Abstract
Surgery has been the standard treatment for perforated duodenal ulcers, with mostly good results. However, the resolution of postoperative leakage after primary repair of perforated duodenal ulcer remains challenging. There are several choices for re-operation required in persistent leakage from perforated duodenal ulcers. However, many of these choices are complicated surgical procedures requiring prolonged general anesthesia that may increase the chances of morbidity and mortality. Several recent reports have demonstrated postoperative leakage after primary repair of a perforated duodenal ulcer treated with endoscopic insertion using a covered self-expandable metallic stent, with good clinical results. We report a case with postoperative leakage after primary repair of a perforated duodenal ulcer treated using a covered self-expandable metallic stent.
The incidence of duodenal ulcer perforation has been reduced since the distribution of commercialized histamine-2 receptor blockers and proton pump inhibitors; however, ulcer-related mortality remains to be an issue. Duodenal ulcer perforation requires emergency surgery and is usually well controlled when initially treated with surgical intervention. However, postoperative leakage has been associated with morbidity as it requires re-operation with prolonged general anesthesia time and severe inflammation, which leads to a challenging problem for surgeons.12
Therefore, presently, surgeons are seeking alternative methods to treating postoperative leakage. One such effort is covered self-expandable metallic stent (SEMS) insertion using endoscopy. Recently, covered SEMS insertion as a treatment for postoperative leakage after duodenal ulcer perforation surgery or other gastrointestinal tract surgery has been studied.34567 We report a case of endoscopic insertion of a covered SEMS as a rescue procedure for postoperative leakage after primary repair of perforated duodenal ulcer.
A 69-year-old man presented to the emergency department with abdominal pain and distention for three days. He only had a history of hypertension and no specified abdominal operation history. He was admitted to a local hospital three days prior; but only symptom control was performed. At admission, he was in septic shock, and physical examination revealed direct tenderness and rebound tenderness of the whole abdomen. Laboratory data showed the following: white blood cell count of 8,440/µL with an elevated neutrophil segment of 81.7%; erythrocyte sedimentation rate of 110 mm/hr; and C-reactive protein level of 45.07 mg/dL. Abdominopelvic CT showed ulcer perforation at the anterior wall of the duodenal first portion with peritonitis. Esophagogastroduodenoscopy performed at a previous local hospital demonstrated a huge ulcer with perforation at the first portion of the duodenum (Fig. 1). The patient was initially treated with antibiotics and fluid resuscitation.
We immediately performed emergency surgery. In the operation room, a 3-cm-sized ulcer perforation with severe inflammation was found. Primary repair of the duodenal ulcer perforation was performed. However, the surrounding tissue of the perforation area was friable, making it difficult to suture. Additionally, we found severe intra-abdominal inflammation with gastric content spillage and massive irrigation with normal saline. However, omentopexy could not be performed due to omental cake causing severe inflammation. Thus, the fibrin sealant (Tisseel, Baxter International Inc., Westlake Village, CA, USA) and absorbable polyglycolic acid sheet (Neoveil, Gunze Ltd., Kyoto, Japan) were applied inevitably above the primary repair site in order that enhances the strength of sutures and prevents postoperative leakage. Additionally, a negative suction drain was placed in the subhepatic area, primary repair site, and pelvic cavity.
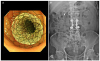
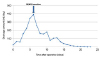
At postoperative day 3, fresh bile drainage in the negative suction drain was noted, and fever spiked to 38.1℃. At postoperative day 5, diatrizoate sodium and diatrizoate meglumine solution (Gastrografin, Bayer Schering Pharma, Berlin, Germany) procedure was performed, and the diatrizoate sodium and diatrizoate meglumine solution leakage at the primary repair site was identified (Fig. 2). We decided on a multidisciplinary team to manage the problem and discussed with a gastroenterologist. After the meeting, we concluded that the endoscopic insertion of covered stent would be an alternative treatment for postoperative leakage. At postoperative day 6, a 6-cm-sized covered SEMS (Taewoong Medical, Seoul, Korea) was applied gently on the leakage site with fluoroscopic assistance (Fig. 3). After SEMS insertion, the patient was tolerable, and a decreased frequency of fever spiking was noted. Additionally, the amount of drainage in the negative suction drain had decreased to below 50 mL/day after 7 days of SEMS insertion (Fig. 4). The stent was removed by esophagogastroduodenoscopy with endoscopic snare at postoperative day 35, and on the following day, the patient was discharged in good condition.
Surgery is widely used as the first-line treatment for duodenal ulcer perforation.8 However, postoperative leakage is a life-threatening complication, and leakage rates remain high (2–16%).1910 In addition, re-operation of postoperative leakage is technically difficult and challenging for older patients and those with co-morbidity and poor general condition at immediate post-operation.7 However, our case demonstrated that it may be possible to use endoscopic-covered SEMS insertion as a rescue treatment for perforated duodenal ulcer with postoperative leakage. Moreover, there was no complication associated with SEMS.
Endoscopic stent insertion is an attractive alternative to surgery. Re-operation is a burdensome procedure to surgeons, especially for those with poor general condition and comorbidities. Endoscopic stent insertion may be advantageous in that patients do not require general anesthesia and it can be performed in patients with poor general condition. Therefore, endoscopic stent placement is already a standard procedure, mainly for intestinal strictures; however, it is now also an approved treatment for esophageal perforations.1112 Additionally, endoscopic stent insertion allows early oral intake, which decreases the need for parenteral nutrition and risk of bacterial translocation from the gut, facilitating early recovery.13
However, despite many of its advantages, endoscopic SEMS insertion also has several disadvantages compared with surgery. There is a potential risk that esophagogastroduodenoscopy may aggravate the perforation or leakage by gas insufflation.14 In addition, SEMS insertion offers the disadvantages of stent-induced stenosis and ulcer aggravation.715 A major drawback of the procedure is distal migration of the stent. Previous study reported stent removal through operation due to stent migration at the small bowel.16 Therefore, SEMS may be removed early before the development of complications associated with stents. Furthermore, frequent check by abdominal X-ray should be performed after SEMS insertion to confirm the stent location and prevent its migration to the small bowel.
Despite its advantages, whether covered SEMS insertion with simultaneous abdominal drainage will replace surgery as the primary treatment method of duodenal ulcer perforation remains uncertain.1718 Bergström et al.2 demonstrated favorable results of primary covered SEMS insertion with abdominal drainage in patients with perforated duodenal ulcer and comorbidities or technically difficult surgery. However, the procedure was only performed in a few patients, and further research may be required. Thus, surgery should still be considered as the primary mode of treatment in patients with a preserved performance status and early detection of duodenal ulcer perforation to achieve early recovery. Additionally, endoscopic SEMS insertion with simultaneous abdominal drainage may be an alternative to surgery only in patients with severe co-morbidities or delayed diagnosis.
The current report demonstrated that endoscopic covered SEMS insertion can be used as a rescue treatment for a perforated duodenal ulcer with postoperative leakage after primary repair. Endoscopic SEMS insertion is a less invasive procedure comparing re-operation and increased survival chance for patients with co-morbidities or technically difficult surgery. Thus, endoscopic covered SEMS insertion may be an alternative procedure for re-operation in selected patients with postoperative leakage after primary repair of duodenal ulcer perforation.
Figures and Tables
 | Fig. 1Preoperative endoscopic examination demonstrating a 3-cm-sized ulcer perforation at the first portion of the duodenum covered by yellowish debris tissue. |
 | Fig. 2Abdomen X-ray findings and esophagogastroduodenoscopy before SEMS insertion. (A) The diatrizoate sodium and diatrizoate meglumine solution procedure demonstrating leakage in the primary repair site of the duodenal ulcer perforation. (B) Esophagogastroduodenoscopy showing a huge ulcer in the first portion of the duodenum with suture material and absorbable polyglycolic acid sheet. SEMS, self-expandable metallic stent. |
References
1. Gupta S, Kaushik R, Sharma R, Attri A. The management of large perforations of duodenal ulcers. BMC Surg. 2005; 5:15.

2. Bergström M, Arroyo Vázquez JA, Park PO. Self-expandable metal stents as a new treatment option for perforated duodenal ulcer. Endoscopy. 2013; 45:222–225.

3. Eubanks S, Edwards CA, Fearing NM, et al. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg. 2008; 206:935–938. discussion 938-939.

4. Puli SR, Spofford IS, Thompson CC. Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc. 2012; 75:287–293.

5. Schubert D, Scheidbach H, Kuhn R, et al. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005; 61:891–896.

6. Serra C, Baltasar A, Andreo L, et al. Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy. Obes Surg. 2007; 17:866–872.

7. Swinnen J, Eisendrath P, Rigaux J, et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc. 2011; 73:890–899.

9. Søreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg. 2014; 101:e51–e64.

10. Lunevicius R, Morkevicius M. Management strategies, early results, benefits, and risk factors of laparoscopic repair of perforated peptic ulcer. World J Surg. 2005; 29:1299–1310.

11. Kim KY, Tsauo J, Song HY, Kim PH, Park JH. Self-expandable metallic stent placement for the palliation of esophageal cancer. J Korean Med Sci. 2017; 32:1062–1071.

12. Johnsson E, Lundell L, Liedman B. Sealing of esophageal perforation or ruptures with expandable metallic stents: a prospective controlled study on treatment efficacy and limitations. Dis Esophagus. 2005; 18:262–266.

13. Reintam Blaser A, Starkopf J, Alhazzani W, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2017; 43:380–398.

14. Chertoff J, Khullar V, Burke L. Duodenal perforation following esophagogastroduodenoscopy (EGD) with cautery and epinephrine injection for peptic ulcer disease: an interesting case of nonoperative management in the medical intensive care unit (MICU). Int J Surg Case Rep. 2015; 10:121–125.

15. Wai CT, Khor C, Lim SE, Ho KY. Post-metallic stent placement bleeding caused by stent-induced ulcers. World J Gastroenterol. 2005; 11:5739–5741.

16. Holm TE, Rosseland AR, Lundin KA, et al. Endoscopic stent treatment of a duodenal ulcer perforation. Endoscopy. 2011; 43:Suppl 2 UCTN. E60.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download