This article has been
cited by other articles in ScienceCentral.
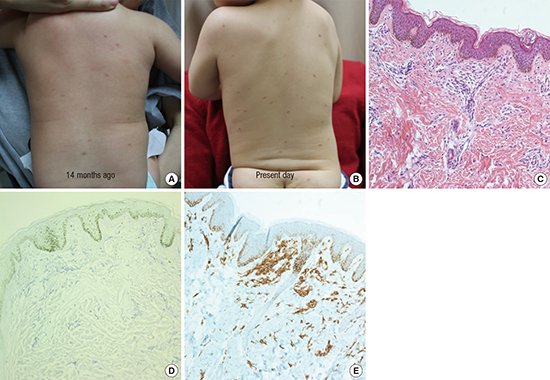
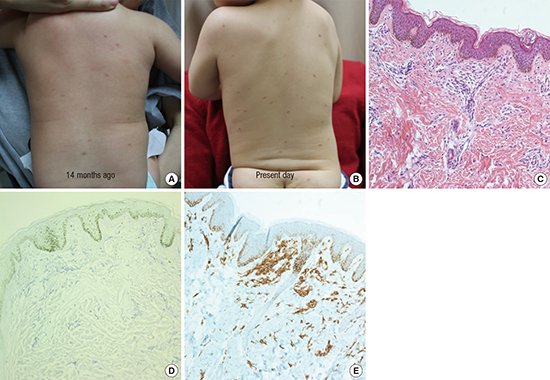
In March 2016, a 22-month-old boy presented with multiple lentigine-like macules on the trunk and thighs that had occurred since 2 months after birth. These lesions initially developed on the back, showing centrifugal spread and gradual size increment with darker color change. He had history of hospitalization for recurrent enteritis and acute bronchiolitis, and also had recurrent urticaria. Clinical examination revealed multiple dark red-brownish macules that appeared upon scratching and were positive for Darier sign on the trunk and both extremities (
Fig. 1A and B). On laboratory examination, the patient had mild anemia with hemoglobin level of 11 g/dL. His liver function tests (LFTs) were within the normal range and he was negative for the multiple allergen simultaneous test (MAST) of foods. Histopathologic examination of skin biopsy on the back showed rich infiltration of mast cells, which are characterized by the presence of metachromatic granules in the cytoplasm. The granules were not visible on hematoxylin and eosin (H & E) staining (
Fig. 1C), but were confirmed after staining with toluidine blue (
Fig. 1D), and c-kit (CD-117) (
Fig. 1E). The serum tryptase was within the normal range (2.3 µg/L). Therefore, the patient was diagnosed with urticaria pigmentosa (UP) (maculopapular cutaneous mastocytosis [CM]). We advised that the patient should avoid mast cell degranulators and environmental triggers. We also recommended annual checks of serum tryptase levels as well as complete blood count and LFTs.
Mastocytosis is characterized by increased numbers of mast cells in the skin, the bone marrow, and/or in other tissues. Most children have CM, which manifests as UP or, less commonly, as mastocytomas or diffuse CM (
1). Ninety percent of cases appear during the second year of life, and mostly improve or resolve spontaneously by adolescence (
23). The pathogenesis of mastocytosis is caused by amassment of mast cells and release of mast cell-mediators in tissues (
4). Mediators include histamine, leukotrienes, prostaglandins, platelet-activating factor, cytokines, and proteases such as tryptase (
1). Hyperpigmentation may be induced through histamine from mast cells (
5). Pruritus associated with UP can be aggravated by a sense of heat, hot shower, friction, alcohol, and emotional stress. It can also be induced by drugs such as anticholinergic preparations, aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), narcotics, and polymyxin B sulfate (
1). Mechanical rubbing and scratching of the lesions causes erythema and edema, and might even result in an anaphylactic reaction, which appears as Darier's sign (
6).
Mastocytosis patients should be cautioned to avoid potential mast cell degranulating agents, which are mentioned above. Therapy is unnecessary in children with UP lesions. Chronic administration of H1 antihistamines, including cetirizine, fexofenadine, and hydroxyzine, is often useful in relieving pruritus (
7).