1. Boivin DB, Boudreau P. Impacts of shift work on sleep and circadian rhythms. Pathol Biol (Paris). 2014; 62:292–301.
2. Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE, Janszky I, Mrkobrada M, Parraga G, Hackam DG. Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012; 345:e4800.
4. Szosland D. Shift work and metabolic syndrome, diabetes mellitus and ischaemic heart disease. Int J Occup Med Environ Health. 2010; 23:287–291.
5. Ye HH, Jeong JU, Jeon MJ, Sakong J. The association between shift work and the metabolic syndrome in female workers. Ann Occup Environ Med. 2013; 25:33.
6. Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, Telama R, Juonala M, Viikari JS, Raitakari OT, et al. Shift work in young adults and carotid artery intima-media thickness: the Cardiovascular Risk in Young Finns study. Atherosclerosis. 2009; 205:608–613.
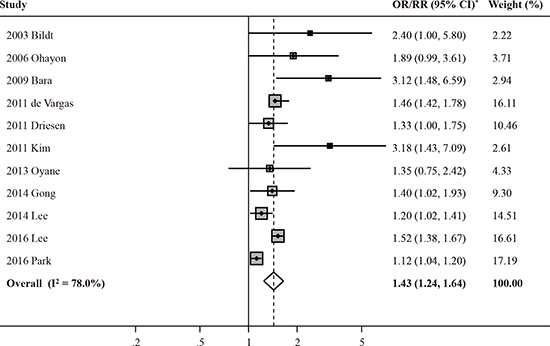
7. Bildt C, Michélsen H. Gender differences in the effects from working conditions on mental health: a 4-year follow-up. Int Arch Occup Environ Health. 2002; 75:252–258.
8. Ohayon MM, Hong SC. Prevalence of major depressive disorder in the general population of South Korea. J Psychiatr Res. 2006; 40:30–36.
9. Bara AC, Arber S. Working shifts and mental health--findings from the British Household Panel Survey (1995–2005). Scand J Work Environ Health. 2009; 35:361–367.
10. de Vargas D, Dias AP. Depression prevalence in intensive care unit nursing workers: a study at hospitals in a northwestern city of São Paulo State. Rev Lat Am Enfermagem. 2011; 19:1114–1121.
11. Driesen K, Jansen NW, van Amelsvoort LG, Kant I. The mutual relationship between shift work and depressive complaints--a prospective cohort study. Scand J Work Environ Health. 2011; 37:402–410.
12. Kim I, Heo HT, Kim S, Jang S. Night duty and depressive symptoms of white collar workers in the public sector. Occup Environ Med. 2011; 68:A100–A101.
13. Øyane NM, Pallesen S, Moen BE, Akerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One. 2013; 8:e70228.
14. Gong Y, Han T, Chen W, Dib HH, Yang G, Zhuang R, Chen Y, Tong X, Yin X, Lu Z. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS One. 2014; 9:e103242.
15. Lee SG, Kim I, Kim D. Workplace violence and depressive symptomatology among police officer. Occup Environ Med. 2014; 71:A76.
16. Lee HY, Kim MS, Kim O, Lee IH, Kim HK. Association between shift work and severity of depressive symptoms among female nurses: the Korea Nurses’ Health Study. J Nurs Manag. 2016; 24:192–200.
17. Park JN, Han MA, Park J, Ryu SY. Prevalence of depressive symptoms and related factors in Korean employees: the Third Korean Working Conditions Survey (2011). Int J Environ Res Public Health. 2016; 13:424.
18. Lexis MA, Jansen NW, van Amelsvoort LG, van den Brandt PA, Kant I. Depressive complaints as a predictor of sickness absence among the working population. J Occup Environ Med. 2009; 51:887–895.
19. Smolensky MH, Hermida RC, Reinberg A, Sackett-Lundeen L, Portaluppi F. Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol Int. 2016; 33:1101–1119.
20. Baba M, Ohkura M, Koga K, Nishiuchi K, Herrera LR, Matsuse R, Inoue T. Analysis of salivary cortisol levels to determine the association between depression level and differences in circadian rhythms of shift-working nurses. J Occup Health. 2015; 57:237–244.
21. Berthelsen M, Pallesen S, Magerøy N, Tyssen R, Bjorvatn B, Moen BE, Knardahl S. Effects of psychological and social factors in shiftwork on symptoms of anxiety and depression in nurses: a 1-year follow-up. J Occup Environ Med. 2015; 57:1127–1137.
22. Maghsoudipour M, Saberi H. Sleep disorders and depression in shift workers in comparison with day workers. Sleep. 2011; 34 Abstr Suppl:A165.
23. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–1558.
24. Simmonds M. Quantifying the risk of error when interpreting funnel plots. Syst Rev. 2015; 4:24.
25. Meyer-Lindenberg A. Neural connectivity as an intermediate phenotype: brain networks under genetic control. Hum Brain Mapp. 2009; 30:1938–1946.
26. Alasaari JS, Lagus M, Ollila HM, Toivola A, Kivimäki M, Vahtera J, Kronholm E, Härmä M, Puttonen S, Paunio T. Environmental stress affects DNA methylation of a CpG rich promoter region of serotonin transporter gene in a nurse cohort. PLoS One. 2012; 7:e45813.
27. Hall BS, Moda RN, Liston C. Glucocorticoid mechanisms of functional connectivity changes in stress-related neuropsychiatric disorders. Neurobiol Stress. 2015; 1:174–183.
28. Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000; 23:477–501.
29. Antunes LC, Jornada MN, Ramalho L, Hidalgo MP. Correlation of shift work and waist circumference, body mass index, chronotype and depressive symptoms. Arq Bras Endocrinol Metabol. 2010; 54:652–656.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download