Methanol poisoning can cause neurological complications, including visual disturbances (
1), bilateral putaminal hemorrhagic necrosis (
2), parkinsonism (
3), cerebral edema, coma, or seizures (
4). Therefore, methanol has strictly restricted use, with reference values of Biological Exposure Indices (BEI) intended as guidelines for evaluation of potential hazards (
5). Methanol poisoning cases were reported as being mainly due to accidental oral ingestion (
67) including suicidal attempts (
8). However, recently there have been outbreaks of methanol poisoning via non-oral exposure at industrial sites in Korea (
910). Besides, a hazard issue has been raised about methanol in automobile washer in Korea (
11). We present in this study 3 patients who had severe neurological complications resulting from methanol poisoning via non-oral exposure in the electronics industry.
The first patient was a 27-year-old woman who was admitted in January 2016 with sudden onset dyspnea. The day before admission, she complained of visual dimness in both eyes and severe nausea. She had no past medical or drug history. Additional occupational history included getting a job in a cellular phone factory at the end of September 2015, in Bucheon, where she removed alcohol-smelling solvent and dust on the surface of raw material using an air-gun. Her initial mental state was alert and her vital signs were stable except for hyperventilation. However, her mental state rapidly worsened to drowsiness. Laboratory findings indicated metabolic acidosis with respiratory compensation (
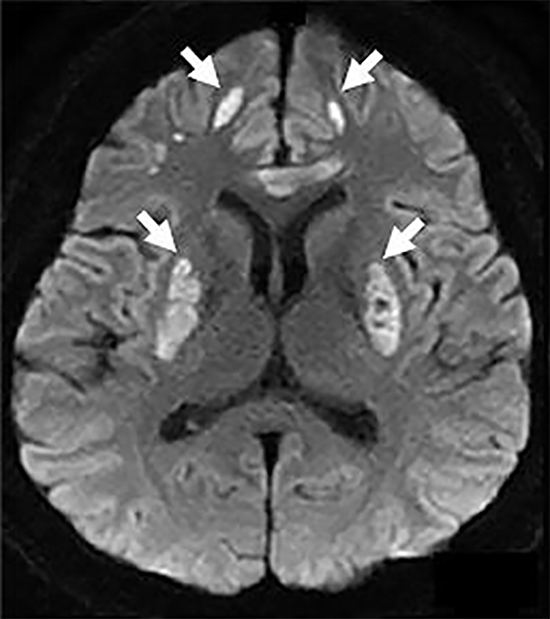
Table 1). Because of rapidly worsening mental status to drowsiness and uncontrolled metabolic acidosis despite medical treatment of intravenous bicarbonate, she was intubated and admitted in intensive care unit, and hemodialysis was performed. Brain magnetic resonance image (MRI) showed abnormal signal intensity in the bilateral putamen and insular cortices (
Fig. 1A, 1B, and 1C). Toxin analysis from collected urine disclosed methanol concentration of 7.632 mg/L (BEI guideline is concentration of 15 mg/L of methanol in urine at the end of shift) (
5); however, this was collected after two rounds of hemodialysis. Workplace inspection revealed that 99.9% methanol was used to cool down the phone parts. Randomly collected air samples from 5 spots in this factory were found to contain methanol in the range of 1,030.1 ppm to 2,220.5 ppm, which exceeded the industrial threshold limit value (Time Weighted Average [TWA] 200 ppm; Short Term Exposure Limits [STEL] 250 ppm) (
10)
. In addition, protection devices including masks and gloves were not provided, and the exhaust ventilation system was not operated.
Although her mental state became alert on the fourth day after admission, she complained of persistent blurred vision in both eyes. Her visual acuity test showed finger counting at 20 cm for her right eye and at 30 cm for her left eye. Her color vision test showed 0/24 for her right eye and 2/24 for her left eye. Fundus examination (
Fig. 2A and 2B) and optical coherence tomography (OCT) indicated both optic nerves were edematous. In addition, she manifested hypomimia, hypophonia, monotonous and slurred speech, bradykinesia, and truncal ataxia (
Supplementary Video 1). Her neurologic sequelae were not improved when discharged on the tenth day after admission. At outpatient clinic, 22 days after symptoms onset, she manifested markedly improved vision, facial expression, speech, and bradykinesia, but still had truncal ataxia (
Supplementary Video 2).
The second patient was a 28-year-old woman who was admitted in February 2016 with acute mental changes. The day before admission, she complained of visual dimness in both eyes, and the next day presented disorientation. She had been working at a small cellular phone factory in Incheon for 6 days.
Her initial mental state was drowsy and vital signs were stable except for tachypnea with metabolic acidosis (
Table 1). Because of unrecovered metabolic acidosis despite medical treatment, she was admitted in intensive care unit and continuous renal replacement therapy (CRRT) was performed. Despite improved metabolic acidosis with CRRT treatment, she showed stuporous mentality on the third day after admission. Spinal tapping was performed and showed negative results. As electroencephalography (EEG) suggested non-convulsive status epilepticus (
Table 1), intravenous loading dose of antiepileptic drug was administered. Brain MRI showed abnormal signal intensity in the bilateral putamen and frontal cortices (
Fig. 1D, 1E, and 1F). It turned out that similar to the first patient, she worked in removing alcohol-smelling solvent and dust using an air-gun, and she poured the solvent into drums. Toxin analysis from collected urine disclosed methanol concentration of 0.813 mg/L; however, it was collected after CRRT for 2 days. Workplace inspection revealed 99.9% methanol was used to cool the phone parts. In addition, workers used methanol without proper protectors.
Although her mental state became alert on the tenth day after admission, she manifested hypophonia, prominent bradykinesia, and gait ataxia. Her mini mental state examination score was 22/30 due to decreased attention and orientation. In addition, she was unable to see the shape of objects in front of her, read letters, or count fingers. Fundus examination revealed bilateral optic atrophy (
Fig. 2C and 2D). Her parkinsonian symptoms were responsive to dopaminergic agents. However, her vision loss was not improved even when she was discharged 1 month later.
The third patient was a 25-year-old man who was admitted in December 2015 with acute mental change on the day of admission. Before admission, he had been working in another small cellular phone factory in Bucheon for 9 days. He also worked removing alcohol-smelling solvent and dust on the surface of cellular phone parts using an air-gun. His initial mental state was comatose and laboratory findings indicated metabolic acidosis with respiratory compensation (
Table 1). He manifested anisocoric pupil size and no direct pupillary light reflex in his left eye, but with preserved indirect light reflex. In the emergency room, he showed generalized tonic-clonic seizure for a few minutes. Because of comatous mentality and unrecovered metabolic acidosis, he was intubated and admitted in intensive care unit, and CRRT was performed. Workplace inspection revealed 99.9% methanol was used to cool the phone parts without proper personal protectors. Randomly collected air samples in the factory contained methanol in the range of 228.5 to 417.7 ppm.
Although the alertness recovered on the fourth day after admission, his awareness was impaired. Fundus examination (
Fig. 2E and 2F) and OCT showed bilateral optic atrophy. Visual evoked potential demonstrated no potential in his left eye and poor wave forms in his right eye. At outpatient clinic, 1 month later, he still expressed consistent inattention and was only capable of obeying a 1-step command. He did not express any interests, was not toilet-trained, and required assistance for eating. Frontal release signs were present. Brain MRI showed abnormal signal intensity in the bilateral putamen, frontal and insular cortices and subcortices (
Fig. 1G, 1H, and 1I).
These 3 patients were poisoned by methanol via inhalation or dermal exposure in 3 different cellular phone parts manufacturing factories. There was no doubt that all 3 patients were not poisoned by oral ingestion. Contrast to several previous reports that proposed inhalational methanol poisoning was rare and at low risk for complications of visual disturbances (
1213), the presented cases and other reports documented severe complications including vision loss and comatose mentality (
1415). All 3 presented patients showed optic atrophy, mental changes, ataxia or parkinsonism, and bilateral putaminal necrosis as complications resulting from methanol poisoning (
Table 1).
Moreover, workplace inspections revealed that 99.9% methanol was used to cool phone parts because the price was approximately 1/3 of ethanol's (
7) and proper protectors were not provided in all 3 factories. In addition, excessive levels of methanol were detected in air samples of the first and third factories. Air sample in the second factory was not collected because methanol was replaced by ethanol before the workplace inspection. In the first and second patients, the amount of methanol in urine was below BEI, however, we have to consider the fact that samples were collected after hemodialysis and CRRT, respectively.
Two more workers were identified presenting visual loss at the factory the first patient worked in, where the total number of workers was 29, and above half of them suffered from relatively minor symptoms such as headache, eye pain, or skin trouble. Through inspection, no significant differences about workplace and personal protection were recognized between those with and without severe complications in each factory. The different degree of individual occupational exposure can be related to why a few workers showed prominent severe complications. It also might be related to an individual difference in sensitivity to methanol (
16) that may be due to decreased hepatic folate stores (
17), or some genetic defect in formate-metabolizing enzymes or in producing transporters in the kidneys (
18).
One of the most common neurological symptoms of methanol poisoning is visual disturbance, ranging from the dimming or blurring of vision to permanent blindness (
1). Our 3 patients showed different severities of visual dimming and bilateral optic atrophy during the follow up examinations.
Methanol poisoning mainly via oral ingestion is known to cause bilateral putaminal hemorrhagic necrosis, although it can extend to adjacent white matter and other brain regions (
2). As in the presented cases, poisoning via non-oral ingestion also resulted in bilateral putamen lesions on MRI images, with putaminal hemorrhagic necrosis in the second and third patients (
Fig. 1). The third patient, probably due to the extensive lesions in the bilateral frontal lobe, manifested frontal release signs and frontal lobe dysfunction. Parkinsonism has been reported (
3) as a neurological sequela of acute methanol poisoning, and severe degrees of poisoning are associated with cerebral edema, coma, or seizures (
4). The first patient suffered from truncal ataxia, whereas the second patient manifested parkinsonism that was relieved by dopaminergic agents. We could find non-convulsive status epilepticus by EEG in the second patient and generalized convulsive seizure event in the third patient (
Table 1).
These cases presented severe neurological complications resulting from industrial outbreaks of methanol poisoning via inhalation and dermal exposure. Indeed, methanol poisoning via non-oral exposure can cause severe neurologic complications as presented above. In order to manage methanol poisoning adequately, as well as to prevent it, it should be recognized promptly by physicians.
Ethics statement
The study protocol was approved by the Institutional Review Board of Ewha Womans University Mokdong Hospital (IRB No. 2016-07-060). Informed consent was confirmed (or waived) by the IRB.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download