1. McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009; 49(5):Suppl. S45–S55. PMID:
19399792.

2. Della Corte C, Nobili V, Comparcola D, Cainelli F, Vento S. Management of chronic hepatitis B in children: an unresolved issue. J Gastroenterol Hepatol. 2014; 29(5):912–919. PMID:
24863185.

3. Chang MH, Chen TH, Hsu HM, Wu TC, Kong MS, Liang DC, et al. Prevention of hepatocellular carcinoma by universal vaccination against hepatitis B virus: the effect and problems. Clin Cancer Res. 2005; 11(21):7953–7957. PMID:
16278421.

4. Chen HL, Lin LH, Hu FC, Lee JT, Lin WT, Yang YJ, et al. Effects of maternal screening and universal immunization to prevent mother-to-infant transmission of HBV. Gastroenterology. 2012; 142(4):773–781.e2. PMID:
22198276.

5. Hong SJ, Park HJ, Chu MA, Choi BS, Choe BH. The rate of conversion from immune-tolerant phase to early immune-clearance phase in children with chronic hepatitis B virus infection. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(1):41–46. PMID:
24749087.

6. Kasırga E. Lamivudine resistance in children with chronic hepatitis B. World J Hepatol. 2015; 7(6):896–902. PMID:
25937866.

7. Shah U, Kelly D, Chang MH, Fujisawa T, Heller S, González-Peralta RP, et al. Management of chronic hepatitis B in children. J Pediatr Gastroenterol Nutr. 2009; 48(4):399–404. PMID:
19322053.

8. Jonas MM, Block JM, Haber BA, Karpen SJ, London WT, Murray KF, et al. Treatment of children with chronic hepatitis B virus infection in the United States: patient selection and therapeutic options. Hepatology. 2010; 52(6):2192–2205. PMID:
20890947.

9. Sokal EM, Paganelli M, Wirth S, Socha P, Vajro P, Lacaille F, et al. Management of chronic hepatitis B in childhood: ESPGHAN clinical practice guidelines: consensus of an expert panel on behalf of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J Hepatol. 2013; 59(4):814–829. PMID:
23707367.
10. Hong SJ, Kim YH, Choe BH, Park HJ, Tak WY, Kweon YO. Current role of Lamivudine regarding therapeutic response and resistance in children with chronic hepatitis B. Pediatr Gastroenterol Hepatol Nutr. 2013; 16(2):80–88. PMID:
24010111.

11. Vajro P, Veropalumbo C, Maddaluno S, Salerno M, Parenti G, Pignata C. Treatment of children with chronic viral hepatitis: what is available and what is in store. World J Pediatr. 2013; 9(3):212–220. PMID:
23929253.

12. Jonas MM, Kelly D, Pollack H, Mizerski J, Sorbel J, Frederick D, et al. Safety, efficacy, and pharmacokinetics of adefovir dipivoxil in children and adolescents (age 2 to <18 years) with chronic hepatitis B. Hepatology. 2008; 47(6):1863–1871. PMID:
18433023.
13. Chang TT, Gish RG, de Man R, Gadano A, Sollano J, Chao YC, et al. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. N Engl J Med. 2006; 354(10):1001–1010. PMID:
16525137.

14. Jonas MM, Chang MH, Sokal E, Schwarz KB, Kelly D, Kim KM, et al. Randomized, controlled trial of entecavir versus placebo in children with hepatitis B envelope antigen-positive chronic hepatitis B. Hepatology. 2016; 63(2):377–387. PMID:
26223345.

15. Chang KC, Wu JF, Hsu HY, Chen HL, Ni YH, Chang MH. Entecavir treatment in children and adolescents with chronic hepatitis B virus infection. Pediatr Neonatol. 2016; 57(5):390–395. PMID:
26806847.

16. Pawłowska M, Domagalski K, Smok B, Rajewski P, Wietlicka-Piszcz M, Halota W, et al. Continuous up to 4 years entecavir treatment of HBV-infected adolescents - a longitudinal study in real life. PLoS One. 2016; 11(9):e0163691. PMID:
27685782.

17. Saadah OI, Sindi HH, Bin-Talib Y, Al-Harthi S, Al-Mughales J. Entecavir treatment of children 2–16 years of age with chronic hepatitis B infection. Arab J Gastroenterol. 2012; 13(2):41–44. PMID:
22980589.
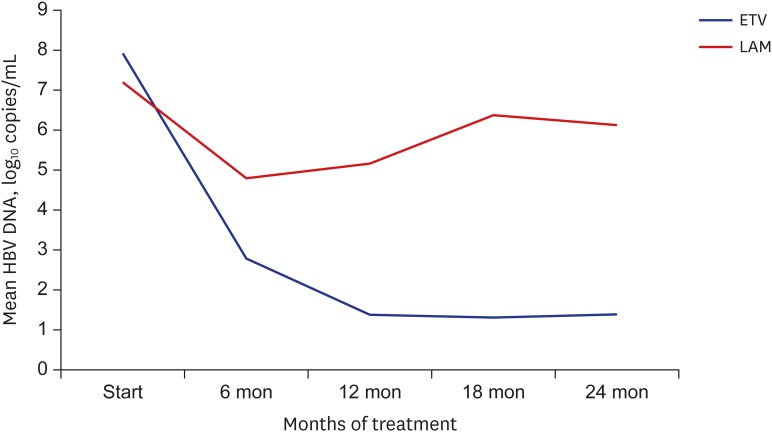
18. Pawłowska M, Halota W, Smukalska E, Woźniakowska-Gęsicka T, Kupś J. HBV DNA suppression during entecavir treatment in previously treated children with chronic hepatitis B. Eur J Clin Microbiol Infect Dis. 2012; 31(4):571–574. PMID:
21796345.

19. Luo J, Li X, Wu Y, Lin G, Pang Y, Zhang X, et al. Efficacy of entecavir treatment for up to 5 years in nucleos(t)ide-naïve chronic hepatitis B patients in real life. Int J Med Sci. 2013; 10(4):427–433. PMID:
23471472.

20. Sokal EM, Kelly DA, Mizerski J, Badia IB, Areias JA, Schwarz KB, et al. Long-term lamivudine therapy for children with HBeAg-positive chronic hepatitis B. Hepatology. 2006; 43(2):225–232. PMID:
16440364.

21. Jonas MM, Mizerski J, Badia IB, Areias JA, Schwarz KB, Little NR, et al. Clinical trial of lamivudine in children with chronic hepatitis B. N Engl J Med. 2002; 346(22):1706–1713. PMID:
12037150.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download