INTRODUCTION
MATERIALS AND METHODS
Subjects
Experimental groups
Surgical procedure
 | Figure 2Surgical procedures of the SL and DL open membrane healing technique. The procedures of the SL and DL groups were only different in the number of the resorbable collagen membranes used to cover the bone graft. (A) Extraction in the SL group. (B) DBBM-C insertion in the SL group. (C) Single-layer of collagen membrane coverage in the SL group. (D) The hidden X or the figure of 8 suture in the SL group. (E) Just before S-O. (F) Four months after extraction, immediately followed by dental implant placement. (G) Occlusal view of the final prosthesis. (H) Extraction in the DL group. (I) DBBM-C insertion in the DL group. (J) Double-layers of collagen membrane coverage in the DL group. (K) The hidden X or the figure of 8 suture in the DL group. (L) Just before S-O. (M) Four months after extraction, immediately followed by dental implant placement in the DL group. (N) Occlusal view of the final prosthesis in the DL group.
SL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a single-layer of a collagen membrane, DL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a double-layer of a collagen membrane, DBBM-C: deproteinized bovine bone mineral with 10% porcine collagen, S-O: stitch-out, 4M: 4 months after alveolar ridge preservation procedure.
|
Radiographic analysis
 | Figure 3Paraxial views from CBCT obtained 4 months after SL (A) and DL (B) ARP procedures.
CBCT: cone-beam computed tomography, SL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a single-layer of a collagen membrane, DL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a double-layer of a collagen membrane, ARP: alveolar ridge preservation, DBBM-C: deproteinized bovine bone mineral with 10% porcine collagen, CM: collagen membrane.
|
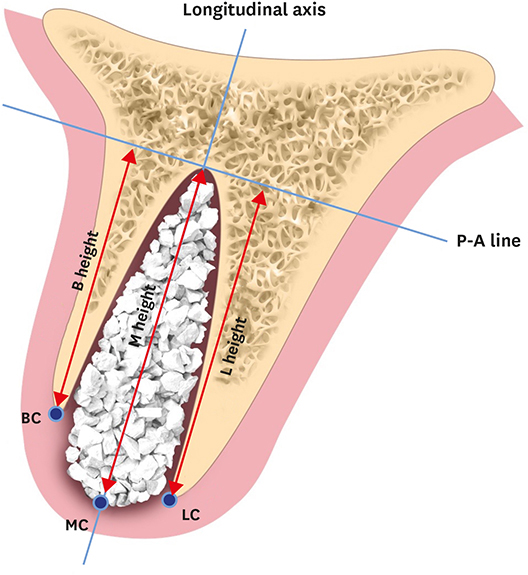
 | Figure 4Schematic drawing of references for measurements in the radiographic analysis.
P-A line: perpendicular line to the longitudinal axis at apex of the socket, BC: buccal crest, B height: height of the buccal cortical plate from the P-A line, LC: lingual/palatal crest, L height: height of the lingual/palatal plate from the P-A line, MC: mid-alveolar crest, M height: height of the mid-alveolar crest from the P-A line. |
Horizontal width in the 1-, 3-, and 5-mm subcrestal aspects (HW1, HW3, and HW5, respectively); the lines parallel to the P-A line lying 1-, 3-, and 5-mm apically from the MC line (the HW1, HW3, and HW5 lines, respectively) were identified and the distances between the peripheral points of the alveolar bone meeting the HW1, HW3, and HW5 were measured.
Vertical height in the buccal, lingual and middle aspects (BH, LH, and MH, respectively); the vertical distances between the P-A line and BC, LC, and MC (BH, LH, and MH, respectively) were measured.
RESULTS
Table 1
Horizontal and vertical ridge changes in the DL group from baseline to 4 months of healing

Table 2
Horizontal and vertical ridge changes in the SL group from baseline to 4 months of healing





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download