1. van Doorn PA, Ruts L, Jacobs BC. Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. Lancet Neurol. 2008; 7:939–950.
2. Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, Keenlyside RA, Ziegler DW, Retailliau HF, Eddins DL, Bryan JA. Guillain-Barré syndrome following vaccination in the National Influenza Immunization Program, United States, 1976–1977. Am J Epidemiol. 1979; 110:105–123.
3. Martín Arias LH, Sanz R, Sáinz M, Treceño C, Carvajal A. Guillain-Barré syndrome and influenza vaccines: a meta-analysis. Vaccine. 2015; 33:3773–3778.
4. Kim HJ, Kim JY, Oh J, Park KD. A case of Guillain-Barré syndrome following influenza vaccination. J Korean Assoc EMG Electrodiagn Med. 2009; 11:35–38.
5. Dieleman J, Romio S, Johansen K, Weibel D, Bonhoeffer J, Sturkenboom M; VAESCO-GBS Case-Control Study Group. Guillain-Barré syndrome and adjuvanted pandemic influenza A (H1N1) 2009 vaccine: multinational case-control study in Europe. BMJ. 2011; 343:d3908.
6. Sejvar JJ, Kohl KS, Gidudu J, Amato A, Bakshi N, Baxter R, Burwen DR, Cornblath DR, Cleerbout J, Edwards KM, et al. Guillain-Barré syndrome and Fisher syndrome: case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 2011; 29:599–612.
7. Vellozzi C, Burwen DR, Dobardzic A, Ball R, Walton K, Haber P. Safety of trivalent inactivated influenza vaccines in adults: background for pandemic influenza vaccine safety monitoring. Vaccine. 2009; 27:2114–2120.
8. Geier MR, Geier DA, Zahalsky AC. Influenza vaccination and Guillain-Barré syndrome. Clin Immunol. 2003; 107:116–121.
9. Fokke C, van den Berg B, Drenthen J, Walgaard C, van Doorn PA, Jacobs BC. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain. 2014; 137:33–43.
10. Choe YJ, Cho H, Bae GR, Lee JK. Guillain-Barré syndrome following receipt of influenza A (H1N1) 2009 monovalent vaccine in Korea with an emphasis on Brighton Collaboration case definition. Vaccine. 2011; 29:2066–2070.
11. Choe YJ, Cho H, Kim SN, Bae GR, Lee JK. Serious adverse events following receipt of trivalent inactivated influenza vaccine in Korea, 2003–2010. Vaccine. 2011; 29:7727–7732.
12. Kim JK, Bae JS, Kim DS, Kusunoki S, Kim JE, Kim JS, Park YE, Park KJ, Song HS, Kim SY, et al. Prevalence of anti-ganglioside antibodies and their clinical correlates with Guillain-Barré syndrome in Korea: a nationwide multicenter study. J Clin Neurol. 2014; 10:94–100.
13. Salmon DA, Proschan M, Forshee R, Gargiullo P, Bleser W, Burwen DR, Cunningham F, Garman P, Greene SK, Lee GM, et al. Association between Guillain-Barré syndrome and influenza A (H1N1) 2009 monovalent inactivated vaccines in the USA: a meta-analysis. Lancet. 2013; 381:1461–1468.
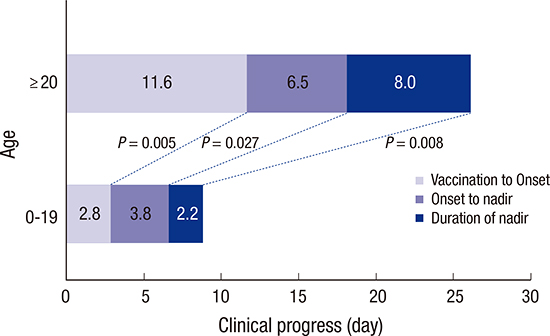
14. Wu X, Shen D, Li T, Mao M, Zhao J, Liu K, Zhang HL. Distinct clinical characteristics of pediatric Guillain-Barré syndrome: a comparative study between children and adults in Northeast China. PLoS One. 2016; 11:e0151611.
15. Van Koningsveld R, Van Doorn PA, Schmitz PI, Ang CW, Van der Meché FG. Mild forms of Guillain-Barré syndrome in an epidemiologic survey in the Netherlands. Neurology. 2000; 54:620–625.
16. Korinthenberg R, Schessl J, Kirschner J. Clinical presentation and course of childhood Guillain-Barré syndrome: a prospective multicentre study. Neuropediatrics. 2007; 38:10–17.
17. Forsberg A, Press R, Einarsson U, de Pedro-Cuesta J, Widén Holmqvist L; Swedish Epidemiological Study Group. Impairment in Guillain-Barré syndrome during the first 2 years after onset: a prospective study. J Neurol Sci. 2004; 227:131–138.
18. Schattner A. Consequence or coincidence? The occurrence, pathogenesis and significance of autoimmune manifestations after viral vaccines. Vaccine. 2005; 23:3876–3886.
19. Souayah N, Nasar A, Suri MF, Qureshi AI. Guillain-Barré syndrome after vaccination in United States a report from the CDC/FDA Vaccine Adverse Event Reporting System. Vaccine. 2007; 25:5253–5255.
20. Patja A, Paunio M, Kinnunen E, Junttila O, Hovi T, Peltola H. Risk of Guillain-Barré syndrome after measles-mumps-rubella vaccination. J Pediatr. 2001; 138:250–254.
21. da Silveira CM, Salisbury DM, de Quadros CA. Measles vaccination and Guillain-Barré syndrome. Lancet. 1997; 349:14–16.
22. Nakayama T, Onoda K. Vaccine adverse events reported in post-marketing study of the Kitasato Institute from 1994 to 2004. Vaccine. 2007; 25:570–576.
23. Kim C, Rhie S, Suh M, Kang DR, Choi YJ, Bae GR, Choi YC, Jun BY, Lee JS. Pandemic influenza A vaccination and incidence of Guillain-Barré syndrome in Korea. Vaccine. 2015; 33:1815–1823.
24. Luigetti M, Servidei S, Modoni A, Rossini PM, Sabatelli M, Lo Monaco M. Admission neurophysiological abnormalities in Guillain-Barré syndrome: a single-center experience. Clin Neurol Neurosurg. 2015; 135:6–10.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download