Abstract
Purpose
Favorable results have been reported after the direct repair of chronic ulnar collateral ligament ruptures of the thumb metacarpophalangeal (MP) joint, but the results for radial ligament seem rather controversial. The purpose of this study is to compare the results of ligament reattachment between chronic rupture of the ulnar and the radial collateral ligament (RCL) of the joint.
Methods
We reviewed retrospectively the radiologic and clinical results of ligament reattachment with suture anchors for chronic (more than 6 weeks) rupture of the collateral ligament of the thumb MP joint with averaged 22-month follow-up. The data between 6 radial and 8 ulnar ligament repairs were compared statistically.
Results
The average of postoperative ulnar deviation angle was 13.3° in radial ligament and 2.0° in ulnar ligament (p=0.020) in the last follow-up plain X-ray. Postoperative ligament instability was positive in 4 out of the 6 radial repairs and no case with instability was observed in ulnar ligament. In postoperative follow-up, sustained joint subluxation was observed only in 2 out of the 6 radial repairs.
For chronic collateral ligament injuries of the metacarpophalangeal (MP) joint of the thumb, ligament reconstruction has been usually recommended1234. Delayed direct suture techniques are not considered effective due to scar tissue formation and degeneration of the ligament ends567891011. The primary repair of chronic collateral ligament injuries to fingers other than the thumb have also been reported suboptimal11.
However, some studies have reported the favorable results after the direct repair or reattachment of chronic ulnar collateral ligament (UCL) ruptures of the thumb MP joint791012. On the contrary, there have been few studies reporting the results of a direct repair for chronic radial collateral ligament (RCL) ruptures and its outcomes seem rather controversial16131415. McDermott and Levin6 reported 5 cases with excellent clinical and subjective results after the repair of chronic RCL ruptures with a suture anchor. Coyle15 also reported successful results using RCL soft tissue advancement and bony reattachment for the late repair of chronic RCL ruptures. However, Camp et al.13 reported unfavourable results of chronic RCL injuries treated with RCL repair and abductor pollicis brevis advancement. Durham et al.14 reported good results in acute RCL ruptures treated with direct repair and chronic RCL injuries treated with a soft tissue repair or reconstruction, but late repair or reconstruction could lead to some loss of joint motion and joint pain. Catalano et al.1 recommended repair of acute RCL injuries and reconstruction of chronic RCL injury after a review of the postoperative results of 26 patients.
The anatomy of the radial side of the thumb MP joint is different from that of the ulnar side8. Musculotendinous insertions of the flexor pollicis brevis and abductor pollicis brevis are weaker and insert more dorsally than that of adductor pollicis. After RCL ruptures, the joint lose radial ligamentous and dorsal capsular support and the dorsally located radial aponeurosis cannot compensate for a volarly and ulnarly deforming force by adductor pollicis. Thus, RCL ruptures leads to volar subluxation and ulnar translation of the proximal phalanx, which may lead to degenerative change of the joint8. In contrast, intrinsic imbalance and joint subluxation is minimal in UCL injuries.
We tried to reattach the ligament with suture anchors if the midsubstance of the ligament was observed to be relatively intact during operation. The purpose of this study was to compare the results of a ligament reattachment with suture anchors for chronic radial and UCL injuries of the thumb MP joint.
We reviewed retrospectively the medical records of patients who underwent the ligament reattachment in the thumb MP joint from June 2007 to September 2014. Inclusion criteria were the thumb with collateral ligament ruptures with grade III instability presenting 6 weeks after the initial trauma, or those who fail more than 6 weeks of conservative immobilization. The joints with osteoarthritis, inflammatory arthritis, any previous history of surgery, or simultaneous both ligament ruptures were excluded. This study was approved by the institutional review board. Fourteen thumbs (9 right, 5 left) in 14 patients (7 males and 7 females) were included in our study. The mean age was 34 years (range, 15–66 years), and the mean injury to operation interval was 313 weeks (range, 6 weeks–5 years). The average follow-up was 22 months (range, 12–61 months). These injuries were most frequently caused by a direct strike or by a fall onto an outstretched hand.
The following information was collected: age, time interval from injury to operation, range of motion (ROM), verbal pain score, grip strength, pinch strength, and the Disabilities of the Arm, Shoulder, and Hand (DASH) scores. Ligament instability was tested and graded as ‘none’, ‘equivocal (larger valgus or varus deviation than the contralateral side with a hard end in manual stress testing)’, or ‘definite (larger deviation with a soft end)’.
There were 6 RCL and 8 UCL repairs. As there was no definite discontinuity in the ligament in all cases, the site with the findings implicative of a chronic ligament rupture was considered the rupture site. The findings were as follows: (1) the focal site of the ligament became thinner, (2) the focal whitish substance became semi-transparent, or (3) the length of the focal site was changed with abduction or adduction of the joint. If the midsubstance was observed to maintain the sufficient thickness and length of the ligament, the scar tissue was removed as little as possible and the ligament was reattached with Mitek® (DePuy Synthes, Raynham, Massachusetts, USA) or SutureTak® (Arthrex, Naples, Florida, USA) suture anchors (Fig. 1). After insertion of the suture anchor, the joint was reduced to a neutral position and was fixated with a Kirschner wire (K-wire) before the ligament was sutured. The K-wires and a thumb spica cast were removed 6 weeks after surgery and active motion exercise was started. Active assisted motion exercise was begun at 9–10 weeks and passive exercise was allowed 3 months after surgery.
Preoperative deviation (ulnar deviation in RCL and radial deviation in UCL) angles of the MP joint were evaluated on anteroposterior X-rays with and without stress testing and postoperative deviation angle were measured on X-ray without stress testing. Subluxation of the MP joint was considered to be positive on the lateral X-ray if the longitudinal axis line crossing the center of the proximal phalangeal base was located volar to the center of the metacarpal head, or if the dorsoradial prominence of the metacarpal head existed in thumb extension (Fig. 2).
The data between RCL (group A) and UCL (group B) repairs and between the injured and the contralateral side were compared statistically with Mann-Whitney test, chi square test, Wilcoxon signed rank test, and Spearman's correlation test and the cut-off value of statistical significance was p<0.05.
A proximal repair was most common in group A (4 out of 6) and a distal repair was most common in group B (7 out of 8), of which the distribution was significantly different (p=0.036).
The average of time interval from injury to operation of group A (86 weeks) was larger than that of group B (14 weeks). Between the 2 groups, there was no significant difference (p>0.05) in average age, postoperative flexion contracture, further flexion, ROM of the MP joint, verbal pain scores, postoperative grip strength ratio (grip strength in the injured side/grip strength in the contralateral side), pinch strength ratio, and DASH scores (Table 1).
The averages of preoperative and postoperative ulnar deviation angles in group A were larger than those in group B in plain anteroposterior X-ray (Table 2). After removal of an inserted K-wire at 6 weeks, slow progression of the deviation had been observed as the time progressed in some cases. The average of preoperative deviation angles of the injured side was significantly larger than that of the contralateral side in group A (p=0.028), but the averages in group B were not significantly different in plain X-ray (Table 3). The averages of postoperative deviation angles of the injured side were not significantly different from those of the contralateral side in group A and group B. In stress X-rays, the average of preoperative ulnar deviation angles of the injured side was significantly larger than that of the contralateral side in group A (p=0.043) and the average of preoperative radial deviation angles of the injured side was significantly larger than that of the contralateral side in group B (p=0.018). Preoperative and postoperative deviation angle in plain X-ray were not significantly correlated (p=0.198), but the preoperative deviation angles in stress X-ray were correlated with the postoperative deviation angles (p=0.002).
In the last follow-up, postoperative ‘definite’ ligament instability was positive in 4 out of the 6 in group A, and no case with ligament instability was observed in group B. The distribution of ligament instability was significantly different between the 2 groups (p=0.006). Joint subluxation was observed preoperatively in 3 out of 6 in group A and subluxation was sustained postoperatively in 2 out of 3, and no case with joint subluxation was observed in group B. The distribution of preoperative joint subluxation was significantly different between the 2 groups (p=0.024), but postoperative subluxation was not significantly different between the 2 groups (p=0.078). Postoperative joint subluxation was observed in 2 out of 4 with postoperative instability, and subluxation and instability was significantly correlated (odds ratio=5.938, p=0.016). The average preoperative deviation angle was significantly different between cases with and without instability (p=0.004), and so was that of the postoperative angles (p=0.002).
The time interval from injury to operation was not correlated with postoperative ROM of the joint, grip or pinch strength ratio, DASH scores, preoperative deviation angle with or without stress, or postoperative deviation angle (p>0.05). Postoperative ROM of the MP joint was not correlated with the preoperative deviation angle without stress, or the postoperative deviation angle (p>0.05). Postoperative further flexion was positively correlated with the deviation angle difference between the injured and the contralateral side with stress testing (r=0.613, p=0.034).
The flexion angle of the MP joint with postoperative K-wire fixation was not correlated with the postoperative ROM (p=0.538) and the deviation angle with postoperative K-wire fixation was not correlated with the postoperative deviation angle in the last follow-up (p=0.598).
There was 1 complication out of 19 ligament repairs. Osteolysis around a metal anchor in the radial condyle of the metacarpal head was observed and the metal was removed 3 years after surgery. Slight ulnar deviation of the joint in X-ray without stress testing was observed with clinical ligament instability.
Treating chronic ligament injuries of the MP joint with ligament reconstruction is more demanding and less anatomical than direct reattachment. If the midsubstance of the ligament was observed to be relatively intact during operation, we tried to reattach the ligament with suture anchors rather than performing a ligament reconstruction. In most of studies, UCL injuries have been best repaired within 3 weeks and after that period, ligament reconstruction is recommended516. Alternatively, operative treatment for RCL ruptures may occasionally be delayed by the understanding that there has been no significant difference in functional results between primary repair and reconstruction117. However, the results of our study was the opposite to the these general considerations. The results of RCL repairs were more unfavorable than those of UCL repairs with ligament reattachment with suture anchors in chronic collateral ligament ruptures of the thumb MP joint. The average of deviation angle of the RCL repairs was larger than that of UCL repairs in preoperative and postoperative plain X-rays. Postoperative ligament instability was only observed in 4 RCL cases and postoperative joint subluxation was observed only in the RCL repairs.
Though there was no statistical difference in clinical results of RCL and UCL repairs except for time interval from injury to operation in averaged 22 months of follow-up, ligament instability and joint subluxation would cause arthritic changes of the joint in the long term follow-up. Thus, the results of RCL repairs with instability or subluxation were considered more unfavorable than those of UCL repairs. Postoperative larger deviation without stress showed that the joint after RCL repair was not maintained in the reduced position and the proper alignment. These results may be the unopposed forces of the adductor pollicis muscle and the dynamic adduction force of the flexor pollicis longus tendon which make the joint prone to ulnar deviation and attenuating the RCL more than UCL. The larger averages of preoperative deviation angles of RCL ruptures in plain and stress X-ray might mean that the RCL group included more cases with injuries of higher degrees including additional injuries in the accessory collateral ligament, joint capsule, and the aponeurosis, but these injuries could not be evaluated intraoperatively due to the chronicity of the injuries.
Unfavorable results of RCL repairs might also be the due to the longer duration of time from injury to operation in RCL repairs (86 weeks) than UCL repairs (14 weeks). Patients with RCL ruptures do not occasionally experienced decreased function and presented to a hand surgeon later than UCL ruptures17. In terms of reattachment rather than reconstruction, longer duration of ligament ruptures before operation could influence the result of treatment.
Another reason of the unfavorable results of RCL repairs might be related to the difference in the rupture sites between RCL and UCL injuries. In RCL injuries, a midsubstance tear is more frequent than in UCL injuries17. Chronic midsubstance ruptures could not be identified intraoperatively and we selected the repair site either at the proximal or distal attachment. The results of more common RCL midsubstance tears might be less successful because the repair site did not coincide with the ruptured site and operation caused the ligament advancement or shortening.
We fixated the joint temporarily with a K-wire before the RCL suture was performed in order to maintain the joint reduction by opposing the deforming force of the adductor pollicis and the flexor pollcis longus. In some cases, the joint deviated ulnarly or subluxated volarly preoperatively. However, for the UCL repairs a K-wire was not inserted or was inserted after the UCL was sutured because there was no deviation or subluxation in most of the UCL ruptures. The angle of the MP joint with postoperative K-wire fixation was not correlated with the postoperative ROM or the postoperative deviation angle in the last follow-up.
This study has some limitations. It is a retrospective study in which some preoperative data were not obtained. The sample size was small, which made some statistical significance missed. The follow-up period was short to observe any clinical or radiologic changes of arthritis.
Figures and Tables
 | Fig. 1(A) Distal ulnar collateral ligament (UCL) ruptured site is thin and changed into a translucent granulation tissue (arrow). (B) Detachment site is well observed with over-pronation of the thumb. (C) UCL was reattached with an absorbable suture anchor and the joint capsule was repaired. |
 | Fig. 2(A) Preoperative X-ray of radial collateral ligament (RCL) rupture shows mild ulnar deviation and volar subluxation. (B) Retracted proximal RCL is thin and translucent. (C) Postoperative X-ray. (D) X-ray at 4 years postoperatively shows increased deformity of the joint and osteolysis around a metal anchor. |
Table 1
Demographic data between 2 groups
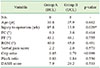
Verbal pain score: 0–10 (maximum pain), Grip ratio (postoperative grip strength ratio): grip strength in the injured side/grip strength in the contralateral side, Pinch ratio (postoperative pinch strength ratio): pinch strength in the injured side/pinch strength in the contralateral side.
RCL: radial collateral ligament, UCL: ulnar collateral ligament, FC: postoperative flexion contracture, FF: postoperative further flexion, ROM: postoperative range of motion, DASH score: Disabilities of the Arm, Shoulder, and Hand score.
*p<0.05.
ACKNOWLEDGEMENTS
This work was supported by a grant from Research Year of Inje University (20121019).
References
1. Catalano LW 3rd, Cardon L, Patenaude N, Barron OA, Glickel SZ. Results of surgical treatment of acute and chronic grade III [corrected] tears of the radial collateral ligament of the thumb metacarpophalangeal joint. J Hand Surg Am. 2006; 31:68–75.
2. Horch RE, Dragu A, Polykandriotis E, Kneser U. Radial collateral ligament repair of the thumb metacarpophalangeal joint using the abductor pollicis brevis tendon. Plast Reconstr Surg. 2006; 117:491–496.

3. Rhee PC, Jones DB, Kakar S. Management of thumb metacarpophalangeal ulnar collateral ligament injuries. J Bone Joint Surg Am. 2012; 94:2005–2012.

4. Samora JB, Harris JD, Griesser MJ, Ruff ME, Awan HM. Outcomes after injury to the thumb ulnar collateral ligament--a systematic review. Clin J Sport Med. 2013; 23:247–254.

5. Smith RJ. Post-traumatic instability of the metacarpophalangeal joint of the thumb. J Bone Joint Surg Am. 1977; 59:14–21.

6. McDermott TP, Levin LS. Suture anchor repair of chronic radial ligament injuries of the metacarpophalangeal joint of the thumb. J Hand Surg Br. 1998; 23:271–274.

7. Fairhurst M, Hansen L. Treatment of “Gamekeeper's Thumb” by reconstruction of the ulnar collateral ligament. J Hand Surg Br. 2002; 27:542–545.

8. Edelstein DM, Kardashian G, Lee SK. Radial collateral ligament injuries of the thumb. J Hand Surg Am. 2008; 33:760–770.

9. Pai S, Smit A, Birch A, Hayton M. Delayed anatomical repair of ruptured ulnar collateral ligament injuries of the thumb using a dissolvable polylactic acid bone anchor. J Trauma. 2008; 65:1502–1506.

10. Moharram AN. Repair of thumb metacarpophalangeal joint ulnar collateral ligament injuries with microanchors. Ann Plast Surg. 2013; 71:500–502.

11. Wong JC, Lutsky KF, Beredjiklian PK. Outcomes after repair of subacute-to-chronic grade III metacarpophalangeal joint collateral ligament injuries in fingers are suboptimal. Hand (N Y). 2014; 9:322–328.

12. Christensen T, Sarfani S, Shin AY, Kakar S. Long-term outcomes of primary repair of chronic thumb ulnar collateral ligament injuries. Hand (N Y). 2016; 11:303–309.

13. Camp RA, Weatherwax RJ, Miller EB. Chronic posttraumatic radial instability of the thumb metacarpophalangeal joint. J Hand Surg Am. 1980; 5:221–225.

14. Durham JW, Khuri S, Kim MH. Acute and late radial collateral ligament injuries of the thumb metacarpophalangeal joint. J Hand Surg Am. 1993; 18:232–237.

15. Coyle MP Jr. Grade III radial collateral ligament injuries of the thumb metacarpophalangeal joint: treatment by soft tissue advancement and bony reattachment. J Hand Surg Am. 2003; 28:14–20.

16. Melone CP Jr, Beldner S, Basuk RS. Thumb collateral ligament injuries. An anatomic basis for treatment. Hand Clin. 2000; 16:345–357.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download