Abstract
Purpose
The purpose of this study was to describe the long-term effects of stenting in patients with hepatic venous outflow obstruction (HVOO), who underwent living donor liver transplantation (LDLT).
Methods
Between January 2000 and December 2009, 622 adult patients underwent LDLT at our hospital, and of these patients, 21 (3.3%) were diagnosed with HVOO; among these patients, 17 underwent stenting. The patients were divided into early or late groups according to the time of their HVOO diagnoses (cutoff: 60 days after liver transplantation).
Results
The median follow-up period was 54.2 months (range, 0.5–192.4 months). Stent insertion was successful in 8 of 10 patients in the early group and 6 of 7 in the late group. The 5-year primary patency rates were 46% and 20%, respectively. In both groups, patients with recurrent HVOO at the beginning showed kinking confirmed by venography. Patients who carried their stents for more than 3 years maintained long-term patency. There was no significant difference in spleen size between groups; however, when the groups were compared according to whether they maintained patency, spleens tended to be smaller in the patency-maintained group.
Liver transplantation is now routinely performed to treat patients with end-stage liver disease, hepatocellular carcinoma, and fulminant hepatic failure [123]. The survival rate of patients undergoing liver transplantation is increasing due to the development of immunosuppressive agents, postoperative care, and endoscopy and angiography techniques [45].
After transplantation, many complications can occur such as rejection, vascular complications, primary nonfunction, biliary stricture or leakage, and infection, and improper treatment of these conditions can lead to liver failure [67]. Vascular complications in particular are life-threatening. Hepatic venous outflow obstruction (HVOO) is one of the most dangerous of these, inducing abnormal liver function tests (LFTs), splenomegaly, intestinal congestion, and renal dysfunction, eventually causing refractory graft dysfunction and mortality [78]. The incidence of hepatic vein outflow abnormalities is approximately 5%–13% after liver transplantation [910].
Primary stent placement is a safe and feasible procedure to treat HVOO; there are a few studies with good long-term results following primary stent placement. For example, Chu et al. [11] reported that the technical success rate was 100% and the 5-year primary patency was 93.8%; the intervals between transplantation and stent placement were 0–1,380 days (median, 59 ± 346.6 days). Previous studies were conducted without regard to the timing of HVOO, and therefore, currently no long-term studies based on the time of stent insertion are available. Indeed, the outcomes of early and late hepatic vein stenosis can differ according to the time of HVOO onset. Postoperative HVOO is viewed as secondary to technical factors such as tight suture line, donor-recipient size discrepancy, and kinking of a hepatic vein [1213]. In contrast, late HVOO is attributed to fibrosis around the anastomotic site, intimal hyperplasia, or compression of the anastomosis site from a hypertrophic graft [13].
In this study, the first study of its kind in adult living donor liver transplantation (LDLT) recipients, we retrospectively analyzed the long-term patency of stent insertion according to the time of HVOO onset.
The study complied with the Declaration of Helsinki and was approved by the Institutional Review Board of Samsung Medical Center (2017-07-023).
Between January 2000 and December 2009, 622 adults underwent LDLT at our hospital, including 21 (3.3%) diagnosed with HVOO. Of these patients, 3 were treated with only percutaneous transluminal balloon angioplasty and were excluded from this study. In the remaining 18 patients, HVOO was managed by stenting. These patients were divided into 2 groups based on the time of HVOO diagnosis: The early group consisted of 10 patients with HVOO diagnosed less than 60 days after LDLT, and the late group comprising 7 patients diagnosed with HVOO more than 60 days post-LDLT (Fig. 1). One patient was excluded because of stent migration to the atrium. Two patients manifested thrombosis caused by decreased blood flow due to stenosis. Both patients underwent stent insertion. Patients who had thrombosis without stenosis or kinking were excluded from the study, because there are other treatments such as thrombectomy or thrombolysis. Patient characteristics are shown in Table 1.
In the left lobe, an opening was created between the donor's middle hepatic (MHV) and left hepatic veins, and anastomosis was performed by Prolene 4-0 running suture of the recipient MHV stump. In the right lobe, the right hepatic vein (RHV) cuff was anastomosed end-side to the inferior vena cava (IVC) opening using a Prolene 4-0 running suture. At this time, the opening was made without differences in size or kinking. The V5/8 of the right lobe was reconstructed using a cryopreserved vessel if necessary (5/8 lobe larger). Intraoperative Doppler was performed after the anastomosis , without abnormal hepatic vein outflow.
We suspected HVOO in patients with ascites, pleural effusion, elevated liver enzymes, or abnormal results during postoperative Doppler ultrasound (US). Specifically, a monophasic waveform in the hepatic vein on Doppler US indicates obstructed outflow. CT was performed when the Doppler US resulted in abnormal findings. When the CT scan showed nonopacified hepatic veins or focal luminal narrowing, venography was performed for a final diagnosis. A blocked outflow was confirmed using venography and pressure measurement in the hepatic vein, the IVC, and the atrium. An outflow block was defined as IVC or hepatic vein with a pressure gradient of 5 mmHg or higher or kinking in the hepatic vein and IVC at the anastomotic site.
Spleen size was also measured when Duplex US was performed. Splenomegaly was defined as 13 cm or more. According to the liver transplant protocol, the next day after stenting, in the absence of any abnormalities with ultrasound or laboratory findings in the follow-up examination, in case of HCC patients, Doppler and liver CT were performed alternately every 3 months after liver transplantation during the first year and every 6 months after first year. Patients who were not diagnosed with HCC underwent Doppler 6 months after liver transplantation and liver CT at 1 year, followed by alternate Doppler and liver CT every other year. We measured spleen in liver CT.
Stenting was performed in 17 patients. Under local anesthesia, the right jugular vein was punctured with a micropuncture, the sheath was inserted to position the tip in the right atrium, and the right hepatic vein was selected via catheter insertion.
Pressure at the right atrium and right hepatic vein was measured to calculate the pressure gradient. Balloon dilatation was performed when the pressure gradient was significant (5 mmHg or more). Stenting was carried out in the absence of any improvement after balloon dilatation. The stent profile was similar to that of the Easy WALLSTENT (Boston Scientific, Natick, MA, USA), the Smart Control nitinol stent, and the Palmaz Genesus peripheral stent (Cordis, Miami, FL, USA). After stenting, hepatic venography and pressure gradient were measured, and the success of the procedure was evaluated by comparing pre- and postprocedure pressure.
Intravenous heparin was used during the procedure alone. After the procedure, the patient was treated with aspirin 100 mg once a day for one to 2 years to prevent thrombotic events.
Stent patency rates and spleen size were evaluated by Doppler US and CT scan. After stenting, a follow-up Doppler US was generally performed the next day or later during the admission; a radiologist at our hospital conducted the Doppler US. Doppler US and CT scans were performed one to 3 months after discharge. Spleen size was measured using Doppler US.
Kinking of hepatic vein does not imply a simple narrowing. Kinking refers to the condition at the anastomotic site where inflow vein (RHV) does not enter vertically into the outflow vein (IVC) and is angled. Kinking may occur when the liver rotates around IVC during liver regeneration or when the thoracic cage is too deep and the direction of RHV is dorsal to ventral and the anastomosis is located in the superior IVC. In addition, after anastomosis with the diaphragm was inflated due to pleural effusion, removing the pleural effusion after surgery may return the diaphragm to its original position and lead to mobilization of liver, resulting in kinking.
In this study, we designed 2 groups depending on their diagnosis of HVOO: either early (within 60 days of liver transplantation) or late (more than 60 days after). We selected this cut-off because Haga et al. [14] reported that the recipient's liver volume increases rapidly until 2 months, exceeding the standard liver volume, followed by an eventual decline to 90% of the standard. Transplanted liver rapidly increases in volume after liver transplantation compared with normal hepatectomy or donor remnant liver. The transplanted liver showed a volume increase of 90% up to 3 months and a rapid increase up to 2 months after transplantation, and a slow rate of increase thereafter. We defined 60 days as the time of the greatest effect of vein compression or kinking due to liver regeneration or mobilization.
We defined successful stenting by a postpressure gradient less than 5 mmHg and defined stent patency as a biphasic or triphasic waveform on a follow-up Doppler US or enhanced stent lumen without HVOO on a follow-up CT scan. We defined primary patency of the stent as the period from the initial stenting until the final patency was detected on Doppler US examination, CT, or hepatic venography.
We compared variations in pressure gradient between prestenting and poststenting using the Wilcoxon rank sum test, and used the Kaplan-Meier method to analyze the patency rate. We compared the rates using the log-rank test, considering a P-value of less than 0.05 as statistically significant. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
Stent insertion was successful in 8 of 10 patients (80%) in the early group and 6 of 7 (85.7%) in the late group. In the early group, the prestenting and poststenting pressure gradients across stenosis lesions were 15.46 ± 8.95 mmHg (range, 6–35 mmHg) and 2.64 ± 3.11 mmHg (range, 0–9 mmHg), respectively (P = 0.005). In the late group, the gradients across lesions were 8.14 ± 3.80 mmHg (range, 2–14 mmHg) and 2.14 ± 2.85 mmHg (range, 0–8 mmHg, P = 0.017) (Fig. 2). In particular, the pressure gradient before stenting was significantly higher in the early group compared with the late group (P = 0.03). Among the 18 patients who underwent stenting, only one had a procedural complication: the stent migrated to the atrium after deployment. After fixation with a balloon, the stent was removed via right internal jugular vein, despite massive bleeding. Surgical repair was performed due to persistent bleeding even after compression. A 2-cm laceration was found in the right internal jugular vein in the surgical field, and Prolene 6-0 running suture was performed. In this patient, HVOO was confirmed by monophasic waveform on Doppler and luminal narrowing on CT angiography, and stenting was performed. The patient did not undergo stenting subsequently because Doppler waveform changed from monophasic to triphasic without any treatment.
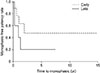
Fig. 3 shows the primary patency rates for stenting in patients with HVOO after LDLT; the median follow-up period was 54.2 months (range, 0.5–192.4 months). In the early group, the comprehensive 1-, 3-, and 5-year primary patency rates were 76%, 46%, and 46%, respectively. In the late group, the overall 1-, 3-, and 5-year rates were 40%, 20%, and 20%, respectively. The follow-up Doppler US showed that 4 patients in the early group failed to maintain triphasic waveforms. However, kinking was confirmed in all patients with kinking prior to stenting using venography, and 3 of those patients underwent second transplants.
Follow-up Doppler US of three patients in the late group did not maintain a triphasic waveform: 2 patients showed stenosis, and 1 patient had kinking. The 1 patient who had kinking underwent a second transplant.
To examine the long-term outcomes other than primary patency, we examined the changes in spleen size before and after stenting. We divided the patients into groups based on the shape of their US waveforms after stent insertion—tri/biphasic or monophasic—and the results are shown in Fig. 4. After stenting, the tri/biphasic group showed significantly smaller spleens than the monophasic group (P = 0.02). Between pre- and poststenting, the spleen size tended to decrease in the tri/biphasic group but increase in the monophasic group; however, there were no changes in the pre-/postinsertion spleen size of the early or late groups because of the low patency rates (Fig. 5). When we compared spleen sizes between patients with triphasic and monophasic waveforms, we confirmed that spleens were smaller in the triphasic group.
This study evaluated only HVOO in LDLT. Unlike hepatic vein anastomosis of LDLT, we performed hepatic vein anastomosis as a piggyback technique during DDLT. There were 133 cases of DDLT in the same period, whereas only a single case of HVOO was detected and excluded from the analysis.
The incidence of HVOO was lower than in other studies. The most important factor was the skilled surgeon who performed all hepatic vein anastomoses. In an anastomosis of hepatic vein, the lesion is determined in IVC to prevent kinking based on the final position of liver.
HVOO is a serious complication which may involve failure of transplanted liver, although many studies have demonstrated the effectiveness of stenting in treating HVOO. For example, Chu et al. [11] reported 1-, 3-, and 5-year stent primary patency rates of 93.8%, and Ko et al. [9] reported that 5-year primary patency was 72.4%. However, in this study, the effectiveness of stent insertion and patency maintenance was lower than in these studies (40% in the early group and 20% in the late group). The reason for the lower efficacy and patency compared with previous studies may be related to detection of kinking during venography findings. After stenting in the early group, all the patients who failed to maintain a triphasic waveform and adopted a monophasic waveform showed kinking (4/4); in contrast, kinking was observed in 1 of 3 patients (33%) in the late group. We found that kinking occurred more frequently in the early group. The development of HVOO due to kinking in the early period was fatal because despite successful stenting obstruction recurred; eventually, second transplant were performed. If kinking occurred in the form of hepatic vein hanging on the IVC, kinking may reccur due to liver weight despite stenting. Therefore, after venography confirms stenosis or kinking, HVOO should be treated, and kinking minimized during hepatic venous anastomosis.
We found variation in preangiographic pressure gradients between the early and late groups (Fig. 2). Darcy [15] reported that acute stenosis can develop due to technical problems or occur after the transplant due to intimal hyperplasia or perianastomotic fibrosis. In this study, in the early group, the pressure gradient was increased due to obstruction in abrupt outflow after the operations. In the late group, progressive stenosis due to intimal hyperplasia occurred, leading to lower pressure gradients. In this study, if we considered only stenosis, all the patients maintained patency, as in other studies. All three patients in the early group in this study showing stenosis maintained patency, whereas in the late group with stenosis, the findings varied. The preintervention pressure gradient in the late group was lower than in the early group, and the differences in pressure gradient between pre- and poststent insertion were higher in the early group. Only 2 of 5 patients with stenosis maintained a triphasic waveform, which suggests a high rate of kinking and lower patency maintenance than in other studies.
Liver transplant patients are exposed to many risks after transplantation: infection, rejection, drug side effects, and anatomical complications associated with artery, portal vein, duct, etc. These adverse effects may be detected together during the follow-up period. Therefore, even with hepatic vein complication, other problems can occur together, and patients in the late group are more likely to manifest a combination of other challenges than the early group patients. Patients in the late group progress to HVOO progressively and even if HVOO is diagnosed, it is likely that liver cirrhosis may have already occurred due to progressive liver injury. In late group, stent insertion may not be effective. In the early group, the abrupt HVOO was more likely to fall into liver failure due to liver congestion before the liver functioned fully. In the late group, the patient's condition is maintained by supportive care for symptoms caused by progressive obstruction rather than hepatic failure as a result of HVOO. Therefore, treatment of ascites is mainly indicated in the late group. Ascites causes spontaneous bacterial peritonitis, resulting in sepsis, or vomiting due to abdominal distension or ileus, resulting in asphyxia and aspiration pneumonia.
Symptoms of HVOO include ascites and abnormalities in LFTs, which tend to normalize in the short term following HVOO resolution [16]. However, the exact ascites volume cannot be measured, making it a subjective indicator. Nevertheless, the spleen size can be measured objectively and assessed for long-term relief of HVOO. Chezmar et al. [17] reported that the spleen remains significantly enlarged despite a 94% decrease in splenic volume after liver transplantation. Chikamori et al. [18] reported that the rate of reversal of spleen volume by liver transplantation was on average 12.0% ± 35.8%. Therefore, spleen size is a useful indicator of patency. In the group that maintained tri/biphasic waveforms on follow-up, the spleen size tended to decrease, whereas those manifesting a monophasic waveform tended to show increased spleen size. HVOO recurrence was confirmed in patients with increased spleen size. Therefore, spleen size needs to be continuously monitored via Doppler US even if patency is maintained.
This study was limited by the retrospective design and the small sample size. In addition, the progress of liver transplantation was influenced by various complications such as infection, rejection, and duct problems, which may occur together during long-term follow-up. Therefore, the patency rate cannot be determined accurately with HVOO alone, especially in the late group.
In conclusion, stenting is more effective for treating early stenosis than for early kinking or late stenosis with acceptable long-term patency.
Figures and Tables
References
1. Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010; 252:652–661.
2. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018; 68:723–750.

3. Kim JM, Lee KW, Song GW, Jung BH, Lee HW, Yi NJ, et al. Outcomes for patients with HCV after liver transplantation in Korea: a multicenter study. Ann Surg Treat Res. 2016; 90:36–42.

4. Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K, et al. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000; 232:490–500.

5. Adam R, Karam V, Delvart V, O'Grady J, Mirza D, Klempnauer J, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012; 57:675–688.

6. Hampe T, Dogan A, Encke J, Mehrabi A, Schemmer P, Schmidt J, et al. Biliary complications after liver transplantation. Clin Transplant. 2006; 20:Suppl 17. 93–96.

8. Piardi T, Lhuaire M, Bruno O, Memeo R, Pessaux P, Kianmanesh R, et al. Vascular complications following liver transplantation: a literature review of advances in 2015. World J Hepatol. 2016; 8:36–57.

9. Ko GY, Sung KB, Yoon HK, Kim KR, Kim JH, Gwon DI, et al. Early posttransplant hepatic venous outflow obstruction: long-term efficacy of primary stent placement. Liver Transpl. 2008; 14:1505–1511.

10. Umehara M, Narumi S, Sugai M, Toyoki Y, Ishido K, Kudo D, et al. Hepatic venous outflow obstruction in living donor liver transplantation: balloon angioplasty or stent placement? Transplant Proc. 2012; 44:769–771.

11. Chu HH, Yi NJ, Kim HC, Lee KW, Suh KS, Jae HJ, et al. Longterm outcomes of stent placement for hepatic venous outflow obstruction in adult liver transplantation recipients. Liver Transpl. 2016; 22:1554–1561.

12. Chen YS, Chen CL, Liu PP, Wang CC, Chiang YC, Huang TL, et al. Successful treatment of hepatic vein thrombosis following reduced-size liver transplantation. Transplant Proc. 1998; 30:3203–3204.

13. Someda H, Moriyasu F, Fujimoto M, Hamato N, Nabeshima M, Nishikawa K, et al. Vascular complications in living related liver transplantation detected with intraoperative and postoperative Doppler US. J Hepatol. 1995; 22:623–632.

14. Haga J, Shimazu M, Wakabayashi G, Tanabe M, Kawachi S, Fuchimoto Y, et al. Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transpl. 2008; 14:1718–1724.

15. Darcy MD. Mnagement of venous outflow complications after liver transplantation. Tech Vasc Interv Radiol. 2007; 10:240–245.
16. Cirera I, Navasa M, Rimola A, García-Pagán JC, Grande L, Garcia-Valdecasas JC, et al. Ascites after liver transplantation. Liver Transpl. 2000; 6:157–162.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download