1. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 365:1687–1717.
2. Olsen AH, Njor SH, Vejborg I, Schwartz W, Dalgaard P, Jensen MB, Tange UB, Blichert-Toft M, Rank F, Mouridsen H, et al. Breast cancer mortality in Copenhagen after introduction of mammography screening: cohort study. BMJ. 2005; 330:220.
3. Stomper PC, D'Souza DJ, DiNitto PA, Arredondo MA. Analysis of parenchymal density on mammograms in 1353 women 25–79 years old. AJR Am J Roentgenol. 1996; 167:1261–1265.
4. Lee A, Chang J, Lim W, Kim BS, Lee JE, Cha ES, Moon BI. Effectiveness of breast-specific gamma imaging (BSGI) for breast cancer in Korea: a comparative study. Breast J. 2012; 18:453–458.
5. Sun Y, Wei W, Yang HW, Liu JL. Clinical usefulness of breast-specific gamma imaging as an adjunct modality to mammography for diagnosis of breast cancer: a systemic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2013; 40:450–463.
6. Brem RF, Floerke AC, Rapelyea JA, Teal C, Kelly T, Mathur V. Breast-specific gamma imaging as an adjunct imaging modality for the diagnosis of breast cancer. Radiology. 2008; 247:651–657.
7. Brem RF, Ruda RC, Yang JL, Coffey CM, Rapelyea JA. Breast-specific γ-imaging for the detection of mammographically occult breast cancer in women at increased risk. J Nucl Med. 2016; 57:678–684.
8. Cho MJ, Yang JH, Yu YB, Park KS, Chung HW, So Y, Choi N, Kim MY. Validity of breast-specific gamma imaging for Breast Imaging Reporting and Data System 4 lesions on mammography and/or ultrasound. Ann Surg Treat Res. 2016; 90:194–200.
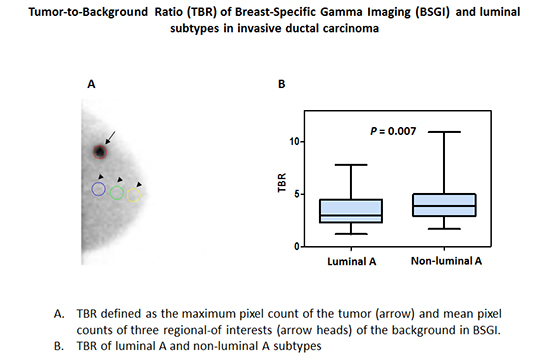
9. Meissnitzer T, Meissnitzer MW, Seymer A, Hergan K, Neureiter D. Relative uptake factor of invasive ductal breast cancer in breast-specific gamma imaging as a surrogate parameter for sub-typing. Anticancer Res. 2015; 35:5671–5677.
10. Tadwalkar RV, Rapelyea JA, Torrente J, Rechtman LR, Teal CB, McSwain AP, Donnelly C, Kidwell AB, Coffey CM, Brem RF. Breast-specific gamma imaging as an adjunct modality for the diagnosis of invasive breast cancer with correlation to tumour size and grade. Br J Radiol. 2012; 85:e212–e216.
11. Yoon HJ, Kim Y, Chang KT, Kim BS. Prognostic value of semi-quantitative tumor uptake on Tc-99m sestamibi breast-specific gamma imaging in invasive ductal breast cancer. Ann Nucl Med. 2015; 29:553–560.
12. Cwikla JB, Buscombe JR, Kolasinska AD, Parbhoo SP, Thakrar DS, Hilson AJ. Correlation between uptake of Tc-99m sestaMIBI and prognostic factors of breast cancer. Anticancer Res. 1999; 19:2299–2304.
13. Tan H, Zhang H, Yang W, Fu Y, Gu Y, Du M, Cheng D, Shi H. Breast-specific gamma imaging with Tc-99m-sestamibi in the diagnosis of breast cancer and its semiquantitative index correlation with tumor biologic markers, subtypes, and clinicopathologic characteristics. Nucl Med Commun. 2016; 37:792–799.
14. Goldsmith SJ, Parsons W, Guiberteau MJ, Stern LH, Lanzkowsky L, Weigert J, Heston TF, Jones E, Buscombe J, Stabin MG, et al. SNM practice guideline for breast scintigraphy with breast-specific gamma-cameras 1.0. J Nucl Med Technol. 2010; 38:219–224.
15. Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010; 28:2784–2795.
16. Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, Thürlimann B, Senn HJ. Panel Members. Tailoring therapies--improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015; 26:1533–1546.
17. Sanli Y, Kuyumcu S, Ozkan ZG, Işik G, Karanlik H, Guzelbey B, Turkmen C, Ozel S, Yavuz E, Mudun A. Increased FDG uptake in breast cancer is associated with prognostic factors. Ann Nucl Med. 2012; 26:345–350.
18. Kim J, Yoo SW, Kang SR, Cho SG, Oh JR, Chong A, Min JJ, Bom HS, Yoon JH, Song HC. Prognostic significance of metabolic tumor volume measured by (18)F-FDG PET/CT in operable primary breast cancer. Nucl Med Mol Imaging. 2012; 46:278–285.
19. Papantoniou V, Christodoulidou J, Papadaki E, Valotassiou V, Souvatzoglou M, Louvrou A, Feida H, Sotiropoulou M, Pampouras G, Michalas S, et al. Uptake and washout of 99mTcV-dimercaptosuccinic acid and 99mTc-sestamibi in the assessment of histological type and grade in breast cancer. Nucl Med Commun. 2002; 23:461–467.
20. Papantoniou VJ, Souvatzoglou MA, Valotassiou VJ, Louvrou AN, Ambela C, Koutsikos J, Lazaris D, Christodoulidou JK, Sotiropoulou MG, Melissinou MJ, et al. Relationship of cell proliferation (Ki-67) to 99mTc-(V)DMSA uptake in breast cancer. Breast Cancer Res. 2004; 6:R56–R62.
21. Kim BS. Usefulness of breast-specific gamma imaging as an adjunct modality in breast cancer patients with dense breast: a comparative study with MRI. Ann Nucl Med. 2012; 26:131–137.
22. Dunnwald LK, Rossing MA, Li CI. Hormone receptor status, tumor characteristics, and prognosis: a prospective cohort of breast cancer patients. Breast Cancer Res. 2007; 9:R6.
23. Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E, Zackrisson S, Cardoso F; ESMO Guidelines Committee. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015; 26:Suppl 5. v8–v30.
24. Kim BS, Moon BI, Cha ES. A comparative study of breast-specific gamma imaging with the conventional imaging modality in breast cancer patients with dense breasts. Ann Nucl Med. 2012; 26:823–829.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download