1. Offenbacher S, Beck JD. Commentary: changing paradigms in the oral disease-systemic disease relationship. J Periodontol. 2014; 85:761–764. PMID:
24875011.

2. Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol. 1996; 67:1123–1137. PMID:
8910831.

3. Offenbacher S, Katz V, Fertik G, Collins J, Boyd D, Maynor G, et al. Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol. 1996; 67:1103–1113. PMID:
8910829.

4. Chistiakov DA, Orekhov AN, Bobryshev YV. Links between atherosclerotic and periodontal disease. Exp Mol Pathol. 2016; 100:220–235. PMID:
26777261.

5. Haynes WG, Stanford C. Periodontal disease and atherosclerosis: from dental to arterial plaque. Arterioscler Thromb Vasc Biol. 2003; 23:1309–1311. PMID:
12909566.
6. Haraszthy VI, Zambon JJ, Trevisan M, Zeid M, Genco RJ. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000; 71:1554–1560. PMID:
11063387.

7. Górska R, Gregorek H, Kowalski J, Laskus-Perendyk A, Syczewska M, Madaliński K. Relationship between clinical parameters and cytokine profiles in inflamed gingival tissue and serum samples from patients with chronic periodontitis. J Clin Periodontol. 2003; 30:1046–1052. PMID:
15002890.

8. Leibur E, Tuhkanen A, Pintson U, Söder PO. Prostaglandin E2 levels in blood plasma and in crevicular fluid of advanced periodontitis patients before and after surgical therapy. Oral Dis. 1999; 5:223–228. PMID:
10483068.

9. Bansal J, Bansal A, Kukreja N, Kukreja U. Periodontal diseases as an emerging potential risk factor for adverse pregnancy outcomes: a review of concepts. J Turk Ger Gynecol Assoc. 2011; 12:176–180. PMID:
24591987.

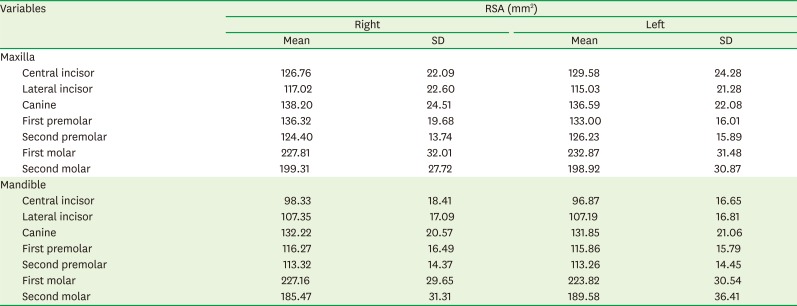
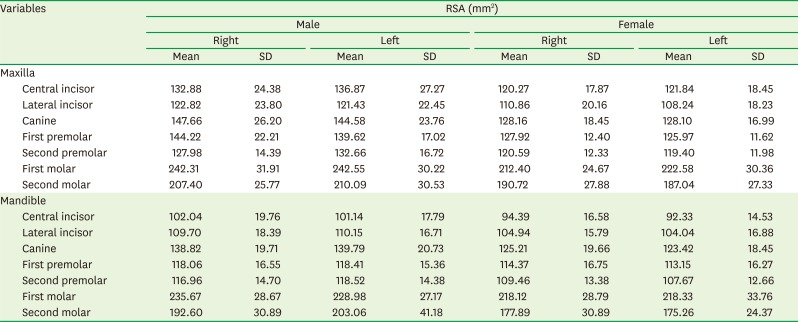
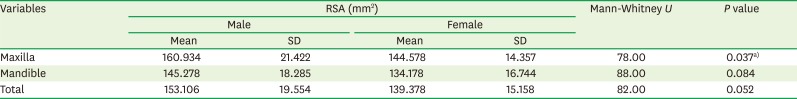
10. Hujoel PP, White BA, García RI, Listgarten MA. The dentogingival epithelial surface area revisited. J Periodontal Res. 2001; 36:48–55. PMID:
11246704.

11. Yamamoto T, Kinoshita Y, Tsuneishi M, Takizawa H, Umemura O, Watanabe T. Estimation of the remaining periodontal ligament from attachment-level measurements. J Clin Periodontol. 2006; 33:221–225. PMID:
16489949.

12. Nesse W, Abbas F, van der Ploeg I, Spijkervet FK, Dijkstra PU, Vissink A. Periodontal inflamed surface area: quantifying inflammatory burden. J Clin Periodontol. 2008; 35:668–673. PMID:
18564145.

13. Gu Y, Tang Y, Zhu Q, Feng X. Measurement of root surface area of permanent teeth with root variations in a Chinese population-A micro-CT analysis. Arch Oral Biol. 2016; 63:75–81. PMID:
26723016.

14. Choi JW, Kim N. Clinical application of three-dimensional printing technology in craniofacial plastic surgery. Arch Plast Surg. 2015; 42:267–277. PMID:
26015880.

15. Mattila K, Rasi V, Nieminen M, Valtonen V, Kesäniemi A, Syrjälä S, et al. von Willebrand factor antigen and dental infections. Thromb Res. 1989; 56:325–329. PMID:
2617473.

16. Syrjänen J, Peltola J, Valtonen V, Iivanainen M, Kaste M, Huttunen JK. Dental infections in association with cerebral infarction in young and middle-aged men. J Intern Med. 1989; 225:179–184. PMID:
2703800.
17. Bahekar AA, Singh S, Saha S, Molnar J, Arora R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J. 2007; 154:830–837. PMID:
17967586.

18. Blaizot A, Vergnes JN, Nuwwareh S, Amar J, Sixou M. Periodontal diseases and cardiovascular events: meta-analysis of observational studies. Int Dent J. 2009; 59:197–209. PMID:
19774803.
19. Simpson TC, Weldon JC, Worthington HV, Needleman I, Wild SH, Moles DR, et al. Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2015; CD004714. PMID:
26545069.

20. Teeuw WJ, Gerdes VE, Loos BG. Effect of periodontal treatment on glycemic control of diabetic patients: a systematic review and meta-analysis. Diabetes Care. 2010; 33:421–427. PMID:
20103557.
21. Boggess KA, Moss K, Madianos P, Murtha AP, Beck J, Offenbacher S. Fetal immune response to oral pathogens and risk of preterm birth. Am J Obstet Gynecol. 2005; 193:1121–1126. PMID:
16157123.

22. Chiu B. Multiple infections in carotid atherosclerotic plaques. Am Heart J. 1999; 138:S534–S536. PMID:
10539867.

23. Jared H, Boggess KA, Moss K, Bose C, Auten R, Beck J, et al. Fetal exposure to oral pathogens and subsequent risk for neonatal intensive care admission. J Periodontol. 2009; 80:878–883. PMID:
19485816.

24. Mustapha IZ, Debrey S, Oladubu M, Ugarte R. Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: a systematic review and meta-analysis. J Periodontol. 2007; 78:2289–2302. PMID:
18052701.

25. Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J Clin Periodontol. 2008; 35:277–290. PMID:
18294231.

26. Al-Shammari KF, Al-Khabbaz AK, Al-Ansari JM, Neiva R, Wang HL. Risk indicators for tooth loss due to periodontal disease. J Periodontol. 2005; 76:1910–1918. PMID:
16274310.

27. Burt B. Research, Science and Therapy Committee of the American Academy of Periodontology. Position paper: epidemiology of periodontal diseases. J Periodontol. 2005; 76:1406–1419. PMID:
16101377.
28. Kamburoğlu K, Kolsuz E, Kurt H, Kiliç C, Özen T, Paksoy CS. Accuracy of CBCT measurements of a human skull. J Digit Imaging. 2011; 24:787–793. PMID:
20857166.

29. Shen P, Zhao J, Fan L, Qiu H, Xu W, Wang Y, et al. Accuracy evaluation of computer-designed surgical guide template in oral implantology. J Craniomaxillofac Surg. 2015; 43:2189–2194. PMID:
26776292.

30. Forst D, Nijjar S, Flores-Mir C, Carey J, Secanell M, Lagravere M. Comparison of
in vivo 3D cone-beam computed tomography tooth volume measurement protocols. Prog Orthod. 2014; 15:69. PMID:
25534123.

31. Li W, Chen F, Zhang F, Ding W, Ye Q, Shi J, et al. Volumetric measurement of root resorption following molar mini-screw implant intrusion using cone beam computed tomography. PLoS One. 2013; 8:e60962. PMID:
23585866.

32. Wang Y, He S, Yu L, Li J, Chen S. Accuracy of volumetric measurement of teeth
in vivo based on cone beam computer tomography. Orthod Craniofac Res. 2011; 14:206–212. PMID:
22008300.
33. Al-Rawi B, Hassan B, Vandenberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from cone beam computed tomography scans. J Oral Rehabil. 2010; 37:352–358. PMID:
20180895.

34. Kim I, Paik KS, Lee SP. Quantitative evaluation of the accuracy of micro-computed tomography in tooth measurement. Clin Anat. 2007; 20:27–34. PMID:
16372341.

35. Acar B, Kamburoğlu K, Tatar İ, Arıkan V, Çelik HH, Yüksel S, et al. Comparison of micro-computerized tomography and cone-beam computerized tomography in the detection of accessory canals in primary molars. Imaging Sci Dent. 2015; 45:205–211. PMID:
26730367.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download