This article has been
cited by other articles in ScienceCentral.
Abstract
The diagnosis of hepatocellular carcinoma (HCC) is based on imaging studies particularly in high-risk patients without histologic confirmation. This study evaluated the prevalence and characteristics of false-positively diagnosed HCC in a liver resection cohort for HCC. A retrospective review was performed of 837 liver resection cases for clinically diagnosed HCC between 2005 and 2010 at our institute. High-risk patients with tumors > 1 cm with one or two image findings consistent with HCC and tumors < 1 cm with two or more image findings consistent with HCC with persistently increased serum alpha-fetoprotein (AFP) levels above the normal range with underlying inhibited hepatitis activity underwent liver resection. The false-positive rate was 2.2% (n = 18). Of the 18 patients, 7 patients (0.8%) were diagnosed with benign conditions (one each of hemangioma, inflammation, cortical adenoma, dysplastic nodule, angiomyolipoma, bile duct adenoma, and non-neoplastic liver parenchyme) and 11 patients (1.3%) were diagnosed with malignancies (cholangiocarcinoma [n = 6], hepatoblastoma [n = 2], and one each of lymphoepithelioma-like carcinoma, ovarian cystadenocarcinoma, and nasopharynx carcinoma metastasis). The clinical characteristics of pathologically diagnosed HCC patients were similar (P > 0.05) compared to non-HCC patients except for higher rate of history of alcoholism (P < 0.05) observed in non-HCC patients. Four of 18 non-HCC patients (22.2%) showed diagnostic discordance on the dynamic imaging study. Despite the recent progression in diagnostic imaging techniques, 2.2% of cases were false-positively diagnosed as HCC in a liver resection patient cohort; and the final diagnosis was benign disease in 0.8% of liver resection patients clinically diagnosed with HCC.
Keywords: Hepatocellular Carcinoma, False-positive Diagnosis, Clinical Diagnosis, Liver Resection
INTRODUCTION
The diagnosis of hepatocellular carcinoma (HCC) is mainly based on clinical information and radiologic imaging studies in high-risk patients; i.e., hepatitis B virus (HBV), hepatitis C virus (HCV), alcoholic liver disease and/or liver cirrhosis with the aid of a reference serum alpha-fetoprotein (AFP) level. Compared to other malignancies, HCC can be clinically diagnosed without histological confirmation (
1).
When HCC is suspected during surveillance in high-risk patients, four-phase dynamic contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) is recommended. During the past few decades, advances in dynamic CT and MRI have significantly improved the clinical diagnostic accuracy of HCC (
234). Such advances in imaging modalities have made clinical diagnosis of HCC possible. According to the European Association for the Study of the Liver-European Organization for Research and Treatment of Cancer (EASL-EORTC) (
5) and the Korean Association for the Study of the Liver (KASL) guideline (
1) of noninvasive diagnostic criteria for HCC, HCC can be diagnosed in the high-risk group with nodules ≥ 1 cm in diameter if one of the 4-phase multi-detector CT scan or dynamic contrast-enhanced MRI shows typical hallmark of HCC. Two or more imaging modalities are required if a suboptimal imaging technique is used. Typical hallmarks of HCC include arterial enhancement with washout in the portal or delayed phase.
As most HCC is clinically diagnosed, a false-positive diagnosis can inevitably prevail after liver resection. Furthermore, the false-positive diagnosis rate in studies performed in the early 2000s was 0.7%–3.1% (
678). However, only a few studies were performed regarding the false-positive rate for a clinical diagnosis of HCC in patients who underwent liver resection. According to recent studies, CT scans have sensitivity of 0.84 (95% confidence interval [CI], 0.59–0.95) and specificity of 0.99 (95% CI, 0.86–0.999) in surveillance settings. In a non-surveillance setting, sensitivity was 0.83 (95% CI, 0.75–0.89; 17 studies) and specificity was 0.91 (95% CI, 0.86–0.96; 11 studies) for CT scans. Study evaluating the diagnostic accuracy of MRI in a surveillance setting are lacking; however, in a non-surveillance setting, sensitivity was 0.86 (95% CI, 0.79–0.91; 14 studies) and specificity was 0.89 (95% CI 0.83–0.93; 12 studies) for MRI (
4).
This study evaluated the prevalence and characteristics of false-positive diagnosis of clinically diagnosed HCC in surgical resection patients based on advances in liver imaging studies, and evaluated possible differential diagnosis from real HCC in liver resection candidates for potential HCC.
MATERIALS AND METHODS
The surgical database of patients who underwent liver resections between January 2005 and December 2010 at Seoul National University Hospital was reviewed retrospectively. This surgical data base was prospectively collected by two data managers.
Diagnostic criteria of HCC at our institute included high-risk patients of HCC with tumors ≥ 1 cm with one or two image findings consistent with HCC. Tumors < 1 cm with two or more image findings consistent with HCC in high-risk patients with persistently increased serum AFP levels above the normal range and underlying inhibited hepatitis activity were eligible for liver resection.
Indication of surgical resection at our institution were as follows; 1) intrahepatic single nodular HCC and well-preserved liver function of Child-Pugh class A without portal hypertension or hyperbilirubinemia, 2) limited resection for HCC patients with liver function Child-Pugh class A or B and with mild portal hypertension or mild hyperbilirubinemia, and 3) less frequently, in patients with three or fewer intrahepatic tumors without macrovascular invasion in cases with well-preserved hepatic function.
Exclusion criteria were insufficient data, preoperative liver biopsy or successful trans-arterial chemoembolization (TACE) before surgery. Among the 876 patients who underwent liver resections, 3 cases (0.3%) were excluded due to insufficient data; and 10 cases (1.1%) were excluded due to preoperative liver biopsy. Of the 863 liver resections, 26 (3.0%) underwent TACE preoperatively and were excluded because the final pathological diagnosis was obscured due to an effective and successful procedure. Finally, 837 patients among 876 patients were included in this study (
Fig. 1) and were evaluated diagnostically based on preoperative clinical risk factors and imaging studies.
Fig. 1
Patient selection in the liver resection cohort.

Quadri-phase (4P) dynamic liver CT scans were performed for 781 liver resections (93.3%) and gadoxetic-acid liver MRI was performed for 607 liver resections (72.5%). The clinical data at the time of diagnosis and surgery were compared between HCC and non-HCC confirmed cases. Relevant clinical factors included age, gender, history of alcoholism, underlying liver disease including viral markers, and serum AFP. Pathological diagnoses were made by two expert hepatopathologists with more than 10 years of experience in liver pathology. Furthermore, diagnostic concordance to the EASL-EORTC and the KASL guidelines were reviewed in non-HCC patients, and imaging studies including CT scans and/or MRI were reviewed individually by a radiologist specializing in abdominal imaging.
CT acquisition
The 4P liver CT evaluation consisted of pre-contrast, arterial, portal and delayed phase. Patients were randomly allocated to one of the CT scanners with multi-detector (≥ 4) at our institution (MX 8000, Philips Healthcare, Bothell, WA, USA; Lightspeed Ultra, GE Healthcare, Waukesha, WI, USA; Sensation 16, Siemens Healthcare, Elrangen, Germany). The acquisition protocol was uniform regardless of the type of CT scanners. After scanning the pre-contrast phase, contrast media (1.5 mL/kg of Ultravist 370, Bayer-Schering Pharmaceuticals, Berlin, Germany) was injected at a rate of 2–4 mL/sec using a power injector (Multilevel CT, Medrad, Indianola, PA, USA) followed by saline flush. The arterial phase was obtained using the bolus tracking method, and the portal and delayed phases were obtained 70 and 180 seconds after contrast media injection, respectively. All scans were performed using standard kVp and automatic tube-current modulation for each vendor, when available.
Magnetic resonance (MR) acquisition
Patients underwent liver MRI with either 1.5T (Signa HDx, GE Healthcare) or 3T scanner (Magnetom Verio, Siemens Healthcare). Our routine MR sequence include heavily T2-weighted images (T2WI), pre-contrast T1-weighted images (T1WI), dual-echo image, dynamic sequence (arterial, portal, 3 minutes delay) and hepatobiliary phase (20 minutes delayed phase). Diffusion weighted image (DWI) was obtained using two b-values depending on the scanner capability (0 and 500 sec/mm2 at 1.5T or 0 and 800 sec/mm2 at 3T). All images were acquired in the axial plane. After the intravenous injection of a standard dose of gadoxetic acid (0.025 mMol/kg, Gd-EOB-DTPA, Primovist or Eovist, Bayer-Schering Pharmaceuticals) at a rate of 1.5 mL/sec followed by a saline chaser with power injector (Spectris Solaris® EP, MEDRAD, Bayer-Schering Pharmaceuticals), the arterial phase was obtained under guidance of MR fluoroscopy, and the portal phase was obtained 60–70 seconds after contrast media injection. In addition, 3 and 20 minutes delayed phases were obtained in the same manner.
Ethics statement
This study protocol was reviewed and approved by the institutional review board of the Seoul National University Hospital (H1601-094-735). The board waived informed consent by individual patients.
RESULTS
Clinical characteristics of the non-HCC cases at the time of liver resection
Of the 837 patients who underwent liver resection for clinically diagnosed HCC, 18 (2.2%) were histologically diagnosed as non-HCC postoperatively. Of the 18 patients, 7 (0.8%) were diagnosed with benign conditions, and 11 (1.3%) were diagnosed with malignancies.
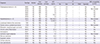
The clinical characteristics of the patients with HCC and with non-HCC conditions are described in
Table 1. The median age at diagnosis for patients with non-HCC was 52.4 (range, 17–71) years, and 15 patients (83.3%) were male. Underlying liver disease was noted in 12 patients (66.7%); hepatitis B infection in 10 (55.6%), hepatitis C infection in 1 (5.6%), and alcoholism in 1 (5.6%). Regardless of underlying liver disease, 14 patients (77.8%) had liver cirrhosis. The median aspartate aminotransferase (AST) level in patients with non-HCC, was 36.6 (range, 20–78) IU/L, alanine transaminase (ALT) was 38.4 (range, 11–130) IU/L, total bilirubin was 1.0 (range, 0.4–2.2) mg/dL, alkaline phosphatase (ALP) was 71.9 (range, 49–114) IU/L, and albumin was 4.1 (range, 3.5–4.8) g/dL. The median international normalized ratio (INR) of prothrombin time was 1.04 (range, 0.89–1.24) and platelet count was 195.7 (range, 49–592 × 10
3/µL. Two patients (11.1%) had platelet counts < 100 × 10
3/µL. The median serum AFP level was 11,621.3 (range, 1.8–195,700) ng/mL. Six patients (33.4%) showed increased serum AFP levels > 20 ng/mL; among them, 3 (16.7%) had levels > 200 ng/mL. The clinical characteristics and laboratory results were not different (
P > 0.05) compared to patients with pathologically diagnosed HCC except for higher rate of history of alcoholism (
P < 0.05) observed in non-HCC patients.
Table 1
Clinical characteristics, laboratory data and CT findings of HCC and non-HCC

|
Clinical characteristics |
HCC (n = 819) |
Non-HCC (n = 18) |
P value |
|
Age at diagnosis, yr |
56.00 (16–82) |
52.40 (17–71) |
0.144 |
|
Gender |
|
|
|
|
Male |
664 (81.1) |
15 (83.3) |
0.809 |
|
Female |
155 (18.9) |
3 (16.7) |
|
|
History of alcoholism |
74 (9.0) |
1 (5.6) |
< 0.050 |
|
Liver disease |
|
|
|
|
Past/present HBV infection |
655 (80.0) |
10 (55.6) |
0.034 |
|
HCV infection |
67 (8.2) |
1 (5.6) |
0.687 |
|
Cirrhosis |
583 (75.7) |
14 (77.8) |
0.840 |
|
Laboratory data and tumor markers |
|
|
|
|
AST, IU/L |
48.40 (12–702) |
36.60 (20–78) |
0.311 |
|
ALT, IU/L |
46.20 (4–612) |
38.40 (11–130) |
0.454 |
|
Total bilirubin, mg/dL |
1.30 (0.1–19.0) |
1.00 (0.4–2.2) |
0.589 |
|
ALP, IU/L |
96.30 (4–856) |
71.90 (49–114) |
0.113 |
|
Prothrombin time, INR |
1.10 (0.18–2.18) |
1.04 (0.89–1.24) |
0.470 |
|
Albumin, g/dL |
3.90 (1.6–6.8) |
4.10 (3.5–4.8) |
0.107 |
|
Platelet count, 103/µL |
165.10 (1.2–970) |
195.70 (49–592) |
0.159 |
|
< 100 × 103
|
145 (17.7) |
2 (11.1) |
0.722 |
|
AFP, ng/mL |
7,168.30 (1–388,000) |
11,621.30 (1.8–195,700) |
0.588 |
|
> 20 and ≤ 200 |
164 (20.0) |
3 (16.7) |
0.599 |
|
> 200 |
254 (31.0) |
3 (16.7) |
0.135 |
|
CT findings |
|
|
|
|
Number |
|
|
0.684 |
|
1 |
710 (92.3) |
18 (100) |
|
2 |
41 (5.3) |
0 (0) |
|
≥ 3 |
18 (2.3) |
0 (0) |
|
Size, cm |
4.90 (0.8–18.5) |
4.40 (1.2–19) |
0.572 |
|
< 2 |
84 (10.8) |
3 (16.7) |
|
2–5 |
450 (57.6) |
10 (55.6) |
|
> 5 |
247 (31.6) |
5 (27.7) |
All 18 non-HCC patients had a single lesion on liver CT/MRI. The number of tumors in non-HCC patients was not different from that in patients with HCC (P = 0.653). No tumor was < 1 cm in non-HCC cases. Three of patients (16.7%) had tumor < 2 cm, 10 (55.6%) had tumor sizes of 2–5 cm, and 5 had (27.7%) tumors ≥ 5 cm. The size distribution was not different from patients with HCC (P = 0.290).
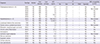
Imaging hallmarks of the non-HCC cases at the time of liver resection
CT scans were taken in all 18 non-HCC cases, whereas MRI was done in 14 cases (51.9%). MRI was not used as the primary diagnostic tool. Of the 18 patients, 8 (44.4%) had typical hallmarks of arterial enhancement and portal/delayed washout on 4P CT scans; among them, 7 cases had MRI findings compatible to HCC. The other 10 (55.6%) revealed CT scans inconsistent with HCC; 5 (27.8%) had an arterial enhancement pattern without portal/delayed washout, and 5 (27.8%) patients had portal/delayed washout patterns without arterial enhancement on 4P dynamic CT scans. Among these 10 patients, eight underwent dynamic MRI and the other three did not. Thus, 1 (0.1%) with no underlying risk factors with only one typical HCC imaging on CT scans and 3 (0.3%) with discordant CT scans without MRI showed diagnostic discordance with the HCC clinical diagnostic criteria based on the EASL-EORCT and the KASL guidelines (
Table 2).
Table 2
Characteristics of non-HCC patients
|
Diagnosis |
Sex/Age |
Alcohol |
Viral infection |
Liver cirrhosis |
AFP, ng/mL |
CT |
MRI compatibility to HCC |
|
No. |
Size |
AE |
PDW |
Typicality |
|
Cholangiocarcinoma (n = 6) |
M/62 |
No |
HBV |
Yes |
12.7 |
1 |
3.0 |
+ |
+ |
Yes |
Yes |
|
M/69 |
No |
HBV |
No |
5.0 |
1 |
3.4 |
− |
+ |
No |
Not checked |
|
M/46 |
No |
HBV |
Yes |
3.0 |
1 |
2.7 |
+ |
− |
No |
Yes |
|
M/60 |
No |
HBV |
Yes |
2.6 |
1 |
1.8 |
+ |
+ |
Yes |
Yes |
|
M/62 |
No |
No |
Yes |
740.0 |
1 |
5.7 |
+ |
− |
No |
Yes |
|
M/59 |
No |
No |
Yes |
5.0 |
1 |
5.7 |
+ |
+ |
Yes |
Yes |
|
Hepatoblastoma (n = 2) |
M/53 |
No |
HBV |
Yes |
195,700.0 |
1 |
9.5 |
− |
+ |
No |
Not checked |
|
F/17 |
No |
HBV |
No |
12,500.0 |
1 |
19.0 |
+ |
− |
No |
Yes |
|
Lymphoepi-thelioma like carcinoma |
F/60 |
No |
HBV |
Yes |
2.9 |
1 |
2.8 |
+ |
− |
No |
Yes |
|
Ovarian serous cystadenocarcinoma |
F/49 |
No |
No |
No |
5.2 |
1 |
2.8 |
+ |
+ |
Yes |
Not checked |
|
Metastatic nasopharyngeal carcinoma |
M/53 |
No |
HBV |
Yes |
2.1 |
1 |
2.6 |
+ |
+ |
Yes |
Yes |
|
Chronic active inflammation |
M/43 |
No |
HBV |
Yes |
81.0 |
1 |
2.3 |
− |
+ |
No |
Yes |
|
Hemangioma |
M/47 |
No |
HBV |
Yes |
77.8 |
1 |
5.8 |
+ |
− |
No |
Yes |
|
Epitheliod angiomyolipoma |
M/36 |
No |
HBV |
Yes |
5.0 |
1 |
3.8 |
− |
+ |
No |
Not checked |
|
Bile duct adenoma |
M/48 |
No |
HBV |
Yes |
24.8 |
1 |
1.2 |
+ |
+ |
Yes |
Yes |
|
Dysplastic nodule |
M/63 |
No |
HCV |
Yes |
8.3 |
1 |
1.8 |
+ |
+ |
Yes |
Yes |
|
Cortical adenoma |
M/45 |
Yes |
No |
No |
1.8 |
1 |
2.5 |
− |
+ |
No |
Yes |
|
Liver parenchyma |
M/71 |
No |
No |
Yes |
6.7 |
1 |
2.8 |
+ |
+ |
Yes |
Yes |
Pathological diagnosis of the non-HCC cases after liver resection
Of the 18 patients, 7 (38.9%) were diagnosed with benign conditions (one each of cavernous hemangioma, chronic active inflammation, adrenal cortical adenoma, dysplastic nodule, epithelioid angiomyolipoma, bile duct adenoma, and non-neoplastic liver parenchyme) and 11 (61.1%) were diagnosed as malignancies (cholangiocarcinoma [n = 6], hepatoblastoma [n = 2], and one each of lymphoepithelioma-like carcinoma, ovarian cystadenocarcinoma, and nasopharynx carcinoma metastasis) (
Fig. 2).
Fig. 2
Final diagnosis after liver resection for clinically diagnosed HCC.

DISCUSSION
Since the introduction of dynamic 4P CT and MRI, the diagnosis of HCC has changed dramatically. Advances in these imaging modalities have greatly enhanced the diagnostic accuracy of liver tumors. The diagnostic accuracy after liver resection in clinically diagnosed HCC was 97.8% in this study. However, the false-positive rate has not been decreased despite the advances in the imaging modalities in the last 15 years, indicating the diagnostic difficulty of small lesions ≤ 2 cm in cirrhotic livers. According to previous studies, the false-positive rate of clinical diagnosis in cirrhotic livers is ≥ 30%, particularly for tumors ≤ 3 cm, whereas the false-positive diagnostic rate of chronic liver disease without cirrhosis is 10% in resected specimens (
4910). In this study, 594 (72.5%) among 819 cases of clinically diagnosed HCC had underlying cirrhosis and 14 out of 18 cases (77.8%) of non-HCC had underlying cirrhosis. A total of 87 cases had nodules ≤ 2 cm and among the 837 cases, three were diagnosed as non-HCC. The false-positive rate in nodules ≤ 2 cm was 3.4%.
Some patients may undergo other managements with radiofrequency ablation (RFA) and TACE before surgery. The final pathology may be a ‘totally necrotic nodule’ in liver resections after effective and successful RFA or TACE. Therefore, in such cases, the diagnosis can be ambiguous and the actual false-positive diagnostic rate obscured. Four of 27 patients (14.8%) received TACE before liver resection in our study. TACE was incomplete, and these 4 patients were diagnosed with cholangiocarcinoma in 2, combined HCC and cholangiocarcinoma, and angiomyolipoma. Therefore, more patients may have been clinically diagnosed with HCC and underwent other treatment modalities before surgery when the post-operative diagnosis was indefinite due to total necrosis of the tumor. Also, patients with benign disease may have undergone unnecessary TACE.
Seven of 837 patients (0.8%) who underwent liver resections were diagnosed with benign diseases. However, the patients diagnosed with dysplastic nodule, angiomyolipoma, and bile duct adenoma should be considered as a relative indication for surgery. Although these tumors can be conservatively managed, progression to malignancy or to a larger tumor is well known. However, judging may be very difficult to exclude or defer from surgery. The incidence of benign disease in these cases is ≤ 1%.
On the other hand, the non-HCC but malignant diseases included very rare diseases, i.e., lymphoepithelioma-like carcinoma, ovarian carcinoma, metastatic nasopharyngeal carcinoma, as well as cholangiocarcinoma and hepatoblastoma which are well known differential diagnosis with HCC. This disease category is also very difficult to diagnosis before surgery without a biopsy. Fortunately, these tumors were single, and the surgical resection had curative intent.
Therefore, the major finding of this study is a false-positive rate ≤ 3%, although the false-positive rate has been improved in patients with cirrhosis and with small nodules. If we follow the exact clinical guidelines, after excluding the diagnostic discordant cases (n = 4), the false positive rate would decrease to ≤ 2% (n = 14, 1.7%). Other tumors showed arterial enhancement and portal/delayed washout either at CT or MRI, which fulfills the non-invasive diagnostic criteria of HCC in high-risk patient group. The finding is the suggestion of a possible differential diagnosis including benign disease even using very qualified diagnostic tools. This is informative to clinicians getting informed consent from patients and their family with surgery planned for clinically diagnosed HCC without a biopsy according to the HCC treatment guidelines. However, there are some limitations to this study. The study was conducted in a retrospective nature and the number of non-HCC was small to compare with HCC.
In conclusion, a 2.2% false-positive diagnosis of HCC was detected in the liver resection patient cohort and the final diagnosis was benign disease in 0.8% of all patients diagnosed as HCC.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download