1. Salvi GE, Ramseier CA. Efficacy of patient-administered mechanical and/or chemical plaque control protocols in the management of peri-implant mucositis. A systematic review. J Clin Periodontol. 2015; 42:Suppl 16. S187–S201.

2. Linden GJ, Lyons A, Scannapieco FA. Periodontal systemic associations: review of the evidence. J Clin Periodontol. 2013; 40:Suppl 14. S8–S19.

3. Reichert S, Haffner M, Keysser G, Schafer C, Stein JM, Schaller HG, et al. Detection of oral bacterial DNA in synovial fluid. J Clin Periodontol. 2013; 40:591–598.

4. Tonetti MS, Van Dyke TE. Working group 1 of the joint EFP/AAP workshop. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol. 2013; 40:Suppl 14. S24–S29.
5. Kornman KS, Loe H. The role of local factors in the etiology of periodontal diseases. Periodontol 2000. 1993; 2:83–97.

6. Haffajee AD, Socransky SS. Microbial etiological agents of destructive periodontal diseases. Periodontol 2000. 1994; 5:78–111.

7. Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review. Clin Oral Implants Res. 2015; 26:Suppl 11. 15–44.

8. Chapple IL, Van der Weijden F, Doerfer C, Herrera D, Shapira L, Polak D, et al. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015; 42:Suppl 16. S71–S76.

9. Serino G, Strom C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009; 20:169–174.

10. Aguirre-Zorzano LA, Estefania-Fresco R, Telletxea O, Bravo M. Prevalence of peri-implant inflammatory disease in patients with a history of periodontal disease who receive supportive periodontal therapy. Clin Oral Implants Res. 2015; 26:1338–1344.

11. Figuero E, Nobrega DF, Garcia-Gargallo M, Tenuta LM, Herrera D, Carvalho JC. Mechanical and chemical plaque control in the simultaneous management of gingivitis and caries: a systematic review. J Clin Periodontol. 2017; 44:Suppl 18. S116–S134.

12. Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962; 65:26–29.

13. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.

14. Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970; 41:41–43.

15. O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972; 43:38.
16. Rustogi KN, Curtis JP, Volpe AR, Kemp JH, McCool JJ, Korn LR. Refinement of the Modified Navy Plaque Index to increase plaque scoring efficiency in gumline and interproximal tooth areas. J Clin Dent. 1992; 3:C9–C12.
17. Renton-Harper P, Claydon N, Warren P, Newcombe RG, Addy M. Conversion of plaque-area measurements to plaque index scores. An assessment of variation and discriminatory power. J Clin Periodontol. 1999; 26:429–433.
18. Matthijs S, Sabzevar MM, Adriaens PA. Intra-examiner reproducibility of 4 dental plaque indices. J Clin Periodontol. 2001; 28:250–254.

19. Dababneh RH, Khouri AT, Smith RG, Addy M. A new method of plaque scoring: a laboratory comparison with other plaque indices. J Clin Periodontol. 2002; 29:832–837.

20. McCracken GI, Preshaw PM, Steen IN, Swan M, deJager M, Heasman PA. Measuring plaque in clinical trials: index or weight? J Clin Periodontol. 2006; 33:172–176.

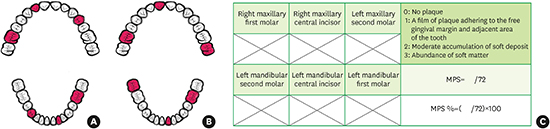
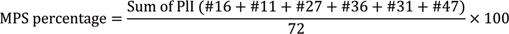
21. Deinzer R, Jahns S, Harnacke D. Establishment of a new marginal plaque index with high sensitivity for changes in oral hygiene. J Periodontol. 2014; 85:1730–1738.

22. Butler BL, Morejon O, Low SB. An accurate, time-efficient method to assess plaque accumulation. J Am Dent Assoc. 1996; 127:1763–1766.

23. Davies GN. The different requirements of periodontal indices for prevalence studies and clinical trials. Int Dent J. 1968; 18:560–569.
24. Tonetti MS, Claffey N. European Workshop in Periodontology group C. Advances in the progression of periodontitis and proposal of definitions of a periodontitis case and disease progression for use in risk factor research. Group C consensus report of the 5th European Workshop in Periodontology. J Clin Periodontol. 2005; 32:Suppl 6. 210–213.

25. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010; 1:100–107.

26. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.

27. Haffajee AD, Teles RP, Patel MR, Song X, Yaskell T, Socransky SS. Factors affecting supragingival biofilm composition. II. Tooth position. J Periodontal Res. 2009; 44:520–528.
28. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995; 152:1423–1433.
29. Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002; 15:25–38.
30. Kerse N, Buetow S, Mainous AG 3rd, Young G, Coster G, Arroll B. Physician-patient relationship and medication compliance: a primary care investigation. Ann Fam Med. 2004; 2:455–461.

31. Dababneh RH, Khouri AT, Smith RG, Addy M. Correlation and examiner agreement between a new method of plaque scoring and a popular established plaque index, modelled
in vitro. J Clin Periodontol. 2002; 29:1107–1111.

32. Van der Weijden GA, Timmerman MF, Nijboer A, Lie MA, Van der Velden U. A comparative study of electric toothbrushes for the effectiveness of plaque removal in relation to toothbrushing duration. Timerstudy. J Clin Periodontol. 1993; 20:476–481.

33. Van der Weijden FA, Slot DE. Efficacy of homecare regimens for mechanical plaque removal in managing gingivitis a meta review. J Clin Periodontol. 2015; 42:Suppl 16. S77–S91.

34. de Freitas GC, Pinto TM, Grellmann AP, Dutra DA, Susin C, Kantorski KZ, et al. Effect of self-performed mechanical plaque control frequency on gingival inflammation revisited: a randomized clinical trial. J Clin Periodontol. 2016; 43:354–358.

35. Ahn JK, Kim JB. An experimental study on the effects of the toothbrushing instructional methods. J Korean Acad Dent Health. 1985; 9:127–133.
36. Harnacke D, Stein K, Stein P, Margraf-Stiksrud J, Deinzer R. Training in different brushing techniques in relation to efficacy of oral hygiene in young adults: a randomized controlled trial. J Clin Periodontol. 2016; 43:46–52.

37. Harnacke D, Beldoch M, Bohn GH, Seghaoui O, Hegel N, Deinzer R. Oral and written instruction of oral hygiene: a randomized trial. J Periodontol. 2012; 83:1206–1212.












 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download