1. Muddugangadhar BC, Amarnath GS, Sonika R, Chheda PS, Garg A. Meta-analysis of failure and survival rate of implant-supported single crowns, fixed partial denture, and implant tooth-supported prostheses. J Int Oral Health. 2015; 7:11–17.
2. Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012; 23:Suppl 6. 2–21.
3. Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012; 23:Suppl 6. 22–38.

4. Albrektsson T, Isidor F. Consensus report of session IV. In : Lang NP, Karring T, editors. Proceedings of the 1st European Workshop on Periodontology. Chicago: Quintessence;1994. p. 365.
5. Lindhe J, Meyle J. Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the sixth European Workshop on Periodontology. J Clin Periodontol. 2008; 35:282–285.

6. Larsson L, Decker AM, Nibali L, Pilipchuk SP, Berglundh T, Giannobile WV. Regenerative medicine for periodontal and peri-implant diseases. J Dent Res. 2016; 95:255–266.

7. Fu JH, Wang HL. Can periimplantitis be treated? Dent Clin North Am. 2015; 59:951–980.

8. Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T. Peri-implantitis - onset and pattern of progression. J Clin Periodontol. 2016; 43:383–388.

9. Albrektsson T, Canullo L, Cochran D, De Bruyn H. “Peri-implantitis”: a complication of a foreign body or a man-made “Disease”. Facts and fiction. Clin Implant Dent Relat Res. 2016; 18:840–849.

10. Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015; 42:Suppl 16. S158–S171.

11. Salvi GE, Cosgarea R, Sculean A. Prevalence and mechanisms of peri-implant diseases. J Dent Res. 2017; 96:31–37.

12. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015; 86:611–622.

13. Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008; 35:292–304.

14. Monje A, Galindo-Moreno P, Tözüm TF, Suárez-López del Amo F, Wang HL. Into the paradigm of local factors as contributors for peri-implant disease: short communication. Int J Oral Maxillofac Implants. 2016; 31:288–292.

15. Heitz-Mayfield LJ, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 39–68.
16. Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015; 26:e8–16.

17. Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL, et al. Impact of maintenance therapy for the prevention of peri-implant diseases: a systematic review and meta-analysis. J Dent Res. 2016; 95:372–379.

18. Begg MD. Analysis of correlated responses. In : Lesaffre E, Feine J, Leroux B, Declerck D, editors. Statistical and methodological aspects of oral health research. Chichester: John Wiley & Sons;2009. p. 221–240.
19. Albrektsson T, Chrcanovic B, Östman PO, Sennerby L. Initial and long-term crestal bone responses to modern dental implants. Periodontol 2000. 2017; 73:41–50.

20. Roccuzzo M, De Angelis N, Bonino L, Aglietta M. Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clin Oral Implants Res. 2010; 21:490–496.

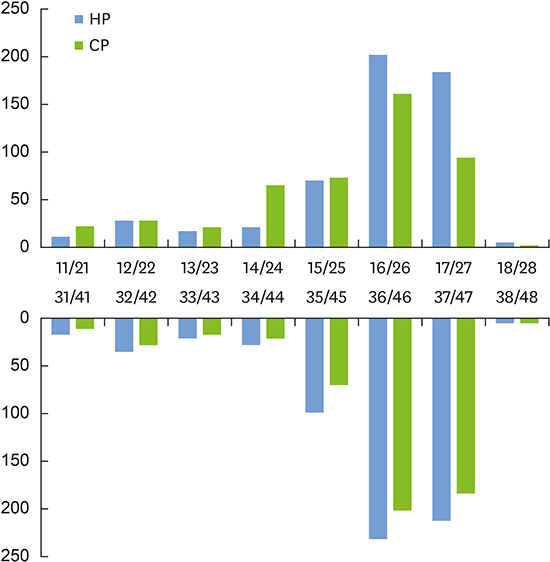
21. Chang M, Wennström JL. Bone alterations at implant-supported FDPs in relation to inter-unit distances: a 5-year radiographic study. Clin Oral Implants Res. 2010; 21:735–740.

22. Balshi TJ, Hernandez RE, Pryszlak MC, Rangert B. A comparative study of one implant versus two replacing a single molar. Int J Oral Maxillofac Implants. 1996; 11:372–378.

23. Jeong JS, Chang M. Food impaction and periodontal/peri-implant tissue conditions in relation to the embrasure dimensions between implant-supported fixed dental prostheses and adjacent teeth: a cross-sectional study. J Periodontol. 2015; 86:1314–1320.

24. Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman JL, Ewigman B, et al. Simplifying the language of evidence to improve patient care: strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. J Fam Pract. 2004; 53:111–120.
25. Blicher B, Joshipura K, Eke P. Validation of self-reported periodontal disease: a systematic review. J Dent Res. 2005; 84:881–890.

26. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Beck JD, et al. Self-reported measures for surveillance of periodontitis. J Dent Res. 2013; 92:1041–1047.

27. Coli P, Christiaens V, Sennerby L, Bruyn H. Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontol 2000. 2017; 73:203–217.

28. Koldsland OC, Scheie AA, Aass AM. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J Periodontol. 2010; 81:231–238.

29. Zetterqvist L, Feldman S, Rotter B, Vincenzi G, Wennström JL, Chierico A, et al. A prospective, multicenter, randomized-controlled 5-year study of hybrid and fully etched implants for the incidence of peri-implantitis. J Periodontol. 2010; 81:493–501.

30. Sanz M, Chapple IL. Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012; 39:Suppl 12. 202–206.









 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download