Abstract
Spiradenomas are benign tumors that originate in the sweat glands. In this case, a 36-year-old Asian woman with no significant medical past history presented with history of tingling and numbness of little finger in the ulnar nerve sensory territory. There is positive Tinel's sign at her ulnar side of hand. At first, neurilemmoma was suspected based on findings of clinical examination. Under local anesthesia, excisional biopsy was performed. Histopathologic study demonstrated the typical histopathologic findings of spiradenoma. In this case, Author misdiagnosed as neurilemmoma due to its neurologic symptom rather than typical spiradenoma's characteristics such as neurologic symptom. Since there is a possibility that it may be different from the first impression, it is imperative to carry out sufficient inspection before surgery to avoid misdiagnosis. Proper diagnosis of eccrine spiradenoma is important because of the occurrence of potentially life-threatening malignant transformation.
Eccrine spiradenoma is exceedingly rare, accounting for roughly 1 of 13,000 specimens submitted to a dermatopathologist, especially at hand1. It most commonly arises in people aged 15 to 35 years, and the front of the trunk and proximal limbs are the most common sites. Proper diagnosis of eccrine spiradenoma is important because of the occurrence of potentially life-threatening malignant transformation. From literature review, there is few case of spiradenoma on hand2. Author present a case of solitary spiradenoma on subcutaneous layer mimicking neurilemmoma.
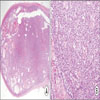
A 36-year-old Asian woman with no significant medical past history presented with history of tingling and numbness of little finger in the ulnar nerve sensory territory of the right hand without tenderness, since the past ten years. Physical examination of the right hand showed about 15 mm size oval shape well-defined soft tissue mass situated on subcutaneous fat. There is positive Tinel's sign at her ulnar side of hand. A neurilemmoma was suspected on the basis of findings at clinical examination. Under local anesthesia, excisional biopsy was performed (Fig. 1). The incision line was designed along the long axis of mass for easy approach. Grossly, Specimen was 15 mm size pinkish color oval shape mass with firm encapsulated characteristics (Fig. 2). Histopathologic examination demonstrated well-demarcated tumor with capsulation and cystic change. The tumor cells consisted of small basaloid cells, paler cells, and lymphocytes, arranged with a ribbon and reticular pattern (Fig. 3). The histopathologic findings of the skin were consistent with spiradenoma. The patient recovered uneventfully from the surgery. There is no evidence of recurrence and metastasis.
Eccrine sweat glands are simple tubular glands that open directly to the skin and are present in all body areas, with their highest concentration in the palms, soles, and axillae. The etiology of eccrine spiradenoma is not fully understood. It is often misdignosed with neuromas, leiomyomas, neurofibroma, hidradenocarcinoma of the sweat glands, glomus tumors, lipoma, angiolipoma, dermatofibroma, hemangioma, and angioleiomyoma3. Computed tomography and magnetic resonance imaging can help the diagnosis of this kind of tumor, especially for tumors in the deep dermis or subcutaneous tissues. However, the definitive diagnosis requires skin biopsy. Low incidence of this tumor may lead to a delay in diagnosis and treatment4.
Clinically, it presents as numerous nodules and also can present as a painful, slow-growing, solitary nodule that approximately one third of eccrine spiradenoma occur in the head and neck, one third on the trunk, and one fifth on the extremities. Random multiple tumors have been reported to occur on the chest, upper extremities, forehead, and scalp5. Noto et al.6 reported linear spiradenoma arising in medial canthus and cheek. Gupta et al.7 reported a 23-year-old woman with linear facial spiradenoma and coexistent eyelid spiradenoma. Pain or tenderness are not always suggested as a clinical characteristic. Several study showed non tender eccrine spiradenoma2,3. The generation of pain is thought to be related to small unmyelinated axons permeating the hyalinized stromal mantle. Some researchers believe that the expansion of cysts in the tumor also gives rise to pain8. Although the pain of an eccrine spiradenoma is ‘the most frequent and striking symptom’, the mechanism of pain generation has not been elucidated entirely. In 1996, Criton and Aravindan9 stated that pain might be due to the contraction of myoepithelial cells. However, electron microscopy has not proven the presence of myoepithelial cells in the tumor.
Histopathologically, eccrine spiradenoma presents as intradermal lobules surrounded by a fibrous capsule without connections to the epidermis. On higher magnification view, the epithelial cells within the tumor lobule are arranged in intertwining cords. The epithelial cells within the tumor lobule are arranged in intertwining cords with two types of epithelial cells. There have been some reports of malignant transformation of spiradenoma6.
Complete surgical excision with longitudinal incision is the first choice of treatment for tumor clearance. The lesion does not usually recur after excision. Surgery is unnecessary if the lesions are not disfiguring, increasing in size and number, or painful. There are no clear recommendations for margins for standard excision. Radiation, chemotherapy, and hyperthermic limb perfusion chemotherapy have been carried out in malignant spiradenomas10.
In conclusion, author misdiagnosed as neurilemmoma due to its neurologic symptom rather than typical spiradenoma's characteristics like pain symptoms. The use of transverse incisions parallel to the long axis of the mass other than longitudinal incision should be avoided. Failure to identify its morphologic features may lead to a mistaken diagnosis. Considering the anatomic location and clinical history, differential diagnoses and preoperative magnetic resonance imaging (MRI) should be performed. Because of possibility of malignant change, close local surveillance (MRI plus contrast) is essential.
Figures and Tables
 | Fig. 1(A) About 15 mm size ovoid shape well-defined firm soft tissue mass situated on subcutaneous fat, which is ulnar side of hand. (B) Under local anesthesia, excisional biopsy was performed. The incision line was designed along the long axis of mass for easy approach. Well encapsulated mass was excised. There is no involvement of neurovasular bundle. (C) Primary repair was performed using Nylon. |
References
1. Padmini HR, Dinesh P. A rare and unique case of eccrine spiradenoma of the eyelid. J Evolution Med Dental Sci. 2013; 2:1700–1703.
2. Al-Qattan MM. Eccrine spiradenoma of the hand clinically mimicking a lipoma. J Hand Surg. 1996; 21:551–552.

3. Alfonso-Trujillo I, Arteaga-Hernández E, Pérez-Suárez JC. Eccrine Spiradenoma in a zosteriform distribution: presentation of a case. Actas Dermosifiliogr. 2009; 100:619–620. Spanish.

4. Siegel HJ, Said-Al-Naief N, Long J, Lopez-Ben RR, Klein M. Giant eccrine spiradenoma of the hand. Am J Orthop. 2008; 37:E141–E143.
5. Mambo NC. Eccrine spiradenoma: clinical and pathologic study of 49 tumours. J Cutan Pathol. 1983; 10:312–320.
6. Noto G, Bongiorno MR, Pravià G, Aricò M. Multiple nevoid spiradenomas. Am J Dermatopathol. 1994; 16:280–284.

7. Gupta S, Radotra BD, Kaur I, Handa S, Kumar B. Multiple linear eccrine spiradenomas with eyelid involvement. J Eur Acad Dermatol Venereol. 2001; 15:163–166.

8. Amoroso C, Grandi E, Carinci F. Eccrine spiradenoma of the ear: case report. Int J Oral Maxillofac Surg. 2003; 32:662–663.

9. Criton S, Aravindan KP. Zosteriform network of spiradenoma. Indian J Dermatol Venereol Leprol. 1996; 62:185–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download