1. Kivity S, Agmon-Levin N, Blank M, Shoenfeld Y. Infections and autoimmunity--friends or foes? Trends Immunol. 2009; 30:409–414.
2. Vanderlugt CL, Begolka WS, Neville KL, Katz-Levy Y, Howard LM, Eagar TN, et al. The functional significance of epitope spreading and its regulation by co-stimulatory molecules. Immunol Rev. 1998; 164:63–72.

3. Lehmann PV, Forsthuber T, Miller A, Sercarz EE. Spreading of T-cell autoimmunity to cryptic determinants of an autoantigen. Nature. 1992; 358:155–157.

4. Vanderlugt CL, Neville KL, Nikcevich KM, Eagar TN, Bluestone JA, Miller SD. Pathologic role and temporal appearance of newly emerging autoepitopes in relapsing experimental autoimmune encephalomyelitis. J Immunol. 2000; 164:670–678.

5. van Noort JM, Bajramovic JJ, Plomp AC, van Stipdonk MJ. Mistaken self, a novel model that links microbial infections with myelin-directed autoimmunity in multiple sclerosis. J Neuroimmunol. 2000; 105:46–57.

6. Ercolini AM, Miller SD. The role of infections in autoimmune disease. Clin Exp Immunol. 2009; 155:1–15.

7. Steinman L. Despite epitope spreading in the pathogenesis of autoimmune disease, highly restricted approaches to immune therapy may still succeed [with a hedge on this bet]. J Autoimmun. 2000; 14:278–282.

8. Kurien BT, Scofield RH. Autoimmunity and oxidatively modified autoantigens. Autoimmun Rev. 2008; 7:567–573.

9. Vanderlugt CL, Miller SD. Epitope spreading in immune-mediated diseases: implications for immunotherapy. Nat Rev Immunol. 2002; 2:85–95.

10. Tabeta K, Yamazaki K, Hotokezaka H, Yoshie H, Hara K. Elevated humoral immune response to heat shock protein 60 (hsp60) family in periodontitis patients. Clin Exp Immunol. 2000; 120:285–293.

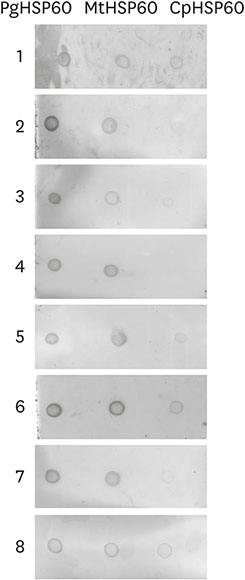
11. Choi J, Lee SY, Kim K, Choi BK. Identification of immunoreactive epitopes of the
Porphyromonas gingivalis heat shock protein in periodontitis and atherosclerosis. J Periodontal Res. 2011; 46:240–245.

12. Jeong E, Lee JY, Kim SJ, Choi J. Predominant immunoreactivity of
Porphyromonas gingivalis heat shock protein in autoimmune diseases. J Periodontal Res. 2012; 47:811–816.

13. Kwon EY, Cha GS, Jeong E, Lee JY, Kim SJ, Surh CD, et al. Pep19 drives epitope spreading in periodontitis and periodontitis-associated autoimmune diseases. J Periodontal Res. 2016; 51:381–394.

14. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012; 35:Suppl 1. S64–S71.
15. Joo JY, Cha GS, Chung J, Lee JY, Kim SJ, Choi J. Peptide 19 of Porphyromonas gingivalis heat shock protein is a potent inducer of low-density lipoprotein oxidation. J Periodontol. 2017; 88:e58–e64.
16. Yu M, Johnson JM, Tuohy VK. A predictable sequential determinant spreading cascade invariably accompanies progression of experimental autoimmune encephalomyelitis: a basis for peptide-specific therapy after onset of clinical disease. J Exp Med. 1996; 183:1777–1788.

17. Kamphuis S, Albani S, Prakken BJ. Heat-shock protein 60 as a tool for novel therapeutic strategies that target the induction of regulatory T cells in human arthritis. Expert Opin Biol Ther. 2006; 6:579–589.

18. Sfriso P, Ghirardello A, Botsios C, Tonon M, Zen M, Bassi N, et al. Infections and autoimmunity: the multifaceted relationship. J Leukoc Biol. 2010; 87:385–395.











 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download