INTRODUCTION
Allergy (also referred to as immunological hypersensitivity) is associated with a wide range of clinical manifestations [
12]. Respiratory allergy is a hypersensitivity reaction that is commonly mediated by IgE. Asthma and allergic rhinitis are respiratory allergic diseases that are referred to as united airway diseases (UADs) because they show some common characteristics [
34]. The World Health Organization has reported that approximately 300 million and 400 million patients worldwide have asthma and allergic rhinitis, respectively [
5]. A basic health research conducted in 2013 by the Indonesian Ministry of Health showed that the prevalence of asthma in Indonesia was 4.5%, with an increased prevalence of 5.2% in Jakarta [
6]. This high prevalence of asthma in Jakarta was associated with high mortality, morbidity, and treatment cost [
7].
Inhalant allergens worsen the clinical manifestations and daily symptoms of asthma and allergic rhinitis. In 1999, Baratawidjaja et al. [
8] reported that out of 107 patients with asthma and/or allergic rhinitis in Jakarta, 77.5% showed
Dermatophagoides pteronyssinus sensitization and 72.0% showed
Blomia tropicalis sensitization. In 2006, Sundaru [
9] reported that majority of patients with asthma showed house dust mite sensitization, with 77.3% patients showing
D. pteronyssinus sensitization and 69.6% patients showing
Dermatophagoides farinae sensitization. However, this study did not examine
Blomia tropicalis sensitization [
9]. The findings of these studies indicate that house dust mites are the major inhalant allergens in Jakarta, Indonesia. Moreover, Sundaru [
9] reported that although the prevalence of dog and cat dander sensitization was low in patients with asthma, these allergens were strongly associated with the clinical symptoms of asthma in these patients.
Allergen sensitization can be diagnosed by detecting serum-specific IgEs (SSIgEs) associated with that allergen [
2]. This can be performed
in vivo by using skin prick test (SPT) and
in vitro by performing SSIgE test [
2510]. SPT is the most accurate method and is considered to be the gold standard for diagnosing IgE-mediated allergen sensitization [
510]. However, SPT is associated with some limitations such as severe local skin reaction and anaphylactic risk. Moreover, results of this test are affected by some medications such as steroids and antihistamines [
1011]. SSIgEs can be detected
in vitro by performing enzyme-linked immunosorbent assay (ELISA) and immunoblotting analysis by using multicheck kits [
1213]. Commercial ELISA kits are available in Indonesia. However, conflicting results are available about the accuracy of this technique in different regions. Moreover, no study has assessed the accuracy of ELISA for diagnosing inhalant allergen sensitization in Indonesian patients with asthma and/or allergic rhinitis. Therefore, the present study assessed the accuracy of the SSIgE test with microfluidic array ELISA for diagnosing inhalant allergen sensitization in Indonesian patients with asthma and/or allergic rhinitis.
MATERIALS AND METHODS
Study subjects
This cross-sectional diagnostic study included patients with asthma and/or allergic rhinitis (age, 18–59 years) who visited the outpatient clinic of the Department of Allergic and Clinical Immunology of Cipto Mangunkusumo National Hospital in Jakarta, Indonesia, from October 2016 to January 2017. The Cipto Mangunkusumo National Hospital is among the top referral hospitals in Indonesia. Study subjects were selected by performing nonprobability sampling with a consecutive sampling method. Patients were included in the study if they were diagnosed with asthma and/or allergic rhinitis and were aged between 18 and 59 years. Patients receiving antihistamines or corticosteroids 7 days before performing the SPT and pregnant and lactating woman were excluded from this study.
Skin prick test
All the study patients underwent SPT by using standard allergens obtained from Stallergenes (Paris, France). SPT was performed on the forearm by using 6 common inhalant allergens, namely, D. pteronyssinus, D. farinae, B. tropicalis, dog dander, cat dander, and cockroach allergen. Histamine was used as a positive control, and diluent was used as a negative control. The selected allergens were dropped on a marked area on the forearm, and the area was pricked using Stallerpoint (Stallergenes). After 15 minutes, the area was wiped. Results were evaluated by measuring wheal and flare reaction for each allergen. A positive reaction was defined as the presence of a wheal and flare, with a wheal diameter of at least 3 mm, compared with that observed for the negative control.
SSIgE test with Agnitio BioIC kit
Patients who showed a positive skin reaction for at least one allergen underwent the SSIgE test on the same day. For this, 2-mL blood was collected from the peripheral vein of the patients, and SSIgEs were detected using BioIC commercial kit (Agnitio Science and Technology Inc., Hsinchu, Taiwan). The SSIgE test uses a microfluidic array system that allows high-density multitarget screening with minimal serum usage. The microfluidic array system is applied on a cartridge that serves as a medium for ELISA. A silicone rubber coated with an antigen protein-containing nitrocellulose membrane is placed in the center of the cartridge. In this region, the antigen protein present in the membrane binds to IgEs present in the serum. Antigen-antibody complexes formed were determined colorimetrically by using a substrate reagent and a CCD camera. Images obtained using the CCD camera were combined with a BioIC laboratory algorithm to produce Agnitio unit (AU) values that were converted into classes 0–6. Class scores of 0–6 were determined using AU values of <1, 1–2, 2–4, 4–8, 8–16, 16–32, and >32, respectively. An AU value of ≥1 indicated a positive reaction [
14].
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Demographic information, characteristics, and sensitization rate of the study patients were analyzed by performing descriptive statistical analysis. Sensitivity, specificity, predictive value, and likelihood ratio (LR) of the SSIgE test for each allergen were evaluated to determine the accuracy of this method for diagnosing allergen sensitization.
Ethical approval
This study was ethically approved by the Ethics Committee of the Faculty of Medicine, University of Indonesia (protocol number: 17-01-009). All the study patients provided informed consent before participating in the study. Moreover, all the study patients provided a detailed medical history and underwent a medical examination before participating in the study.
RESULTS
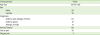
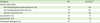
In the present study, 104 patients underwent SPT, of which 3 patients showed dermographism. Moreover, one of these 104 patients was aged more than 60 years at the time of SPT. Of the 104 patients, 100 underwent the SSIgE test. The median age of the patients was 39 years (range, 19–59 years), and approximately 78% patients were women. Majority of the patients (64%) had asthma as well as allergic rhinitis. The characteristics of the study patients are summarized in
Table 1.
Table 1
Characteristics of the study patients (n = 100)
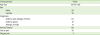
|
Characteristic |
Value |
|
Age (yr) |
39 (19–59) |
|
Sex |
|
|
Male |
24 |
|
Female |
76 |
|
Diagnosis |
|
|
Asthma and allergic rhinitis |
64 |
|
Asthma alone |
21 |
|
Allergic rhinitis |
15 |
|
Family history*
|
66 |
|
Cat as pet |
23 |
|
Dog as pet |
3 |

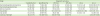
Results of the SPT indicated that approximately 72%–77% patients showed house dust mite sensitization, with the highest sensitization rate observed for
B. tropicalis. Results of the SSIgE test by using the Agnitio BioIC kit indicated that 38%–66% patients showed house dust mite sensitization, with the lowest sensitization rate observed for
B. tropicalis. The sensitization rates for cat and dog dander and cockroach allergen determined by performing the SSIgE test were lower than those determined by performing the SPT. These results are summarized in
Table 2.
Table 2
Sensitization rates for the inhalant allergens examined in the present study
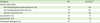
|
Allergens |
SPT |
BioIC kit*
|
|
House dust mites |
|
|
|
Dermatophagoides pteronyssinus (%) |
72 |
58 |
|
Dermatophagoides farinae (%) |
72 |
66 |
|
Blomia tropicalis (%) |
77 |
38 |
|
Cat dander (%) |
37 |
11 |
|
Dog dander (%) |
33 |
8 |
|
Cockroach allergen (%) |
41 |
5 |

The sensitivity of the SSIgE test using microfluidic array ELISA for diagnosing house dust mite sensitization was approximately 48%–77%, with the highest sensitivity observed for diagnosing
D. farinae sensitization. The specificity of the SSIgE test for diagnosing house dust mite sensitization was approximately 64%–95%. However, the SSIgE test showed low sensitivity and high specificity for diagnosing cat dander, dog dander, and cockroach allergen sensitization. These results are summarized in
Table 3.
Table 3
Diagnostic accuracy of the serum-specific immunoglobulin E (SSIgE) test with microfluidic array ELISA
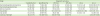
|
SSIgE |
Diagnostic accuracy |
|
Sensitivity (%) |
Specificity (%) |
PPV (%) |
NPV (%) |
LR (+) |
LR (−) |
|
Dermatophagoides pteronyssinus
|
70 (58–80) |
75 (54–88) |
87 (76–94) |
50 (34–65) |
2.8 (1.4–5.4) |
0.38 (0.26–0.57) |
|
Dermatophagoides farinae
|
77 (66–86) |
64 (44–80) |
84 (73–92) |
52 (35–69) |
2.1 (1.3–3.6) |
0.34 (0.2–0.5) |
|
Blomia tropicalis
|
48 (36–59) |
95 (76–99) |
97 (84–99) |
35 (24–48) |
11 (1.6–76) |
0.5 (0.4–0.7) |
|
Dog dander |
3 (1.5–17) |
89 (79–95) |
12.5 (0.65–53) |
65 (54–74) |
0.29 (0.03–2.26) |
1.08 (1.05–1.15) |
|
Cat dander |
10 (3.5–26) |
88 (77–95) |
36 (12–68) |
62 (51–72) |
0.9 (0.3–3.1) |
1 (0.89–1.12) |
|
Cockroach allergen |
12 (4.5–27) |
100 (92–100) |
100 (46–100) |
62 (51–71) |
- |
0.8 (0.78–0.98) |

DISCUSSION
Asthma and allergic rhinitis were diagnosed in 64% study patients. This finding confirmed the unity in structure and function between the upper and lower airways as a UAD. Allergic rhinitis increases the risk of allergic asthma, and more than 80% patients with asthma show symptoms of allergic rhinitis [
415]. Most patients with asthma and allergic rhinitis show sensitization to house dust mites followed by that to cockroach allergen, cat dander, and dog dander. Results of previous studies performed in Jakarta have also reported that most patients with asthma and allergic rhinitis show sensitization to house dust mites among other inhalant allergens [
89]. Therefore, education about preventing house dust mites must be given to all patients with asthma and allergic rhinitis. Cat and dog dander sensitization rates reported in the present study are higher than those reported in the 2006 study by Sundaru [
9], which reported cat and dog dander sensitization rates of approximately 6.76% and 3.68%, respectively. This difference may be because patients included in the present study resided in different regions of Jakarta compared with those included in the study by Sundaru who resided in a single region in central Jakarta.
The SSIgE test using microfluidic array ELISA had a sensitivity of 70%, specificity of 75%, and high positive predictive value (PPV) of 87% for diagnosing
D. pteronyssinus sensitization. Moreover, this test had an LR (+) value of 2.8 that increased posttest probability to 88%. Therefore, a positive result of the SSIgE test confirmed
D. pteronyssinus sensitization. However, the SSIgE test had a low negative predictive value (NPV) despite having a good LR (–) value (0.34), suggesting that a negative result of this test could not rule out
D. pteronyssinus sensitization. This finding is similar to that reported by Calabria et al. [
16] who showed that the SSIgE test showed better specificity than sensitivity for diagnosing
D. pteronyssinus sensitization. However, this result is different from that reported by Asha'ari et al. [
17] and Shyur et al. [
14] who showed good sensitivity but low specificity of the SSIgE test for diagnosing
D. pteronyssinus sensitization.
The SSIgE test using microfluidic array ELISA showed better sensitivity (77%) than specificity (64%) and high PPV (84%) and LR (+) value (2.1) for diagnosing
D. farinae sensitization, suggesting that a positive result of this test indicated sensitization to this allergen. However, a negative result of this test did not rule out
D. farinae sensitization because the NPV of this test was only 52%. The study by Shyur et al. [
14] reported that the SSIgE test showed good sensitivity of approximately 81.8% but low specificity of 37.5% for diagnosing
D. farinae sensitization. In contrast, the study by Calabria et al. [
16] reported that the SSIgE test showed better specificity (91.6%) than sensitivity (75.7%) for diagnosing
D. farinae sensitization.
The SSIgE test using microfluidic array ELISA showed high specificity (95%), PPV (97%), and LR (+) value (11) for diagnosing B. tropicalis sensitization, indicating that a positive result of this test confirmed B. tropicalis sensitization. However, this test had a sensitivity of only 48% and low NPV of 35% for B. tropicalis, indicating that a negative result of this test did not rule out B. tropicalis sensitization.
Accuracy of the SSIgE test using microfluidic array ELISA for diagnosing house dust mite sensitization in the present study was different from that reported in earlier studies by Asha'ari et al. [
17] in Malaysia and Shyur et al. [
14] in Taiwan. This difference may be because of the differences in the age of and type of allergic disease in patients included in these studies. The study by Shyur et al. [
14] included children aged 3–18 years, and the study by Asha'ari et al. [
17] included adult patients aged up to 65 years. The present study included patients aged 18–59 years to minimize the effect of extreme age on the results of wheal and flare reaction in the SPT. Moreover, the present study only included patients with respiratory allergic diseases, whereas the studies by Shyur et al. [
14] and Asha'ari et al. [
17] included patients with all types of allergic diseases.
The SSIgE test using microfluidic array ELISA showed good specificity (89%) but low sensitivity (3%) and predictive value for diagnosing dog dander sensitization. Moreover, the LR of this test did not improve the posttest probability to rule in or rule out dog dander sensitization. These findings indicate that the SSIgE test showed low accuracy for diagnosing dog dander sensitization. This result is similar to that reported by Shyur et al. [
14]. However, Calabria et al. [
16] reported better accuracy of the SSIgE test for diagnosing dog dander sensitization, with a sensitivity of 70.3% and specificity of 85.8%.
The SSIgE test using microfluidic array ELISA showed high specificity (88%) but low sensitivity, predictive value, and LR for diagnosing cat dander sensitization, indicating that the result of this test cannot be used to rule in or rule out cat dander sensitization. Calabria et al. [
16] also reported that the SSIgE test showed good accuracy for diagnosing cat dander sensitization. Prevalence of and exposure to pet allergens, mainly dog and cat dander, is higher in America than in Indonesia, which may be the reason for the difference in the accuracy of this test [
18].
The SSIgE test using microfluidic arraay ELISA showed high specificity (100%), PPV (100%), and LR (+) value (∞) for diagnosing cockroach allergen sensitization, suggesting that a positive result of this test indicated cockroach allergen sensitization. However, this test had a sensitivity of only 12% and low NPV (62%) and LR (–) value (0.8), suggesting that a negative result of this test did not rule out cockroach allergen sensitization. Moreover, this finding indicates an increased the chance of obtaining false-negative results. Thus, these findings indicate that although the SSIgE test has high specificity, PPV, and LR value, it has low sensitivity for diagnosing cockroach allergen sensitization. This finding is similar to that reported by Shyur et al. [
14] and Calabria et al. [
16] who showed low sensitivity and high specificity of the SSIgE test for diagnosing cockroach allergen sensitization.
In conclusion, the SSIgE test using microfluidic array ELISA showed moderate accuracy for diagnosing house dust mite sensitization and low accuracy for diagnosing cockroach allergen and dog and cat dander sensitization. These results indicate that the SSIgE test cannot replace the SPT for diagnosing inhalant allergen sensitization but can be used as alternative diagnostic tool for diagnosing house dust mite sensitization in patients who are contraindicated for or who do not respond to the SPT.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download