Abstract
Purpose
We investigated occurrence of reduction loss after extension block (EB) Kirschner wire fixation or additional interfragmentary fixation (AIF) and clinical results including extension lag of the distal interphalangeal joint for treating bony mallet finger.
Methods
Forty-six patients were included with a mean follow-up of 28 months (range, 12–54 months). Twenty-seven patients were treated with EB K-wire fixation (Group A) while 19 patients were treated with AIF (Group B). We checked radiologic factors, such as amount of articular involvement, volar subluxation, mallet fragment angle, reduction loss, range of motion including extension lag, and functional outcomes using Crawford's criteria.
Results
Reduction loss occurred in eight patients (17%). Differences in mean extension lag, age, preoperative volar subluxation and mallet fragment angle between patients with reduction loss and those with reduction maintaining were significant. However, there were no significant differences in gender, hand dominance, amount of articular involvement, AIF, or further flexion between reduction loss and reduction maintaining. As for patterns of displacement, there was a significant relationship between gap or step-off and extension lag. Using Crawford's evaluation criteria, functional outcomes were excellent in 31, good in 10, fair in 3, and poor in 2 patients.
Extension block (EB) Kirschner wire (K-wire) fixation is a convenient technique and the most commonly used operative procedure for treating bony mallet finger1234567. However, there are some problems associated with the accuracy of reduction and stability of fixation. Several authors have reported various modified EB techniques including additional fixation to reduce the gap between distal phalanx and dorsal fragment1689.
Although anatomic reduction is achieved immediate postoperatively, reduction loss can occasionally occur until bony union. The gap between the distal phalanx and dorsal fragment may be associated with extension lag10. Residual displacement immediately postoperatively has been reported to be a prognostic factor11. However, to our knowledge, reduction loss after treatment of bony mallet finger has not been reported yet. Reduction loss also leads to malunion which may cause extension lag of the distal interphalangeal (DIP) joint, although remodeling of DIP joint may occur.
For this reason, we analyzed the relationship between reduction loss and extension lag of the DIP joint. In this study, we investigated occurrence of reduction loss after EB K-wire fixation or additional interfragmentary fixation (AIF) for the treatment of bony mallet finger and evaluated clinical results including extension lag of the DIP joint.
The first hypothesis of this study was that reduction loss after EB K-wire fixation for bony mallet finger would increase extension lag. The second hypothesis was that AIF would effectively prevent reduction loss in the treatment of bony mallet finger.
This study was approved by the Institutional Review Board of our hospital. This retrospective study was performed from November 2004 to June 2014. Patients with bony mallet finger deformity were treated by modified EB K-wire fixation. The inclusion criteria of modified EB K-wire fixation were: (1) a dorsal intra-articular fracture fragment involving more than one-third of the base of the distal phalanx, (2) volar subluxation of the DIP joint, or (3) step-off of >1 mm between the dorsal fragment and distal phalanx with an extension DIP splint. Seventy patients were eligible for this criteria. Patients with osteoarthritic change of the DIP joint (n=1), neglected mallet finger deformity (n=2) (untreated cases more than 8 weeks after injury) and less than 1 year follow-up (n=21) were excluded. So 46 patients were included among 70 patients excluding 24 patients. All patients were assessed for reduction loss. Radiographic images were taken immediately after surgery and at 2, 4, 6, and 8 weeks, and then every 6 months after union. Images were reviewed by two different orthopedic surgeons. All patients were assessed for extension lag at 3 months postoperatively and at the last follow-up.
Forty-six (66%) of 70 patients with a minimum followup of 1 year were included. The mean follow-up was 28 months (range, 12–54 months) excluding 21 patients because of follow-up loss. Twenty-seven patients were treated with EB K-wire fixation (Group A) while 19 patients were treated with AIF (Group B). We inserted additional interfragmentary K-wire to improve quality of reduction when the reduction was not satisfactory or to increase stability when bony fragment seemed to be unstable despite EB K-wire fixation. There were 29 males and 15 females with a mean age of 29 years (range, 17–53 years). The mean time from injury to surgery was 16 days (range, 4–48 days). When the reduction was delayed more than 4 weeks, we inserted 23-G needle into the fracture gap to remove hematoma and freshen the fracture site.
Thirty-two patients had right-sided injury and 14 had left-sided injury. The most common mechanism for injury was fall (26 patients), followed by volleyball (9 patients), basketball (5 patients), traffic accident (4 patients), and soccer (2 patients). The ring finger was the most commonly affected (17 patients), followed by the small finger (11 patients), index finger (11 patients), and long finger (7 patients).
All patients were assessed with respect to the time to radiological union, residual pain using visual analogue scale, and range of motion at the DIP joint recorded with a goniometer. Functional outcomes were assessed using Crawford's criteria12. Extension lag was defined as a >10° limitation of DIP active extension. We classified the pattern of displacement between the distal phalanx and dorsal fragment on a true lateral radiograph into step-off, gap, and rotation irrespective of existence of reduction loss. Step-off was defined as displacement of more than 1 mm in the longitudinal direction. A gap was defined as displacement of more than 1 mm in the anteroposterior direction. Rotation was defined as rotation of more than 10° of the dorsal fragment (Fig. 1). Reduction loss was defined as change of step-off more than 1 mm, gap displacement more than 1 mm, and rotation more than 10° between the distal phalanx and dorsal fragment on a true lateral radiograph comparing radiograph immediate postoperatively with the radiograph at the time of detecting reduction loss before bony union occurred. In addition, we checked preoperative mallet fragment angle. The mallet fragment angle was defined as an acute angle between the axis of the distal phalanx and the fracture line (Fig. 2). Preoperative volar subluxation was defined as more than 2 mm of the distal phalanx volar cortex margin than the middle phalanx one. The Wehbé and Schneider13 classification was used to analyze radiological fracture type (Table 1).
The procedure was generally performed under digital block anesthesia with lateral radiography using image intensifier control. Closed manipulation was achieved by compression of the dorsal fragment with surgeon's index finger and thumb with DIP flexion and joint congruity was evaluated with DIP extension. When the joint congruity was unsatisfactory, hematoma was removed using a 23-G needle inserted from dorsum of distal phalanx into the fracture gap. Then the fracture site was freshened by swiveling the needle tip mediolaterally within the fracture site with care not to injure the middle phalanx head (Fig. 3). After satisfactory joint congruity was achieved, a 1.4-mm K-wire was inserted obliquely from the dorsal neck of the middle phalanx to the volar side of the middle phalanx to prevent dorsal displacement of dorsal fragment. A second K-wire was inserted obliquely from the radial side of the distal phalanx to the ulnar side of the middle phalanx while maintaining slightly dorsal translation and extension of the DIP joint. For Group B patients, a 0.9 or 1.1-mm K-wire was additionally inserted from the dorsal fracture fragment to the volar cortex of the distal phalanx perpendicular to the fracture surface with care not to make fracture of the fragment itself (Fig. 4). Regular dressing and pin care were encouraged and the DIP joint was immobilized using a U-shaped aluminum splint for 6 weeks. Wires were removed in the outpatient clinic at 6 weeks postoperatively with verification of radiological union. After removal of pins, active exercise of the DIP joint was then initiated with a removable night DIP extension aluminum splint for an additional two weeks to prevent further extension lag. Independent t-test were used to compare continuous variables between groups. Chi-square test were used to compare categorical value between groups or pattern of displacement.
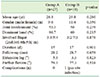
Mean radiographic bone union was 6.2 weeks (range, 5–7 weeks) based on callus between fragments. There was no statistically significant difference in age, sex, joint involvement, or time to surgery between the two groups (Table 2). The average articular surface involvement was 47.4% (10%–70%). Reduction loss occurred in 8 (17%) of 46 patients within postoperative 4 weeks (range, 2–4 weeks) (Table 3). Differences in mean extension lag, age, and mallet fragment angle between patients with reduction loss and those with reduction maintaining were significant according to the independent t-test (all p<0.05, Table 4).
Four out of 46 patients had preoperative volar subluxation (more than 2 mm) of the distal phalanx. Three of these four patients with preoperative subluxation had reduction loss (p<0.05). However there were no significant difference in gender, hand dominance, AIF, or further flexion between reduction loss and reduction maintaining (all p>0.05, Table 4).
Patients with reduction loss showed displacement patterns of gap only (n=3), step-off only (n=2), and combined (n=3) (Fig. 5, 6). For patterns of displacement, there was a significant relationship between gap (n=5) or step-off (n=5) and extension lag more than 10° (both p<0.05). However, there was no significant relationship between rotation (n=1) and extension lag more than 10° (p>0.05).
The extensor lag of the DIP joint at the last follow-up was 4.3°±9.3° (Group A, 5.3°±12.4° vs. Group B, 3.3°±6.2°, p>0.05). Further flexion of the DIP joint was 78.3°±15.1° (Group A, 79.3°±15.3° vs. Group B, 77.3°±14.9°, p>0.05). There was no statistically significant difference between the two groups.
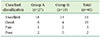
Using Crawford's evaluation criteria, functional outcomes were excellent in 31 patients (Group A, 18; Group B, 13), good in 10 patients (Group A, 6; Group B, 4), fair in 3 patients (Group A, 1; Group B, 2), and poor in 2 patients (Group A, 2; Group B, 0) (Table 5). Residual pain using visual analogue scale was 0.8 (0–2). There were no nail deformities, persistent pain, or DIP arthritis in any patient. One case of a pin-site infection was treated successfully with oral antibiotics and local wound care.
We evaluated a cohort of eight patients with reduction loss after modified EB K-wire fixation for treatment of bony mallet finger. Seven of these eight patients had extension lag of >10°. We also identified several factors related to reduction loss such as age, volar subluxation, and mallet fragment angle previously reported to be a prognostic factor for EB technique11. In contrast, AIF was not effective for preventing reduction loss.
It is important to restore joint surface by accurate reduction because it is closely related to functional outcome31415. In this study, we focused on the relationship between reduction loss and extension lag. If reduction loss occurs until bony union, extension lag could be anticipated at the final follow-up. This is critical for postoperative management.
At the final follow-up, extensor lag in patients with reduction loss differed significantly from that in patients with reduction maintaining. This supports our hypothesis that reduction loss after EB K-wire fixation for bony mallet finger can affect extension lag.
We confirmed that extension lag was dependent on the final reduction quality such as step-off or gap. However, rotation in the sagittal plane did not affect extension lag. Reduction loss caused by fragment rotation is rather related to articular incongruity which fortunately has high remodeling potential3. It is mainly caused by rotation of the dorsal fragment, not by rotation of the distal phalanx. On the other hand, the occurrence of step-off or gap was dependent upon displacement of both the dorsal fragment and distal phalanx. The reason for reduction loss is currently unclear. Single transfixing K-wire across DIP might not be sufficient to prevent sagittal or rotational movement from bending or loosening of the pin. These findings suggest that effort should be made to maintain reduction of the distal phalanx to the middle phalanx (which is dependent solely upon transfixing a single K-wire) and the dorsal fragment.
It is difficult to verify the quality of reduction in EB K-wire because it involves an indirect reduction under an image intensifier16. Several authors have described additional percutaneous procedures to increase stability of the fragment5. However, potential disadvantages of additional pin fixation should be considered. For example, it is difficult to locate the exact insertional entry point. In addition, there is potential for further soft tissue injury16. Enhancement of functional outcome related to additional pin fixation was not found in this study.
Reduction loss did not affect further flexion in our study. Further flexion is rather dependent on early mobilization of the DIP joint because extensor tendon adhesion hinders DIP joint motion6. As the number of pin tracks increases, adhesion points are added which may prevent tendon excursion3. Therefore, additional K-wires may diminish the potential advantage of fragment stability because additional K-wires could not provide enough strength to allow early DIP motion.
The limitations of this study are as follows. First, it was retrospective in design without a control group. Although standardization of the degree of injury may be difficult, a prospective randomized study is warranted. Second, age and injury mechanism could affect extension lag according to Kim and Lee17. In our study, 3 of 38 patients without reduction loss were identified to have extension lag at the last follow-up. This means that other factors might influence extension lag. Further studies are needed.
Last, reduction loss proportion in this study seems to be relatively high. We cannot exclude possibility that immediate postoperative incomplete reduction such as subtle volar subluxation (Fig. 5) or immediate postoperative less rigid DIP fixation (Fig. 4) would result in reduction loss. Some modification such as two small EB K-wires or additional intrafocal pinning techniques may improve reduction quality if immediate anatomic reduction could not be achieved318.
One case of a pin-site infection occurred in this study. Burying the tips of all pins under the skin would be helpful to prevent infection or other pin-related complications according to Shin et al.19.
Although accurate reduction was initially achieved, reduction loss after EB K-wire fixation for the treatment of bony mallet finger occasionally occurred, leading to extension lag. Reduction loss should be careful in older age, smaller mallet fragment angle and preoperative volar subluxation.
Figures and Tables
 | Fig. 1(A) Step-off was defined as more than 1 mm of displacement in the longitudinal direction. (B) Gap was defined as more than 1 mm of displacement in the anteroposterior direction. (C) Rotation was defined as more than 10 degrees in rotation of the dorsal fragment. |
 | Fig. 2Mallet fragment angle was defined as acute angle between an axis of distal phalanx and a line of fracture. |
 | Fig. 3Intraoperative fluoroscopic image showing that hematoma was removed using 23-G needle when the reduction was unsatisfactory. Satisfactory reduction was then achieved. |
 | Fig. 4(A) Patients of Group A were treated using modified extension block K-wire fixation alone. (B) Group B patients were treated by additional interfragmentary fixation. |
 | Fig. 5(A) Lateral radiograph showing a displaced mallet fracture with joint subluxation in a 22-year-old man (case number 4). (B) A postoperative radiograph showing subtle volar subluxation. (C) The 6-month follow-up radiograph showing a reduction loss with both gap and step off, resulting in volarly subluxation of distal phalanx. At the final follow-up, extension lag of the injured distal interphalangeal joint remained. |
 | Fig. 6(A) Lateral radiograph showing a displaced mallet fracture in a 49-year-old man (case number 5). (B) A postoperative radiograph showing an anatomic reduction. (C) The 6-month follow-up radiograph showing a reduction loss with step off. At the final follow-up, extension lag of the injured distal interphalangeal joint remained. |
References
1. Tetik C, Gudemez E. Modification of the extension block kirschner wire technique for mallet fractures. Clin Orthop Relat Res. 2002; (404):284–290.

2. Pegoli L, Toh S, Arai K, Fukuda A, Nishikawa S, Vallejo IG. The Ishiguro extension block technique for the treatment of mallet finger fracture: indications and clinical results. J Hand Surg Br. 2003; 28:15–17.
3. Lee YH, Kim JY, Chung MS, Baek GH, Gong HS, Lee SK. Two extension block kirschner wire technique for mallet finger fractures. J Bone Joint Surg Br. 2009; 91:1478–1481.

4. Jörgsholm P, Björkman A, Emmeluth C, Björkman-Burtscher IM. Extension block pinning of mallet fractures. Scand J Plast Reconstr Surg Hand Surg. 2010; 44:54–58.

5. Hofmeister EP, Mazurek MT, Shin AY, Bishop AT. Extension block pinning for large mallet fractures. J Hand Surg Am. 2003; 28:453–459.

7. Ishiguro T, Itoh Y, Yabe Y, Hashizume N. Extension block with kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg. 1997; 1:95–102.

8. Theivendran K, Mahon A, Rajaratnam V. A novel hook plate fixation technique for the treatment of mallet fractures. Ann Plast Surg. 2007; 58:112–115.

9. Lucchina S, Badia A, Dornean V, Fusetti C. Unstable mallet fractures: a comparison between three different techniques in a multicenter study. Chin J Traumatol. 2010; 13:195–200.
10. Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: part II, kinematic study. J Hand Surg Am. 2004; 29:903–908.

11. Hahn SB, Park KH, Choi YR, Kang HJ, Lee JK. Prognostic factors of the extension block technique for the bony mallet finger. J Korean Orthop Assoc. 2010; 45:127–132.

12. Crawford GP. The molded polythene splint for mallet finger deformities. J Hand Surg Am. 1984; 9:231–237.

14. Husain SN, Dietz JF, Kalainov DM, Lautenschlager EP. A biomechanical study of distal interphalangeal joint subluxation after mallet fracture injury. J Hand Surg Am. 2008; 33:26–30.

15. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010; 35:580–588.

17. Kim JY, Lee SH. Factors related to distal interphalangeal joint extension loss after extension block pinning of mallet finger fractures. J Hand Surg Am. 2016; 41:414–419.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download