1. Brokaw EB, Nichols D, Holley RJ, Lum PS. Robotic therapy provides a stimulus for upper limb motor recovery after stroke that is complementary to and distinct from conventional therapy. Neurorehabil Neural Repair. 2014; 28:367–376.
2. Klamroth-Marganska V, Blanco J, Campen K, Curt A, Dietz V, Ettlin T, Felder M, Fellinghauer B, Guidali M, Kollmar A, et al. Three-dimensional, task-specific robot therapy of the arm after stroke: a multicentre, parallel-group randomised trial. Lancet Neurol. 2014; 13:159–166.
3. Ren Y, Kang SH, Park HS, Wu YN, Zhang LQ. Developing a multi-joint upper limb exoskeleton robot for diagnosis, therapy, and outcome evaluation in neurorehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2013; 21:490–499.
4. Shin JH, Kim MY, Lee JY, Jeon YJ, Kim S, Lee S, Seo B, Choi Y. Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomized controlled trial. J Neuroeng Rehabil. 2016; 13:17.
5. Timmermans AA, Lemmens RJ, Monfrance M, Geers RP, Bakx W, Smeets RJ, Seelen HA. Effects of task-oriented robot training on arm function, activity, and quality of life in chronic stroke patients: a randomized controlled trial. J Neuroeng Rehabil. 2014; 11:45.
6. Novak D, Nagle A, Keller U, Riener R. Increasing motivation in robot-aided arm rehabilitation with competitive and cooperative gameplay. J Neuroeng Rehabil. 2014; 11:64.
7. Babaiasl M, Mahdioun SH, Jaryani P, Yazdani M. A review of technological and clinical aspects of robot-aided rehabilitation of upper-extremity after stroke. Disabil Rehabil Assist Technol. 2016; 11:263–280.
8. Dohle C, Püllen J, Nakaten A, Küst J, Rietz C, Karbe H. Mirror therapy promotes recovery from severe hemiparesis: a randomized controlled trial. Neurorehabil Neural Repair. 2009; 23:209–217.
9. Hamzei F, Läppchen CH, Glauche V, Mader I, Rijntjes M, Weiller C. Functional plasticity induced by mirror training: the mirror as the element connecting both hands to one hemisphere. Neurorehabil Neural Repair. 2012; 26:484–496.
10. Pervane Vural S, Nakipoglu Yuzer GF, Sezgin Ozcan D, Demir Ozbudak S, Ozgirgin N. Effects of mirror therapy in stroke patients with complex regional pain syndrome type 1: a randomized controlled study. Arch Phys Med Rehabil. 2016; 97:575–581.
11. Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror therapy for improving motor function after stroke. Stroke. 2013; 44:e1–2.
12. Crossman AR, Neary D. Neuroanatomy: an Illustrated Colour text. 5th ed. New York, NY: Churchill Livingstone;2015.
13. De Santis D, Zenzeri J, Casadio M, Masia L, Riva A, Morasso P, Squeri V. Robot-assisted training of the kinesthetic sense: enhancing proprioception after stroke. Front Hum Neurosci. 2015; 8:1037.
14. Semrau JA, Herter TM, Scott SH, Dukelow SP. Robotic identification of kinesthetic deficits after stroke. Stroke. 2013; 44:3414–3421.
15. Smorenburg AR, Ledebt A, Deconinck FJ, Savelsbergh GJ. Practicing a matching movement with a mirror in individuals with spastic hemiplegia. Res Dev Disabil. 2013; 34:2507–2513.
16. Beom J, Koh S, Nam HS, Kim W, Kim Y, Seo HG, Oh BM, Chung SG, Kim S. Robotic mirror therapy system for functional recovery of hemiplegic arms. J Vis Exp. 2016; e54521.
17. Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther. 1993; 73:447–454.
18. Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987; 67:206–207.
19. Beom J, Jang HJ, Han TR, Oh BM, Paik NJ, Yang EJ, Lee SU. Fatty replacement of rotator cuff in brain-injured patients is associated with hemiplegic arm function, but not with tendon tear: a multicenter study. NeuroRehabilitation. 2015; 37:213–219.
20. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989; 42:703–709.
21. Hillier S, Immink M, Thewlis D. Assessing proprioception: a systematic review of possibilities. Neurorehabil Neural Repair. 2015; 29:933–949.
22. Prescott RJ, Garraway WM, Akhtar AJ. Predicting functional outcome following acute stroke using a standard clinical examination. Stroke. 1982; 13:641–647.
23. Hesse S, Schulte-Tigges G, Konrad M, Bardeleben A, Werner C. Robot-assisted arm trainer for the passive and active practice of bilateral forearm and wrist movements in hemiparetic subjects. Arch Phys Med Rehabil. 2003; 84:915–920.
24. Lum PS, Burgar CG, Van der Loos M, Shor PC, Majmundar M, Yap R. MIME robotic device for upper-limb neurorehabilitation in subacute stroke subjects: a follow-up study. J Rehabil Res Dev. 2006; 43:631–642.
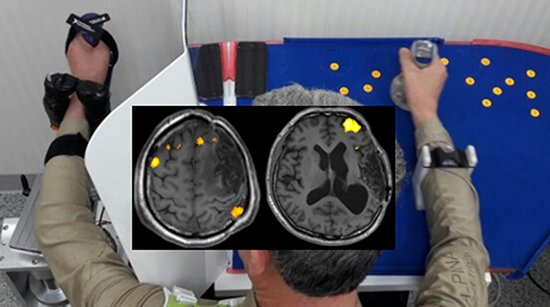
25. Marins TF, Rodrigues EC, Engel A, Hoefle S, Basílio R, Lent R, Moll J, Tovar-Moll F. Enhancing motor network activity using real-time functional MRI neurofeedback of left premotor cortex. Front Behav Neurosci. 2015; 9:341.
26. Pandian JD, Arora R, Kaur P, Sharma D, Vishwambaran DK, Arima H. Mirror therapy in unilateral neglect after stroke (MUST trial): a randomized controlled trial. Neurology. 2014; 83:1012–1017.
27. Thieme H, Bayn M, Wurg M, Zange C, Pohl M, Behrens J. Mirror therapy for patients with severe arm paresis after stroke--a randomized controlled trial. Clin Rehabil. 2013; 27:314–324.
28. Wang W, Zhang X, Ji X, Ye Q, Chen W, Ni J, Shen G, Zhang B, Yuan TF, Shan C. Mirror neuron therapy for hemispatial neglect patients. Sci Rep. 2015; 5:8664.
29. Seo HG, Beom J, Oh BM, Han TR. Effects of robot-assisted upper limb training on hemiplegic patients. Brain Neurorehabil. 2014; 7:39–47.
30. Choi YS, Lee KW, Lee JH, Kim SB, Park GT, Lee SJ. The effect of an upper limb rehabilitation robot on hemispatial neglect in stroke patients. Ann Rehabil Med. 2016; 40:611–619.
31. Kraft E, Schaal MC, Lule D, König E, Scheidtmann K. The functional anatomy of motor imagery after sub-acute stroke. NeuroRehabilitation. 2015; 36:329–337.
32. Bhasin A, Padma Srivastava MV, Kumaran SS, Bhatia R, Mohanty S. Neural interface of mirror therapy in chronic stroke patients: a functional magnetic resonance imaging study. Neurol India. 2012; 60:570–576.
33. Diers M, Kamping S, Kirsch P, Rance M, Bekrater-Bodmann R, Foell J, Trojan J, Fuchs X, Bach F, Maaß H, et al. Illusion-related brain activations: a new virtual reality mirror box system for use during functional magnetic resonance imaging. Brain Res. 2015; 1594:173–182.
34. Fritzsch C, Wang J, Dos Santos LF, Mauritz KH, Brunetti M, Dohle C. Different effects of the mirror illusion on motor and somatosensory processing. Restor Neurol Neurosci. 2014; 32:269–280.
35. Guo F, Xu Q, Abo Salem HM, Yao Y, Lou J, Huang X. The neuronal correlates of mirror therapy: A functional magnetic resonance imaging study on mirror-induced visual illusions of ankle movements. Brain Res. 2016; 1639:186–193.
36. Wang J, Fritzsch C, Bernarding J, Krause T, Mauritz KH, Brunetti M, Dohle C. Cerebral activation evoked by the mirror illusion of the hand in stroke patients compared to normal subjects. NeuroRehabilitation. 2013; 33:593–603.
37. Holmes NP, Spence C. Visual bias of unseen hand position with a mirror: spatial and temporal factors. Exp Brain Res. 2005; 166:489–497.
38. Moseley GL, Gallace A, Spence C. Is mirror therapy all it is cracked up to be? Current evidence and future directions. Pain. 2008; 138:7–10.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download