INTRODUCTION
MATERIALS AND METHODS
Sample preparation
Cell culture
Nitrite production measurements
Cell viability measurements using the MTT assay
ELISA for PGE2, IL-1β, and IL-6 release measurements
iNOS, COX2, and p44/42 MAPK measurements by western blotting
NF-κB activity measurements
Statistical analysis
RESULTS
Effects of M and Z on Pam3CSK4-induced NO production by RAW 264.7 cells
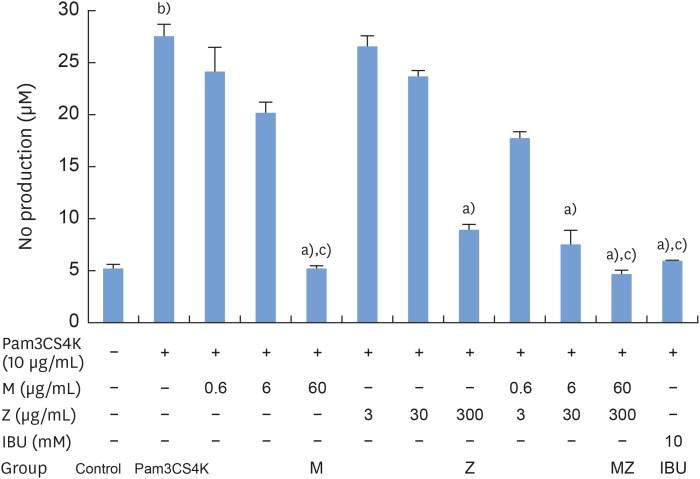 | Figure 1Effects of M and Z on Pam3CSK4-induced NO production in RAW 264.7 cells. Cells (5×104/cm2) were treated with M, Z, MZ, or IBU and 10 μg/mL Pam3CSK4 for 24 hours at 37°C. In experiments without Pam3CSK4, the medium alone was used as a negative control, and IBU was used as a positive control. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, NO: nitric oxide, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control; c)P<0.05 in comparison with Z.
|
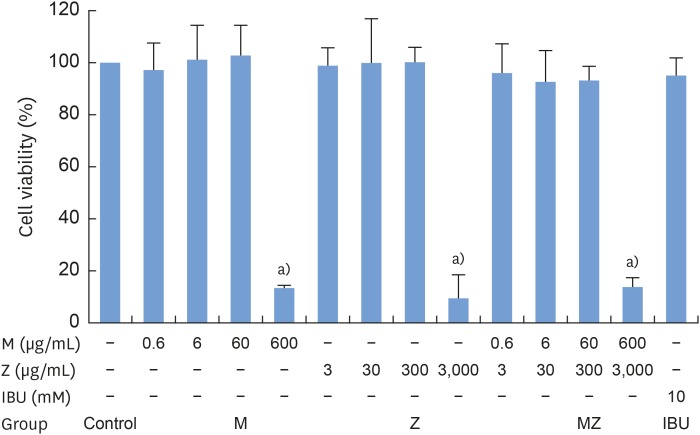 | Figure 2Cytotoxicity of M and Z treatments in RAW 264.7 cells. Cells (3.3×104/cm2) were treated with M, Z, or IBU for 24 hours at 37°C. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide, MZ: the combination treatment of M and Z.
a)P<0.05 in comparison with the control.
|
Effects of M and Z on PGE2, IL-1β, and IL-6 production in Pam3CSK4-induced RAW 264.7 cells
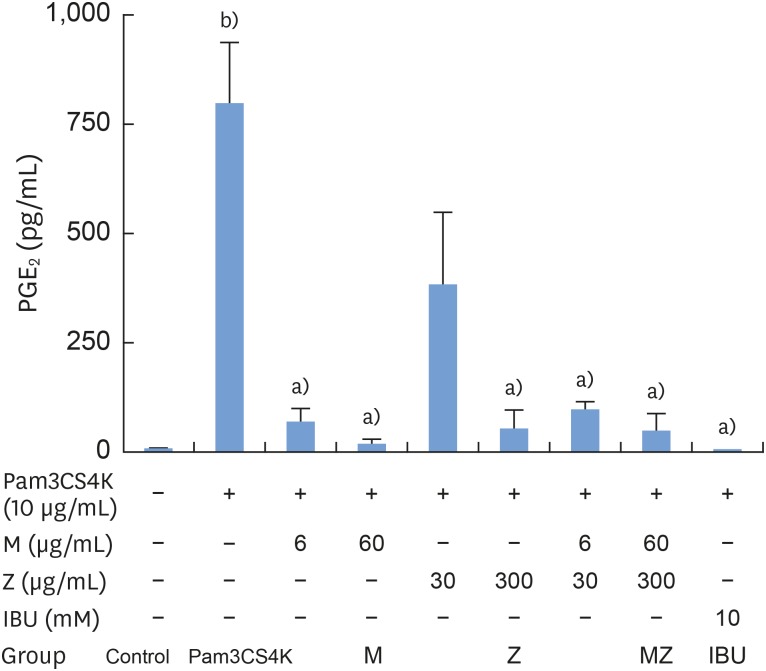 | Figure 3Effects of M and Z on Pam3CSK4-induced PGE2 formation in RAW 264.7 cells. Cells (5×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes before treatment with 10 μg/mL Pam3CSK4 for 24 hours at 37°C. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, PGE2: prostaglandin E2, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control.
|
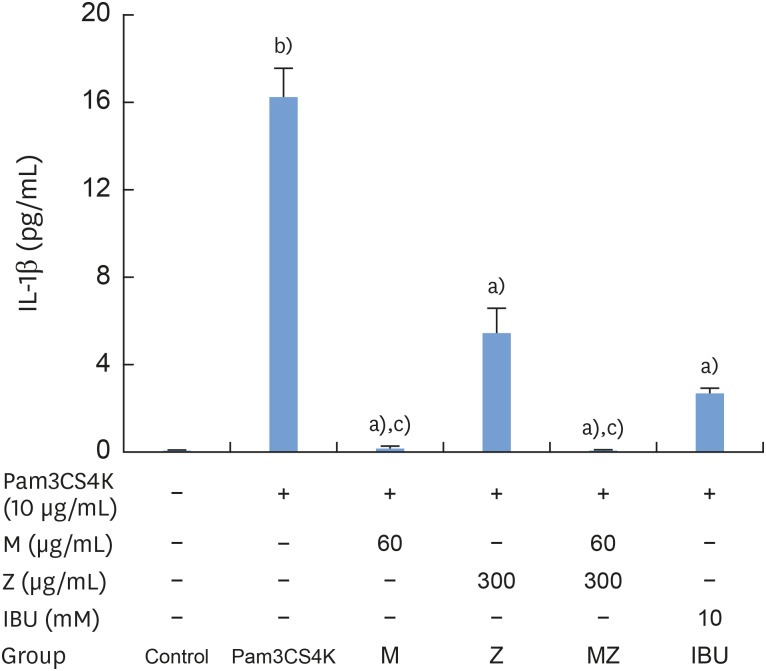 | Figure 4Effects of M and Z on Pam3CSK4-induced IL-1β formation in RAW 264.7 cells. Cells (5×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes before treatment with 10 μg/mL Pam3CSK4 for 24 hours at 37°C. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, IL-1β: interleukin-1β, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control; c)P<0.05 in comparison with both Z and IBU.
|
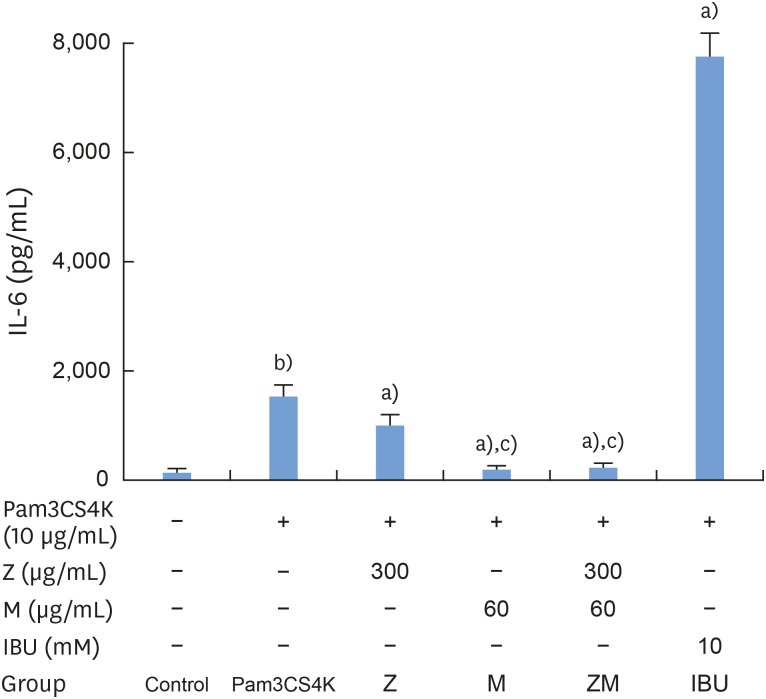 | Figure 5Effects of M and Z on Pam3CSK4-induced IL-6 formation in RAW 264.7 cells. Cells (5×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes before treatment with 10 μg/mL Pam3CSK4 for 24 hours at 37°C. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, IL-6: interleukin-6, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control; c)P<0.05 in comparison with M.
|
Effects of M and Z on p44/42 MAPK activation in Pam3CSK4-induced RAW 264.7 cells
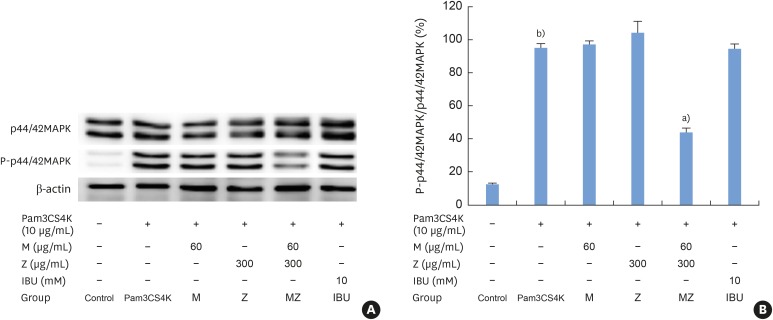 | Figure 6Effects of M and Z on nuclear p44/42 MAPK expression levels in Pam3CSK4-induced RAW 264.7 cells. The levels of p44/42 MAPK and β-actin expression were detected by western blotting using specific antibodies. Cells (1.9×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes before being treated with 10 μg/mL Pam3CSK4. To detect p44/42 MAPK expression, Pam3CSK4 was added for 30 minutes at 37°C. The blots shown here are representative of 3 independent experiments. Each sample contained 10 μg of total protein. (A) The levels of p44/42 MAPK, P-p44/42 MAPK and β-actin expression; (B) ratio of P-p44/42 MAPK to p44/42 MAPK expressed as a percentage.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), MAPK: mitogen-activated protein kinase, Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control.
|
Effects of M and Z on iNOS, and COX-2 expression in Pam3CSK4-induced RAW 264.7 cells
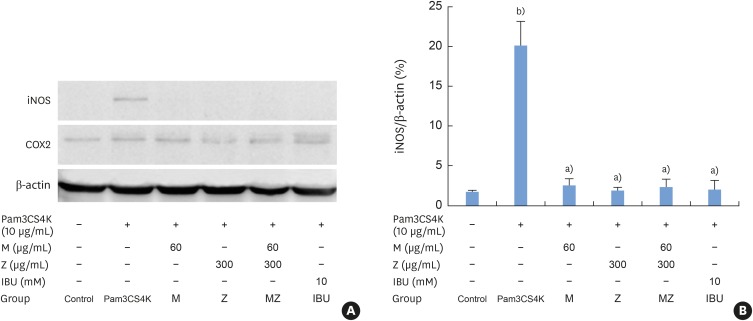 | Figure 7Effects of M and Z on nuclear iNOS and COX-2 expression levels in Pam3CSK4-induced RAW 264.7 cells. The levels of iNOS, COX-2, and β-actin expression were detected by western blotting using specific antibodies. Cells (1.9×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes before being treated with 10 μg/mL Pam3CSK4. To detect iNOS and COX-2 expression, Pam3CSK4 was added for 24 hours at 37°C. The blots shown here are representative of 3 independent experiments. Each sample contained 10 μg of total protein. (A) The levels of iNOS, COX-2, and β-actin expression; (B) ratio of iNOS to β-actin expressed as a percentage.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), iNOS: inducible nitric oxide synthase, COX-2: cyclooxygenase-2, Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control.
|
Effects of M and Z on Pam3CSK4-induced NF-κB transactivation in RAW 264.7 cells
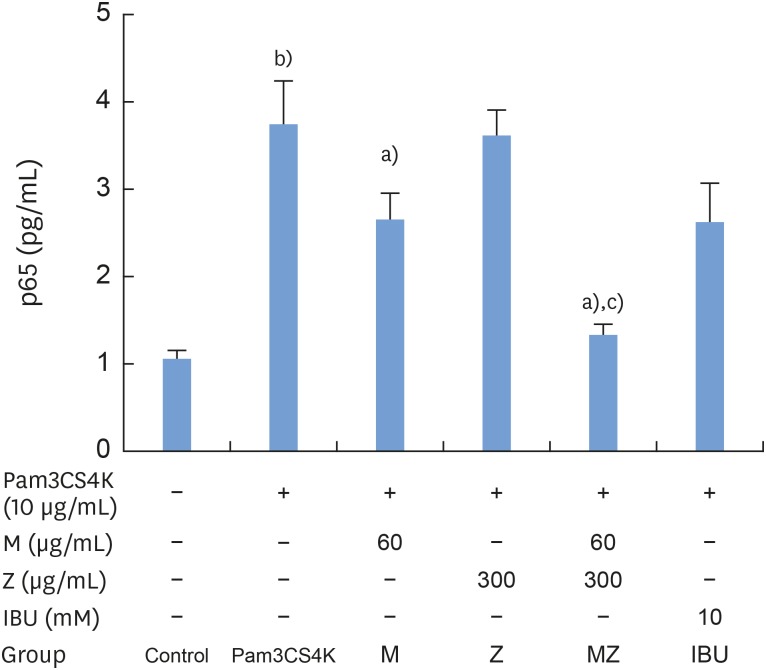 | Figure 8Effects of M and Z on Pam3CSK4-induced NF-κB transactivation in RAW 264.7 cells. Cells (5×104/cm2) were treated with M, Z, MZ, or IBU for 30 minutes prior to treatment with 10 μg/mL Pam3CSK4 for 2 hours at 37°C. The data are expressed as mean±standard deviation, as obtained from 6 separate experiments.M: soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, NF-κB: nuclear transcription factor κB, MZ: the combination treatment of M and Z, IBU: ibuprofen (10 mM in 1% DMSO), DMSO: dimethyl sulfoxide, p65: transcription factor p65.
a)P<0.05 in comparison with Pam3CSK4; b)P<0.05 in comparison with the control; c)P<0.05 in comparison with M and Z.
|
DISCUSSION
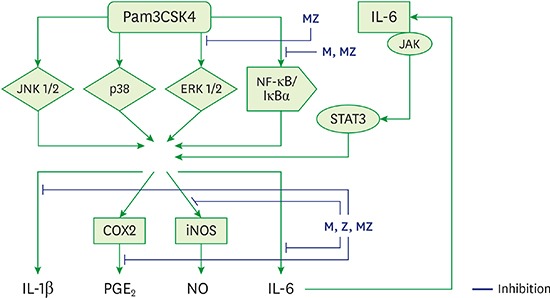
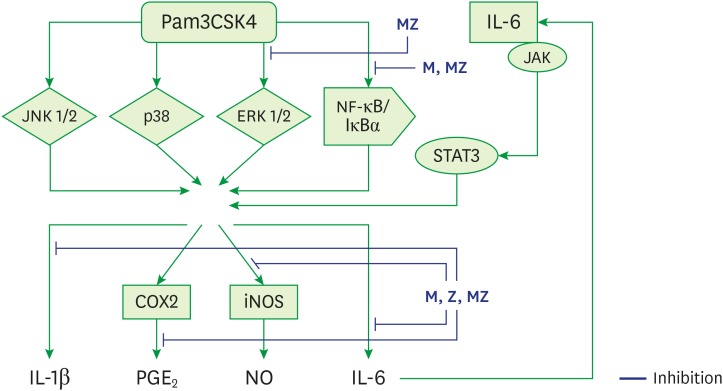 | Figure 9Schematic model for the anti-inflammatory mechanism of M and Z in Pam3CSK4-induced RAW 264.7 cells.ML soft 75% ethanol Magnoliae Cortex extract (60 μg/mL in 1% DMSO), Z: titrated unsaponifiable maize extract fraction (300 μg/mL in 1% DMSO), Pam3CSK4: synthetic Toll-like receptors of Porphyromonas gingivalis, MZ: the combination treatment of M and Z, JNK 1/2: c-Jun N-terminal kinase 1/2, p38: p38 mitogen-activated protein kinase, ERK 1/2: extracellular signal-regulated kinase 1/2, NF-κB/IκBα: nuclear transcription factor κB pathway, JAK/STAT3: Janus kinase/signal transduction and activator of transcription 3 signaling pathway, iNOS: inducible nitric oxide synthase, COX-2: cyclooxygenase-2, IL: interleukin; PGE2: prostaglandin E2, NO: nitric oxide, DMSO: dimethyl sulfoxide.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download