Although pharmacotherapy is considered the second line treatment for post-traumatic stress disorder (PTSD),
1,2 medication is still the most commonly referred treatment option for this chronic and debilitating illness. For example, among 186,460 Iraq and Afghanistan veterans with PTSD enrolled in Veterans Affairs care, 80.1% received psychotropic medication.
3 The referral rate for medication from the US general hospital settings is also substantial; of 1,848 individuals with a diagnosis of PTSD, 74.6% and 63.0% received psychotherapy and medication respectively, and 37.6% were treated with both treatment modalities.
4
Despite the popularity of pharmacotherapy as the most frequently offered treatment for PTSD, the overall response rates from clinical trials with selective serotonin reuptake inhibitors (SSRIs), the mostly recommended pharmacological agents for PTSD, range from 50%–60% and only 20%–30% of patients achieve complete remission of symptoms.
5,6 Moreover, next-step treatment strategies for these individuals who failed to respond, such as combination therapy or a switch to other medications or psychotherapy, are poorly understood. In this context, trauma-focused psychotherapies were examined for the possible next-step candidates of poor medication responders including cognitive behavior therapy (CBT), interpersonal psychotherapy, and prolonged exposure.
7-11
As an alternative to these treatments usually delivered for 10–16 sessions, eye movement desensitization and reprocessing (EMDR) therapy is the other option from evidence-based psychotherapeutic strategies.
2,12 EMDR therapy is a trans-diagnostic, integrative psychotherapy approach, which is intrinsically client-centered at its core.
13 It has been extensively researched and proven effective for the treatment of adverse life experiences.
12 It utilizes a theoretical framework known as adaptive information processing (AIP). The context of AIP is that adverse life experiences cause imbalance in the nervous system thus creating blockages or incomplete information processing, namely trauma memories. These inappropriately stored episodic memories, which include the perceptions, sensations, beliefs and emotions that occurred at the time of the adverse life event, can be triggered by current internal and external stimuli, contributing to ongoing dysfunction.
12,14 This model, developed in the early 1990's, has since demonstrated the role played by disturbing life events in the genesis of many forms of psychological and somatic symptomology, including PTSD.
12 To investigate the benefit of adding EMDR therapy as a sequencing treatment strategy for PTSD in patients who failed to initially respond, we analyzed naturalistic cohort data of EMDR at an outpatient trauma clinic.
The original data included 51 adult patients with a current Diagnostic and Statistical Manual for Mental Disorders – fourth edition (DSM-IV) PTSD diagnosis who received at least one session of EMDR and psychotropic medication at a psychological trauma clinic, Hanyang University Guri Hospital in Gyeonggi Province, Korea. Their PTSD and comorbid diagnoses were confirmed by the Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version.
15 Inclusion criteria were a total score greater than 45 on the Clinician Administered PTSD Scale (CAPS),
16,17 age between 18 to 64, and ability to read and write. Exclusion criteria were comorbid psychotic illness and neurological or cognitive disorders.
18
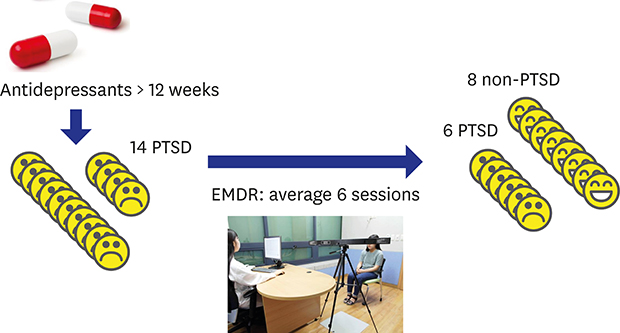
Subjects were included in this analysis if they had received at least 12 weeks of one or more antidepressants at maximal tolerable dose (for example, at least fluoxetine 20 mg/day, sertraline 50 mg, and paroxetine 20 mg) before initiation of EMDR therapy. These criteria reflect the stringent standard for minimal effective dose and duration for antidepressant trials for adult PTSD.
19 Of 51 patients, 29 (57%) were excluded because they were not given medication at least 12 weeks prior to EMDR treatment. Among the 22 remaining patients, two did not receive antidepressants, two did not have detailed information for dose and four had an inadequate dose of antidepressants leaving 14 for final analysis.
Among these 14 patients, eight were women (57.1%), eight were married (57.1%), and nine had more than high school education (64.3%). The mean age of participants was 40.5 (standard deviation [SD], 13.2; 95% confidence interval [CI], 32.9–48.1; range, 22–61). The index traumatic event of participants was motor vehicle accident (n = 12), industrial accident (n = 1) and family violence (n = 1). The median duration of illness was 7 months (range = 3–150). Six patients had two comorbid psychiatric diagnoses other than PTSD, another six had one, and two had no comorbidity. Baseline CAPS score was 69.6 (SD, 13.6; 95% CI, 61.7–77.5; range, 46–105).
We used The CAPS for measurement, which is a gold standard interview-based instrument for diagnosis of DSM-IV PTSD.
16 It contains 17 items of DSM-IV criteria for PTSD symptoms and each item is rated for two categories of frequency and intensity and each scored between 0 and 4. A symptom of PTSD is considered present if the sum of frequency and intensity is more than 4 in this study.
20
EMDR therapy was delivered weekly for a mean of 5.9 sessions (SD, 2.4; 95% CI, 2.5–7.3; range, 2–10) depending on the clinical needs and complexity of problems. The second author administered EMDR for 10 cases (71.4%) and four psychiatric residents each treated one of the other patients. Participants remained on the same dose of medication during the therapy.
Paired t test was used for pre- and post-treatment comparison. Spearman's correlation was applied for the decrease in the CAPS score and demographic or clinical variables. Statistical significance was set at P value of 0.05 bidirectionally and all the analyses were conducted with IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA).
The protocol of this study was reviewed and approved by the Institutional Review Board (IRB) of Hanyang University Guri Hospital (approval No. 20121119). All the participants submitted the written informed consents when they were enrolled.
The median time of prior dose-adequate antidepressant therapy was 3.5 months (range, 3–15) and three participants had received two concomitant antidepressants. Antidepressant prescribed were sertraline (50–100 mg, n = 2), paroxetine (40 mg, n = 2), escitalopram (20 mg, n = 2), venlafaxine (150 mg, n = 2), duloxetine (60 mg, n = 2), tianeptine (37.5 mg, n = 2), mirtazapine (15–30 mg, n = 2), trazodone (200 mg, n = 1), and amitriptyline (100 mg, n = 1). Comparison between baseline and after medication indicated a statistically significant decrease in CAPS symptoms (t = 2.3, df = 13, P = 0.035) with a mean reduction of 8.1% (SD, 12.7; range, 14–32; 95% CI, 0.9–15.4).
The participant showed a mean 32.7% decrease in CAPS scores (SD, 26.4; range, −3.9–72.0; 95% CI, 17.5–48.0); 7 (50%) responded with a more than 30% decrease in the total CAPS score and 8 (57%) lost the PTSD diagnosis (
Table 1). When these seven participants were followed up at 6 months, four showed similar results, one further improved to the level of complete remission (CAPS score < 20), and one had lost the benefit and met the diagnostic criteria for PTSD again (
Table 2). No statistical differences were found for response and decrease in CAPS scores between those who were followed-up and those who were not.
In this study, among 14 patients who failed to respond to an initial 12-week trial of antidepressant, seven responded with a greater than 30% decrease in the total CAPS score and eight (57%) lost the PTSD diagnosis. This is comparable to findings from a previous study in which CBT was added to therapy for pharmacotherapy-resistant patients with PTSD and 60% in the immediate treatment group (n = 20) and 50% in the delayed treatment group (n = 20) lost their PTSD diagnosis.
8 It is noteworthy that the number of sessions administered with EMDR therapy was smaller (i.e., about six sessions) than the 10 to 12 sessions reported in previous psychotherapy studies.
21 This may favor EMDR as add-on psychotherapy after failure of pharmacotherapy in terms of cost-effectiveness; in support of this view, EMDR showed a sharper decline in the pattern of reduction in PTSD symptoms than trauma-focused CBT.
22
However, participants in three CBT studies had longer duration of SSRI treatment (at least 6 or 12 months) with the maximally tolerated dose prior to adding psychotherapy and are therefore more likely to be labeled pharmacotherapy-resistant or refractory.
8-10 One study noted that 55% of SSRI non-responders turned into responders after additional 6-month continuation of the same drug, suggesting that a more extended period of continued medication may be needed.
23 However, it is generally recommended that at least 8 to 12 weeks of SSRIs or serotonin and norepinephrine reuptake inhibitors (SNRIs) at maximal tolerable dose should be given to judge treatment response
24; one clinical trial of pharmacotherapy with PTSD defined SSRI resistance as less than a 30% decrease of PTSD symptoms (based on CAPS scores) after 8 weeks of sertraline at a dose of 25 mg to 200 mg.
24 Therefore, our participants at least meet the criteria for failure of treatment response.
Our finding also broadly supports the current opinions of experts that either a switch to another medication or addition of psychotherapy should be considered when initial pharmacotherapy with SSRIs or SNRIs fails.
21 Further studies are necessary to examine whether switching to another type of medication or adding trauma-focused psychotherapy will provide the greatest benefit.
The first limitation of this study is that this is not a prospective clinical trial without control group. Secondly, we do not have information for patients who improved after initial antidepressant pharmacotherapy and there may be selection bias concerning which patients received additional trauma psychotherapy. Thirdly, the treatment dose of EMDR may be insufficient given that clinical trials typically administered the therapy at 8–12 sessions.
22,25 However, in the real-world practice, trauma-focused psychotherapies are delivered at fewer sessions (median, 5 sessions).
26 Further clinical trials are needed to determine best practice for combined and sequential approaches with medication and trauma-focused psychotherapy.
In conclusion, EMDR therapy seems to be a good option for addition to psychotherapy when initial pharmacotherapy fails to improve PTSD conditions with the additional benefit of cost-effectiveness (fewer sessions and no homework assignment).





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download