), ascites in 8 (7.4%), gastrointestinal bleeding in 2 (1.9%), hepatic encephalopathy in 2 (1.9%), bile leakage in 1 (0.9%), infection in 6 (5.6%), and PHLF in 38 (35.2%). Two of the 44 patients with PHT (4.5%) and 5 of the 108 patients without PHT (4.6%) died within 90 days after hepatectomy. There were no significant differences in postoperative morbidity (
p=0.578) and mortality (
p=0.982) rates between the two groups. In particular, PHLF was not significantly different between the two group (
p=0.356) (
Table 2).
Table 2
Postoperative complications in hepatocellular carcinoma patients with or without PHT, before and after PSM

Long-term results
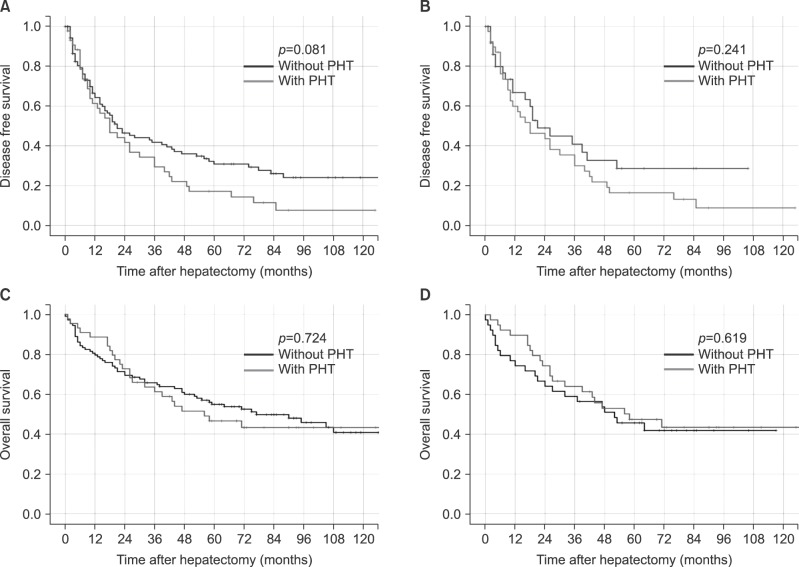
The mean follow-up of the 152 patients was 57.1±41.6 months. Recurrence developed after hepatectomy in 37 (84.1%) patients with PHT and in 69 (63.9%) patients without PHT. Patients without PHT had better disease-free survival than those with PHT, although the difference was not statistically significant (p=0.081). One, 3 and 5 year disease-free survival rates in patients with PHT were 61.3%, 29.4%, and 17.2% respectively, versus 64.3%, 41.8%, and 30.9% respectively in those without PHT.
During the follow-up period, 24 patients with PHT (54.5%) died, compared to 57 patients without PHT (52.8%). Survival rates of 1, 3, and 5-years were 88.6%, 61.2%, 46.6% in the PHT group and 79.6%, 65.7%, 54.9% in the non-PHT group respectively. There was no significant difference in survival between the two groups (
p=0.724) (
Fig. 2).
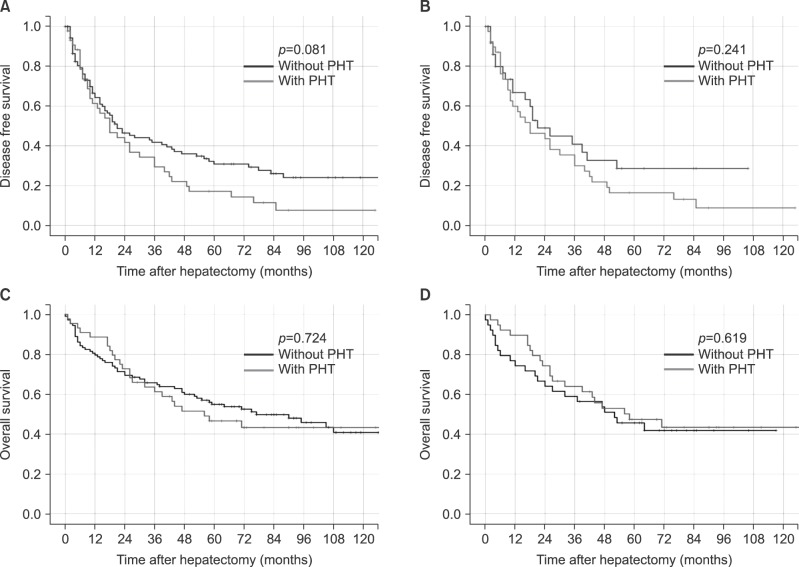 | Fig. 2Kaplan-Meier survival curves of the population undergoing hepatectomy for hepatocellular carcinoma with and without portal hypertension (PHT). (A) and (B) show disease-free survival before and after propensity score matching, respectively. (C) and (D) show overall survival before and after propensity score matching, respectively (blue line, without PHT; and green line, with PHT).
|
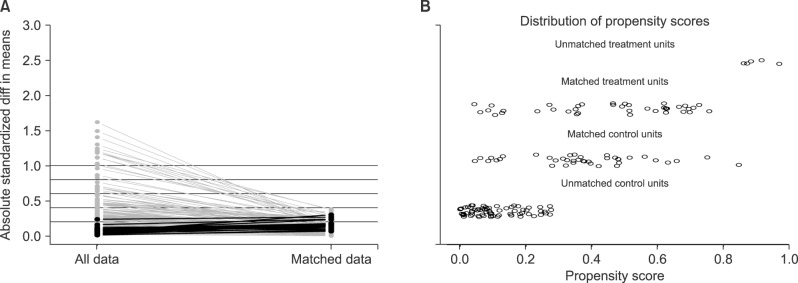
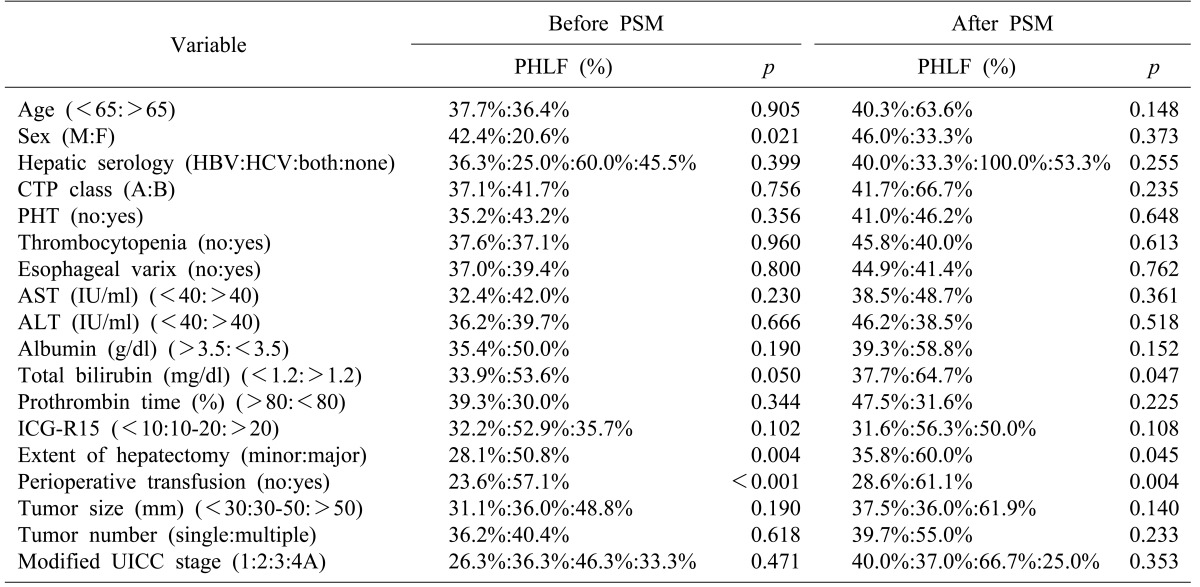
Predictive factors of PHLF according to the definition of ISGLS
According to the univariate analysis, the statistically significant factors related to PHLF were male gender (
p=0.021), total bilirubin of 1.2 mg/dl or greater (
p=0.05), major hepatectomy (
p=0.004), and perioperative transfusion (
p<0.001). However, there was no difference in PHLF with respect to the presence of PHT (
p=0.356) (
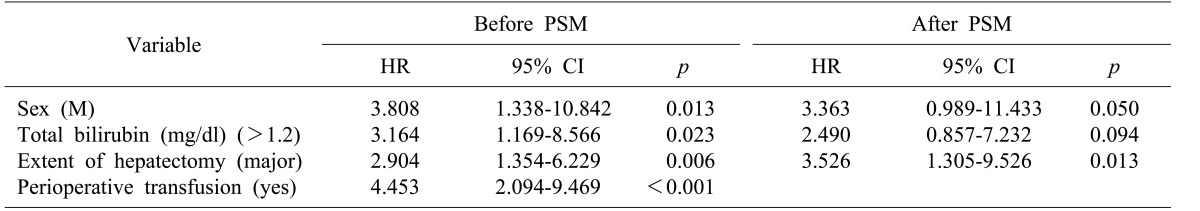
Table 3). A multivariate analysis based on the significant variables in the univariate analysis also indicated that male gender (Hazard ratio (HR): 3.808; 95% Confidence interval (CI): 1.338-10.842;
p=0.013), total bilirubin of 1.2 mg/dl or greater (HR: 3.164; 95% CI: 1.169-8.566;
p=0.023), major hepatectomy (HR: 2.904; 95% CI: 1.354-6.229;
p=0.006), and perioperative transfusion (HR: 4.453; 95% CI: 2.094-9.469;
p<0.001) were independent predictive factors for PHLF (
Table 4).
Table 3
Univariate analysis of predictive factors of PHLF
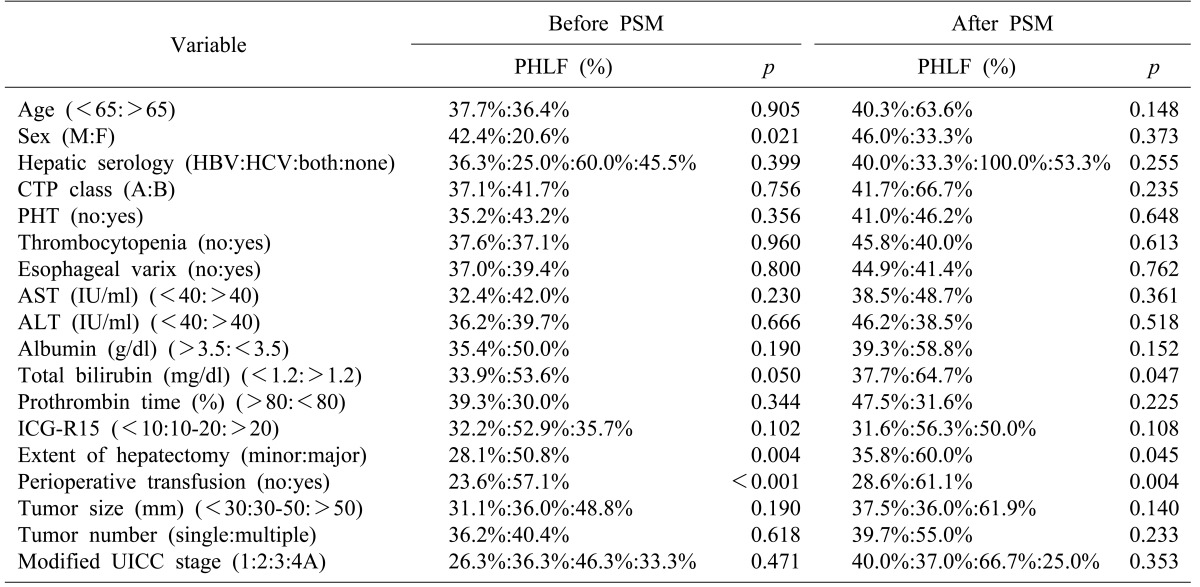

Table 4
Multivariate analysis of predictive factors of post-hepatectomy liver failure
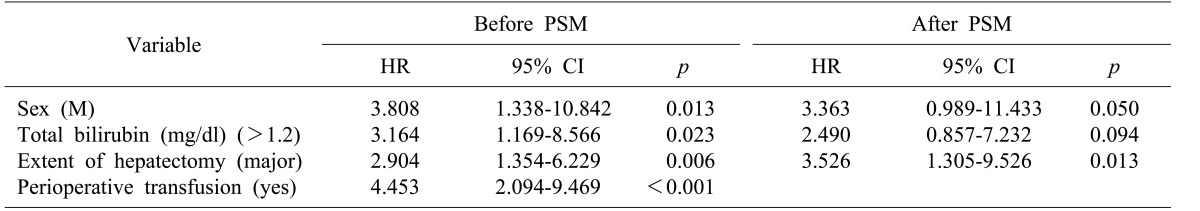

Analysis of the matched sample
After the one-to-one PSM, 78 patients were selected for comparison: 39 were assigned to the PHT group and an equal number to the non-PHT group (
Fig. 1). As can be observed in
Table 1, clinical characteristics were generally similar in both groups after PSM.
The postoperative complications after PSM are shown in
Table 2. No significant difference in postoperative complications was found between the two groups. The patients with PHT and without PHT had similar morbidity (59.0% vs. 56.4%,
p=0.819) and 90-day mortality (2.6% vs. 7.7%,
p=0.305). In particular, both groups had similar PHLF rates (30.8% vs. 25.0%,
p=0.615) regardless of the presence of PHT.
The matched patients without PHT also had better disease-free survivals compared to those with PHT, although the difference did not reach statistical significance (
p=0.241). One, 3 and 5 year disease-free survival rates in the patients with PHT were 59.8%, 29.9%, and 16.3%, respectively compared to 66.7%, 40.8%, and 28.5%, respectively, in those without PHT. Survival was not significantly different between patients with or without PHT at 1 year (89.7% vs. 74.6%), 3 years (64.0% vs. 59.0%), and 5 years (47.4% vs. 45.7%) (
p=0.619) (
Fig. 2).
Among the variables in univariate analysis, total bilirubin of 1.2 mg/dl or greater (
p=0.047), major hepatectomy (
p=0.045), and perioperative transfusion (
p=0.004) were identified as independent predictive factors for PHLF. In contrast, PHT was not confirmed as an independent predictive factor (
p=0.648). The logistic regression results on PHLF are shown in
Table 4. Total bilirubin of 1.2 mg/dl or greater (HR: 3.363; 95% CI: 0.989-11.433;
p=0.05) and perioperative transfusion (HR: 3.526; 95% CI: 1.305-9.526;
p<0.001) were identified as independent predictive factors for PHLF. In contrast, PHT was not confirmed as an independent predictive factor. The extent of hepatectomy also was not identified as a predictor for PHLF in the post-PSM logistic regression analysis.
Go to :

DISCUSSION
The outcome of liver resection in cirrhotic patients with HCC has improved greatly with better surgical techniques and perioperative care, and also because of more careful patient selection.
89101112 Liver resection is widely accepted as an oncologically effective treatment for HCC. However, cirrhotic patients with PHT often are not candidates for liver resection.
Bruix and Llovet evaluated the role of direct preoperative measurement of portal venous pressure to predict the outcome after liver resection in patients with cirrhosis.
213 These studies reported that a hepatic venous pressure gradient (HVPG) of 10 mmHg or more was a predictive factor for postoperative liver decompensation, and that PHT and the serum bilirubin level were associated with poor long-term survival. As a result of these studies, the European Association for the Study of the Liver/American Association for the Study of Liver Diseases considered PHT as a contraindication for liver resection.
1415 However, preoperative HVPG is not routinely applied in practice because of invasiveness. Therefore, indirect criteria of PHT (esophageal varix and/or splenomegaly associated with thrombocytopenia) are usually used instead of direct measurement of portal pressure. The impact of indirect criteria of PHT on postoperative short- and long-term results has not been confirmed, and several studies have reported contradictory results.
A report on predictors of short-term outcomes in a series of 1056 consecutive hepatectomies without mortality by Imamura et al.
16 indicated that PHT did not influence the overall postoperative complications in patients with HCC. Capussotti et al.
17 reported that Child A cirrhotic patients (n=66) have similar short- and long-term outcomes compared to patients without PHT. Similarly, Cucchetti et al.
18 reported that 241 patients who underwent resection for HCC experienced the same intraoperative course, postoperative occurrence of hepatic failure, morbidity, length of in-hospital stay and survival rates. They concluded that the presence of PHT should not be considered as a contraindication for hepatic resection in cirrhotic patients. Kawano et al.
19 analyzed surgical outcomes in 131 cirrhotic patients and found that 31 patients with esophageal varices had similar outcomes as the 100 patients without esophageal varices. Therefore, we suggest that the recommendation made in the guideline that PHT should be a contraindication for liver resection is not appropriate for all patients because the prognostic role of PHT after resection in patients with HCC is still unclear.
In the present retrospective study, univariate and multivariate analyses showed that the presence of PHT had no impact on postoperative complications, PHLF, and survivals. In matched samples, there was no significant difference in disease-free survivals of patients without PHT compared to those with PHT (p=0.241). The 1 year, 3 year and 5 year disease-free survival rates in patients with PHT were 59.8%, 29.9%, and 16.3%, respectively versus 66.7%, 40.8%, and 28.5%, respectively in those without PHT. Survival rates were similar between patients with PHT and without PHT at 1 year (89.7% vs. 74.46%), 3 years (64.0% vs. 59.0%), and 5 years (47.4% vs. 45.7%) (p=0.619).
Before PSM, male gender (HR: 3.808; 95% CI: 1.338-10.842; p=0.013), total bilirubin of 1.2 mg/dl or greater (HR: 3.164; 95% CI: 1.169-8.566; p=0.023), major hepatectomy (HR: 2.904; 95% CI: 1.354-6.229; p=0.006), and perioperative transfusion (HR: 4.453; 95% CI: 2.094-9.469; p<0.001) were identified as independent predictive factors for PHLF, regardless of PHT. When other variables were evenly distributed by PSM, total bilirubin of 1.2 mg/dl or greater (HR: 3.363; 95% CI: 0.989-11.433; p=0.05) and perioperative transfusion (HR: 3.526; 95% CI: 1.305-9.526; p<0.001) were identified as independent predictive factors for PHLF. In contrast, PHT was not confirmed as an independent predictive factor.
Major hepatectomy was not identified as a predictor for PHLF in the post-PSM logistic regression analysis, although the extent of hepatectomy was associated with PHLF in the logistic regression analysis before PSM. Finally, prognostic variables that significantly affected PHLF were an elevated total bilirubin level and perioperative transfusion. We recommend selecting patients with PHT carefully when there is a need for extensive resection to achieve a curative treatment, especially when the total bilirubin level is elevated. In order to decrease the need or amount of perioperative transfusion, meticulous surgical methods and close cooperation with the anesthetic team to minimize blood loss should be recommended. Thus, selected patients with compensated liver cirrhosis, even with PHT, could have favorable long term results.
In conclusion, portal hypertension has been reported as a negative prognostic factor and a contraindication to liver resection. However, in this study, Child-Pugh class A and B patients with PHT have short- and long-term surgical outcomes similar to those without PHT. The presence of PHT was not an independent factor for poor surgical outcomes. Total bilirubin level and perioperative transfusion were the factors related to PHLF. Therefore, hepatectomy can be safely performed and also considered as a potentially curative treatment in HCC patients with PHT and compensated liver cirrhosis.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download