Abstract
A 60-year-old male presented with a three-month history of redness and swelling on his left little finger. His medical history was not informative. Wound culture revealed methicillin-resistant Staphylococcus aureus. After vancomycin administration, the skin lesions became worse and whole body bullae and desquamation occurred. This was initially suspected to be a drug eruption; thus, we switched antibiotics from vancomycin to teicoplanin. However, biopsy revealed Staphylococcal scalded skin syndrome (SSSS). After several days, generalized skin symptoms improved. The patient recovered and is in good physical health without recurrence six months later. We describe a localized form of SSSS, which is very rare in healthy adults. Consequently, there is a high risk of misdiagnosis. Thus, we report a rare case of SSSS in a healthy adult and the importance of early histological examination for accurate diagnosis.
Staphylococcal scalded skin syndrome (SSSS) is a generalized exanthematous disease with symptoms including cutaneous tenderness and broad superficial blistering and denudation. SSSS is caused by bacterial exotoxins A and B, which are released from Staphylococcus aureus and cause detachment of desmoglein within the epidermal layer1. Epidermolysis usually takes place between the stratum spinosum and granulosum1.
Although it is more commonly seen in infants and children, SSSS can also occur in adults1, in whom its rare appearance is usually associated with kidney failure, malignancy or immunosuppression. The case described herein is of interest because of its onset in a healthy adult and its mild clinical course.
A 60-year-old male presented with a three-month history of redness and swelling on his left little finger. He had a history of local trauma with sharp metal three months prior. Since then, the redness and swelling had slowly extended to the whole finger. He had undergone antibiotic treatment at a local clinic without symptom improvement. His medical history was not informative. In order to differentiate from bacterial tenosynovitis, physical examination was performed. On the initial physical examination, hand range of motion was in normal range. His finger did not hold in flexion position and there was no pain aggravation when passive extension. At the time of hospitalization, his body temperature was 37.4℃. Erythema with generalized small erythematous punctiform eruptions were present on the little finger (Fig. 1) and there were no radiologic abnormalities (Fig. 2). Routine laboratory tests did not reveal any abnormalities, other than slight inflammatory signs: C-reactive protein, 0.78 mg/dL and erythrocyte sedimentation rate, 40 mm/hr. The patient was negative for HIV antibody and other immunological examinations did not reveal any abnormalities. He was hospitalized and wound culture was performed. Empirical intravenous antibiotics (cephazedone+nesomicin) were used for cellulitis treatment. On hospital day 4, wound culture results indicated methicillin-resistant Staphylococcus aureus (MRSA). Skin symptoms had not improved (Fig. 3). Therefore, the antibiotic regimen was switched to vancomycin. After 3 days of vancomycin use, the patient developed a generalized fever, skin bullae on the trunk (Fig. 4), and desquamation of the top layers of skin, clear yellowish discharge on the left hand. Initially, we assumed this indicated a drug allergy and treated the patient with intravenous anti-histamines and steroids; however, there was no response. Five days later, skin desquamation and discharge had worsened (Fig. 5), with multiple bullae and desquamation extending to the whole hand. Therefore, to rule out drug eruption, such as Stevens-Johnson syndrome (SJS) related to vancomycin, as a possible cause, we performed skin biopsy. Meanwhile, antibiotic treatment was switch to teicoplanin. After several days, generalized skin symptoms improved progressively, and skin biopsy results indicated SSSS (Fig. 6). Since the patient was already treating with strong antibiotics to cover the MRSA, we observed the progress while continuing the same treatment. He was responding to antibiotic treatment and showed improved symptoms. Patient discharged from the hospital and returned for outpatient follow-up. He is in good physical health without recurrence 6 months later (Fig. 7).
SSSS is the clinical term that used for a spectrum of blistering skin diseases induced by exfoliative toxins type A or B from S. aureus. The severity of SSSS varies from a few blisters in localized SSSS to severe exfoliation affecting most of the body surface in generalized SSSS. SSSS can occur at any age but it is the most common in children less than 5 years of age12.
As opposed to pediatric patients who are usually in otherwise good health when they develop SSSS34, virtually all adult cases of SSSS occur in those who are immunocompromised due to chronic renal disease, HIV infection, malignant neoplasms, chemotherapy, intravenous drug abuse or diabetes mellitus. Similar to pediatric patients, adults with SSSS demonstrate a fever, erythema, bullae formation and desquamation of the skin. Possibly as a result of underlying morbidities, adults with SSSS have a mortality rate of 40%–63%56.
SSSS typically needs to be distinguished from drug eruption, as skin bullae and desquamation are common clinical symptoms. In particular, severe drug eruptions, known as toxic epidermal necrolysis (TEN) or SJS, need to be distinguished from SSSS. In adults, both TEN and SSSS have a high mortality rate and require different treatment. Clinician awareness of SSSS is important in early diagnosis and treatment.
To differentiate SSSS from TEN, findings suggestive of SSSS include striking cutaneous tenderness, positive Nikolsky sign, and lack of mucosal involvement. In TEN, ulcerated mucosa is common, but diagnosis is not possible from clinical features alone (Table 1)6. A biopsy is necessary for accurate differential diagnosis.
In this case, we first suspected as TEN because the patient was a healthy adult without renal failure. Although the period of infection was long, there was no systemic skin symptom. Systemic symptoms–such as Nicolsky's sign–appeared after using vancomycin. However, we could not stop the antibiotics because of the possibility of SSSS. So we replaced the antibiotics with another things and performed skin punch biopsy immediately. As result of biopsy, SSSS was confirmed. And Bacterial culture result also revealed as MRSA. Consequently, the patient was cured by proper antibiotics usage.
Once diagnosed as SSSS, hospitalization, rehydration and intravenous systemic antibiotic therapy become the principle of treatment. As the review of the literature, S. aureus was isolated from skin lesions in many adult patients7. In case of our patient, MRSA was found in wound culture. There were some cases caused by methicillin-resistant S. aureus have been reported89. Comprehensively, early wound culture to find the causative bacteria and using the suitable antibiotics are best treatment of choice. Early strong antibiotics usage can lead to good results.
This patient exhibited systemic skin vesicles, multiple bullae, desquamation of the left small finger and a slight increase in inflammation. We suspected drug eruption because of wound aggravation after 3 days of vancomycin treatment. We stopped vancomycin, which was thought to be the causative drug, and switched treatment to teicoplanin. We also performed a biopsy for differential diagnosis. Because of the diagnosis of SSSS on histological examination, antibiotics were continued.
Optimal treatment from drug eruption, such as SJS and TEN, is to stop the causative drug. However, treatment of SSSS requires continuing antibiotic therapy. Drug eruption and SSSS have similar symptoms but differing treatment. If these diseases cannot be differentiated, high mortality can occur in adult patients. Adults, whitish blister color, full thickness epidermal necrosis suggest that TEN rather than SSSS but the differential diagnosis of scaled-skin lesions in healthy adults can be difficult; thus, reliable histologic examination is particularly important in SSSS and TEN. It is very important that mortality rate is up to 35% high in TEN and 63% in SSSS. Early histological examination for correct diagnosis is the most important and that can lead to better result.
We think it may be meaningful report to predict the rare case of SSSS which was clinically mild course on healthy adult.
In this case, it is meaningful because the possibility of infection by exfoliative toxin B cannot be ruled out. When a patient present with generalized symptoms such as skin bullae and desquamation, drug eruptions are typically suspected. However, clinicians should consider SSSS in cases of S. aureus infection and be aware of the need for prompt biopsy to ensure an accurate and timely diagnosis.
Figures and Tables
Fig. 4
Hospital day 7. After 3 days of vancomycin use, multiple bullae on the whole body was appeared. (A) Left lateral chest. (B) Back and sacral area.

Fig. 5
Hospital day 12. Skin desquamation and discharge on left hand were even worse. (A) Dorsal side. (B) Palmar aspect.

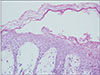
Fig. 6
Skin biopsy result. Subcorneal splitting of the epidermis with superficial epidermal necrosis is seen. There are few inflammatory cells within the bulla cavity and there is only slight damage to the underlying epidermal cells. It suggests staphylococcal scalded skin syndrome (H&E, ×100).
References
1. Fitzpatrick TB, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw Hill Medical;2012. p. 2148–2160.
2. Miyashita K, Ogawa K, Iioka H, et al. Adult case of Saphylococcal scalded skin syndrome differentiated from toxic epidermal necrolysis with the aid of dermoscopy. J Dermatol. 2016; 43:842–843.
3. Aydin D, Alsbjørn B. Severe case of Saphylococcal scalded skin syndrome in a 5-year-old child - case report. Clin Case Rep. 2016; 4:416–419.
4. Mishra AK, Yadav P, Mishra A. A systemic review on Staphylococcal scalded skin syndrome (SSSS): a rare and critical disease of neonates. Open Microbiol J. 2016; 10:150–159.

5. Cribier B, Piemont Y, Grosshans E. Staphylococcal scalded skin syndrome in adults. A clinical review illustrated with a new case. J Am Acad Dermatol. 1994; 30:319–324.
6. Badon HR, King J, Brodell RT, Byrd A. Distinguishing features: Staphylococcal scalded skin syndrome vs toxic epidermal necrolysis. SKIN J Cutan Med. 2018; 2:135–139.

7. Patel GK, Finlay AY. Staphylococcal scalded skin syndrome: diagnosis and management. Am J Clin Dermatol. 2003; 4:165–175.
8. Ito Y, Funabashi Yoh M, Toda K, Shimazaki M, Nakamura T, Morita E. Staphylococcal scalded-skin syndrome in an adult due to methicillin-resistant Staphylococcal aureus. J Infect Chemother. 2002; 8:256–261.
9. Yamaguchi T, Yokota Y, Terajima J, et al. Clonal association of Staphylococcus aureus causing bullous impetigo and the emergence of new methicillin-resistant clonal groups in Kansai district in Japan. J Infect Dis. 2002; 185:1511–1516.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download