1. Robertson PA, Sniderman SH, Laros RK Jr, Cowan R, Heilbron D, Goldenberg RL, Iams JD, Creasy RK. Neonatal morbidity according to gestational age and birth weight from five tertiary care centers in the United States, 1983 through 1986. Am J Obstet Gynecol. 1992; 166:1629–1641.
2. Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006; 118:1566–1573.
3. Norman JE, Morris C, Chalmers J. The effect of changing patterns of obstetric care in Scotland (1980-2004) on rates of preterm birth and its neonatal consequences: perinatal database study. PLoS Med. 2009; 6:e1000153.
4. Romero R, Espinoza J, Kusanovic JP, Gotsch F, Hassan S, Erez O, Chaiworapongsa T, Mazor M. The preterm parturition syndrome. BJOG. 2006; 113:Suppl 3. 17–42.
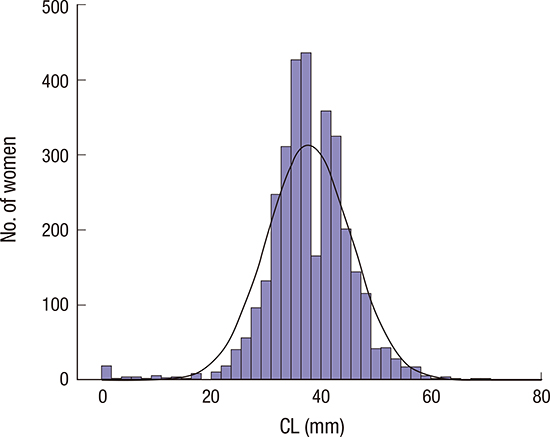
5. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, Thom E, McNellis D, Copper RL, Johnson F, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996; 334:567–572.
6. Parry S, Simhan H, Elovitz M, Iams J. Universal maternal cervical length screening during the second trimester: pros and cons of a strategy to identify women at risk of spontaneous preterm delivery. Am J Obstet Gynecol. 2012; 207:101–106.
7. Kuusela P, Jacobsson B, Söderlund M, Bejlum C, Almström E, Ladfors L, Hagberg H, Wennerholm UB. Transvaginal sonographic evaluation of cervical length in the second trimester of asymptomatic singleton pregnancies, and the risk of preterm delivery. Acta Obstet Gynecol Scand. 2015; 94:598–607.
8. van der Ven AJ, van Os MA, Kleinrouweler CE, de Groot CJ, Haak MC, Mol BW, Pajkrt E, Kazemier BM. Is cervical length associated with maternal characteristics? Eur J Obstet Gynecol Reprod Biol. 2015; 188:12–16.
9. Sakai M, Shiozaki A, Tabata M, Sasaki Y, Yoneda S, Arai T, Kato K, Yamakawa Y, Saito S. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006; 194:14–19.
10. Facco FL, Simhan HN. Short ultrasonographic cervical length in women with low-risk obstetric history. Obstet Gynecol. 2013; 122:858–862.
11. Miller ES, Grobman WA. The association between cervical excisional procedures, midtrimester cervical length, and preterm birth. Am J Obstet Gynecol. 2014; 211:242.e1–242.e4.
12. Shachar BZ, Mayo JA, Lee HC, Carmichael SL, Stevenson DK, Shaw GM, Gould JB. Effects of race/ethnicity and BMI on the association between height and risk for spontaneous preterm birth. Am J Obstet Gynecol. 2015; 213:700.e1–700.e9.
13. Beta J, Akolekar R, Ventura W, Syngelaki A, Nicolaides KH. Prediction of spontaneous preterm delivery from maternal factors, obstetric history and placental perfusion and function at 11-13 weeks. Prenat Diagn. 2011; 31:75–83.
14. Torloni MR, Betrán AP, Daher S, Widmer M, Dolan SM, Menon R, Bergel E, Allen T, Merialdi M. Maternal BMI and preterm birth: a systematic review of the literature with meta-analysis. J Matern Fetal Neonatal Med. 2009; 22:957–970.
15. Sharashova EE, Anda EE, Grjibovski AM. Early pregnancy body mass index and spontaneous preterm birth in Northwest Russia: a registry-based study. BMC Pregnancy Childbirth. 2014; 14:303.
16. Albayrak M, Ozdemir I, Koc O, Coskun E. Can maternal height predict shorter cervical length in asymptomatic low-risk pregnant women? Eur J Obstet Gynecol Reprod Biol. 2011; 157:161–165.
17. Poon LC, Savvas M, Zamblera D, Skyfta E, Nicolaides KH. Large loop excision of transformation zone and cervical length in the prediction of spontaneous preterm delivery. BJOG. 2012; 119:692–698.
18. Suh YH, Park KH, Hong JS, Noh JH. Prediction of prolonged pregnancy in nulliparous women by transvaginal ultrasonographic measurement of cervical length at 20-24 weeks and 37 weeks. J Korean Med Sci. 2007; 22:89–93.
19. Jin G. LanLan Z, Li C, Dan Z. Pregnancy outcome following loop electrosurgical excision procedure (LEEP) a systematic review and meta-analysis. Arch Gynecol Obstet. 2014; 289:85–99.
20. Bruinsma F, Lumley J, Tan J, Quinn M. Precancerous changes in the cervix and risk of subsequent preterm birth. BJOG. 2007; 114:70–80.
21. Andía D, Mozo de Rosales F, Villasante A, Rivero B, Díez J, Pérez C. Pregnancy outcome in patients treated with cervical conization for cervical intraepithelial neoplasia. Int J Gynaecol Obstet. 2011; 112:225–228.
22. Heath VC, Southall TR, Souka AP, Novakov A, Nicolaides KH. Cervical length at 23 weeks of gestation: relation to demographic characteristics and previous obstetric history. Ultrasound Obstet Gynecol. 1998; 12:304–311.
23. Miller ES, Tita AT, Grobman WA. Second-trimester cervical length screening among asymptomatic women: an evaluation of risk-based strategies. Obstet Gynecol. 2015; 126:61–66.
24. Orzechowski KM, Boelig R, Nicholas SS, Baxter J, Berghella V. Is universal cervical length screening indicated in women with prior term birth? Am J Obstet Gynecol. 2015; 212:234.e1–234.e5.
25. Miller ES, Sakowicz A, Grobman WA. The association between cervical dysplasia, a short cervix, and preterm birth. Am J Obstet Gynecol. 2015; 213:543.e1–543.e4.
26. Owen J, Hankins G, Iams JD, Berghella V, Sheffield JS, Perez-Delboy A, Egerman RS, Wing DA, Tomlinson M, Silver R, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009; 201:375.e1–375.e8.
27. Souka AP, Papastefanou I, Michalitsi V, Papadopoulos GK, Kassanos D. A predictive model of short cervix at 20-24 weeks using first-trimester cervical length measurement and maternal history. Prenat Diagn. 2011; 31:202–206.
28. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007; 357:462–469.
29. Moroz LA, Simhan HN. Rate of sonographic cervical shortening and the risk of spontaneous preterm birth. Am J Obstet Gynecol. 2012; 206:234.e1–234.e5.
30. Temming LA, Durst JK, Tuuli MG, Stout MJ, Dicke JM, Macones GA, Cahill AG. Universal cervical length screening: implementation and outcomes. Am J Obstet Gynecol. 2016; 214:523.e1–523.e8.
31. Committee on Practice Bulletins—Obstetrics, The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012; 120:964–973.
32. Iams JD. Clinical practice. Prevention of preterm parturition. N Engl J Med. 2014; 370:254–261.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download