1. Freour T, Masson D, Mirallie S, Jean M, Bach K, Dejoie T, Barriere P. Active smoking compromises IVF outcome and affects ovarian reserve. Reprod Biomed Online. 2008; 16:96–102.
2. Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998; 13:1532–1539.
3. Crha I, Hrubá D, Fiala J, Ventruba P, Záková J, Petrenko M. The outcome of infertility treatment by in-vitro fertilisation in smoking and non-smoking women. Cent Eur J Public Health. 2001; 9:64–68.
4. Klonoff-Cohen H, Natarajan L, Marrs R, Yee B. Effects of female and male smoking on success rates of IVF and gamete intra-Fallopian transfer. Hum Reprod. 2001; 16:1382–1390.
5. Gruber I, Just A, Birner M, Lösch A. Effect of a woman’s smoking status on oocyte, zygote, and day 3 pre-embryo quality in in vitro fertilization and embryo transfer program. Fertil Steril. 2008; 90:1249–1252.
6. Firns S, Cruzat VF, Keane KN, Joesbury KA, Lee AH, Newsholme P, Yovich JL. The effect of cigarette smoking, alcohol consumption and fruit and vegetable consumption on IVF outcomes: a review and presentation of original data. Reprod Biol Endocrinol. 2015; 13:134.
7. Lintsen AM, Pasker-de Jong PC, de Boer EJ, Burger CW, Jansen CA, Braat DD, van Leeuwen FE. Effects of subfertility cause, smoking and body weight on the success rate of IVF. Hum Reprod. 2005; 20:1867–1875.
8. Kornya L, Bódis J, Verzár Z, Török A, Tinneberg HR. Cigarette smoking and infertility. Hum Reprod. 1998; 13:3576.
9. Kim H, Kim SK, Yu EJ, Lee JR, Jee BC, Suh CS, Kim SH. The prevalence of positive urinary cotinine tests in Korean infertile couples and the effect of smoking on assisted conception outcomes. Clin Exp Reprod Med. 2015; 42:136–142.
10. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3). Cheongwon: Korea Centers for Disease Control and Prevention;2013.
11. Neal MS, Hughes EG, Holloway AC, Foster WG. Sidestream smoking is equally as damaging as mainstream smoking on IVF outcomes. Hum Reprod. 2005; 20:2531–2535.
12. Peppone LJ, Piazza KM, Mahoney MC, Morrow GR, Mustian KM, Palesh OG, Hyland A. Associations between adult and childhood secondhand smoke exposures and fecundity and fetal loss among women who visited a cancer hospital. Tob Control. 2009; 18:115–120.
13. Hull MG, North K, Taylor H, Farrow A, Ford WC; The Avon Longitudinal Study of Pregnancy and Childhood Study Team. Delayed conception and active and passive smoking. Fertil Steril. 2000; 74:725–733.
14. Rhee MK, Lee YH, Jung HY, Choi JH, Kim SH, Kim YK, Lee SK. A standardization study of Beck depression inventory II—Korean version (K-BDI): validity. Korean J Psychopathol. 1995; 4:96–104.
15. Pirkle JL, Flegal KM, Bernert JT, Brody DJ, Etzel RA, Maurer KR. Exposure of the US population to environmental tobacco smoke: the third National Health and Nutrition Examination Survey, 1988 to 1991. JAMA. 1996; 275:1233–1240.
17. Meeker JD, Benedict MD. Infertility, pregnancy loss and adverse birth outcomes in relation to maternal secondhand tobacco smoke exposure. Curr Womens Health Rev. 2013; 9:41–49.
18. Lee SR, Lee CK, Im H, Yang W, Urm SH, Yu SD, Lee JH, Suh CH, Kim KH, Son BC, et al. Secondhand smoke exposure and urine cotinine concentrations by occupation among Korean workers: results from the 2008 Korea national survey for environmental pollutants in the human body. J Occup Environ Hyg. 2014; 11:314–325.
19. Meeker JD, Missmer SA, Cramer DW, Hauser R. Maternal exposure to second-hand tobacco smoke and pregnancy outcome among couples undergoing assisted reproduction. Hum Reprod. 2007; 22:337–345.
20. Wagenknecht LE, Perkins LL, Cutter GR, Sidney S, Burke GL, Manolio TA, Jacobs DR Jr, Liu KA, Friedman GD, Hughes GH, et al. Cigarette smoking behavior is strongly related to educational status: the CARDIA study. Prev Med. 1990; 19:158–169.
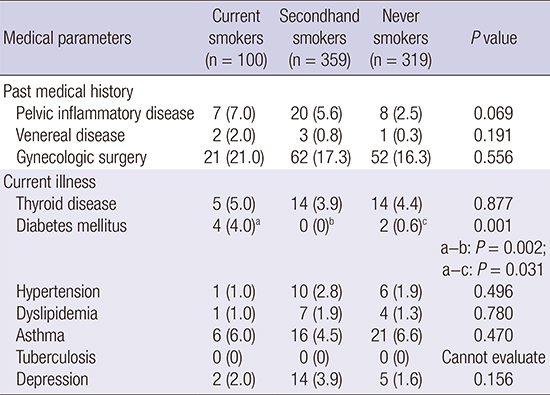
21. InterAct Consortium. Smoking and long-term risk of type 2 diabetes: the EPIC-InterAct study in European populations. Diabetes Care. 2014; 37:3164–3171.
22. Will JC, Galuska DA, Ford ES, Mokdad A, Calle EE. Cigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort study. Int J Epidemiol. 2001; 30:540–546.
23. Cho NH, Chan JC, Jang HC, Lim S, Kim HL, Choi SH. Cigarette smoking is an independent risk factor for type 2 diabetes: a four-year community-based prospective study. Clin Endocrinol (Oxf). 2009; 71:679–685.
24. Jee SH, Foong AW, Hur NW, Samet JM. Smoking and risk for diabetes incidence and mortality in Korean men and women. Diabetes Care. 2010; 33:2567–2572.
25. Biringer E, Howard LM, Kessler U, Stewart R, Mykletun A. Is infertility really associated with higher levels of mental distress in the female population? Results from the North-Trøndelag Health Study and the Medical Birth Registry of Norway. J Psychosom Obstet Gynaecol. 2015; 36:38–45.
26. Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med. 1997; 45:1679–1704.
27. Domar AD, Broome A, Zuttermeister PC, Seibel M, Friedman R. The prevalence and predictability of depression in infertile women. Fertil Steril. 1992; 58:1158–1163.
28. Domar AD, Zuttermeister PC, Friedman R. The psychological impact of infertility: a comparison with patients with other medical conditions. J Psychosom Obstet Gynaecol. 1993; 14:Suppl. 45–52.
29. Demyttenaere K, Bonte L, Gheldof M, Vervaeke M, Meuleman C, Vanderschuerem D, D'Hooghe T. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril. 1998; 69:1026–1033.
30. Pasch LA, Gregorich SE, Katz PK, Millstein SG, Nachtigall RD, Bleil ME, Adler NE. Psychological distress and in vitro fertilization outcome. Fertil Steril. 2012; 98:459–464.
31. Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundström Poromaa I. Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Fertil Steril. 2010; 93:1088–1096.
32. Lawson AK, Klock SC, Pavone ME, Hirshfeld-Cytron J, Smith KN, Kazer RR. Prospective study of depression and anxiety in female fertility preservation and infertility patients. Fertil Steril. 2014; 102:1377–1384.
33. Windham GC, Elkin EP, Swan SH, Waller KO, Fenster L. Cigarette smoking and effects on menstrual function. Obstet Gynecol. 1999; 93:59–65.
34. Belin RM, Astor BC, Powe NR, Ladenson PW. Smoke exposure is associated with a lower prevalence of serum thyroid autoantibodies and thyrotropin concentration elevation and a higher prevalence of mild thyrotropin concentration suppression in the third National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2004; 89:6077–6086.
35. Jorde R, Sundsfjord J. Serum TSH levels in smokers and non-smokers. The 5th Tromsø study. Exp Clin Endocrinol Diabetes. 2006; 114:343–347.
36. Baron JA. Cigarette smoking and Parkinson’s disease. Neurology. 1986; 36:1490–1496.
37. Al-Turki HA. Effect of smoking on reproductive hormones and semen parameters of infertile Saudi Arabians. Urol Ann. 2015; 7:63–66.
38. Baron JA, Bulbrook RD, Wang DY, Kwa HG. Cigarette smoking and prolactin in women. Br Med J (Clin Res Ed). 1986; 293:482–483.
39. Asvold BO, Bjøro T, Nilsen TI, Vatten LJ. Tobacco smoking and thyroid function: a population-based study. Arch Intern Med. 2007; 167:1428–1432.
40. Caserta D, Bordi G, Di Segni N, D'Ambrosio A, Mallozzi M, Moscarini M. The influence of cigarette smoking on a population of infertile men and women. Arch Gynecol Obstet. 2013; 287:813–818.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download