INTRODUCTION
‘Percutaneous osteoplasty (POP),’ cementoplasty, was defined as ‘the injection of bone cements into bone to treat bone lesions’ in 2012 in the medical subject headings of the United States National Library of Medicine. If ‘plasty’ is used as a suffix, it means that the body part described in the first part of the word is molded or shaped in order to restore its form or function in the body, such as rhinoplasty or mammoplasty. However, cementoplasty is an awkward and inappropriate nomenclature, because it is not used to mold or shape the cement. Therefore, it is more reasonable to use the term ‘osteoplasty’ just like vertebroplasty.
After percutaneous vertebroplasty (PVP) was first introduced for the treatment of painful angioma in 1987,
1 it has been widely used for osteoporotic compression fractures, metastatic osteolytic compression fractures, and multiple myelomas. The mechanisms of pain relief are the augmentation and chemical/thermal denervation of ingrown nerves into the vertebral body.
2 Using the same mechanism of pain relief as in the PVP of the vertebral body, POP is also useful to treat various painful metastatic bone lesions in the whole body.
PVP is performed on the body of the vertebra, a kind of irregular bone, according to its shape; POP can be performed on various shapes of bones, such as flat bones and the heads of long bones.
3 Although the most frequent site of bony metastasis is known to be the spine and vertebroplasty is commonly performed in painful osteolytic or osteoblastic metastatic vertebral compression fractures, the treatment for painful extraspinal bony metastasis is also a novel, veiled, challenging field of palliative care.
This retrospective study explored the efficacy and complications of extraspinal POPs.
METHODS
Study design
This observational retrospective study reviewed medical records of patients who had received POPs from 2009 to 2015. An informed consent about potential complications related to POP, including generalized complications such as nerve injury, bleeding, and wound infection, and specialized complications such as pneumothorax or hemothorax according to each procedure, had already been obtained.
Setting and participants
Inclusion criteria for POP were a history of pain in a dependent position, local tenderness or rebound tenderness on physical examination, and corresponding radiologic images including plain films, computed tomography, and bone scans.
The principle approaches for the POPs were chosen as the shortest distance to the targeted osteolytic lesion, while preventing nerve or vessel damage. The needle was chosen by the thickness and depth of the targeted bony structures: an 11-gauge, 10-cm long needle for the scapula, humeral head, greater or lesser trochanter of the femur, ilium, and ischium; a 13-gauge, 5-cm needle for the rib and sternum.
According to the targeted lesion, patients were placed in a prone, supine, or lateral decubitus position in order to expose the targeted structures. Before infiltration of local anesthetic, 30 mg of ketorolac and 50 μg of fentanyl were given intravenously. After aseptic draping, an outline of the bone and anticipated needle pathway to the target structure were drawn on the skin. Major vessels and nerves should be avoided during the needle approach to prevent damage. Five to 10 mL of 1% lidocaine was infiltrated into the targeted periosteum using a 3- or 5-cm long, 26-gauge needle.
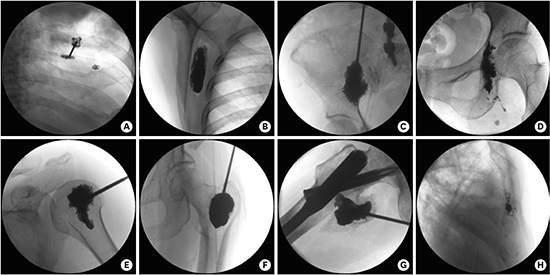
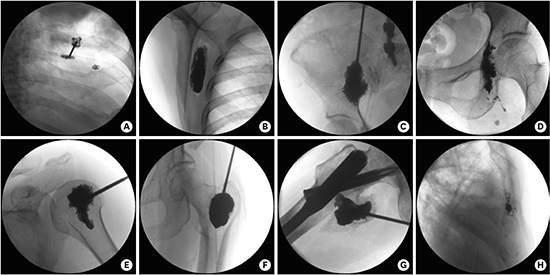
A 10-cm long, 11-gauge or 5-cm long, 13-gauge vertebral biopsy needle was inserted by manual force and anchored using a hammer. While advancing the vertebral needle into the bone, progress should be observed and compared using various fluoroscopic views. After the needle reached the targeted painful point, contrast medium was injected to observe the shape of its spread in the bone and any leakage into the vessels. If there was any leakage, a slice of gelatin sponge was inserted into the needle using 2 mL of 1% lidocaine in order to produce gelatin embolization. Then, contrast medium was reinjected to check whether the embolization was successful. Different volumes of bone cement were inserted into the needle for different bones using a manual injector (
Fig. 1).
 | Fig. 1Percutaneous osteoplasties. 
|
Palpation was checked to determine whether the painful tenderness had disappeared immediately after the POP procedure. After waiting 2 hours to allow the cement to harden, patients were allowed to move freely. Three-dimensional computed tomography was taken to determine whether the cement had been inserted into the targeted site after the POP.
Costoplasty
For the costoplasty, the posterior and anterior intercostal arteries, posterior and anterior intercostal veins, and intercostal nerves should be avoided, due to the danger of piercing them. However, if a 5-cm long, 13-gauge needle is inserted perpendicularly to the surface of the rib, these risks can be avoided. After the sensation of touching the outer convex cortex of the rib shaft with its slippery and smooth surface, the needle should be placed into the medulla, without penetrating the inner cortex. It was also important to choose a short-beveled stylet, because it is less likely to inadvertently penetrate the inner cortex. The needle should also be of a short length, which is easier to control.
The ribs can be divided into true (from the first to seventh) and false (eighth to twelfth) ribs, according to whether or not they are attached to the sternum. The last 2 pairs of ribs terminate freely between the muscles of the lateral abdominal wall, so we call them floating ribs.
4 It should be considered that the rebounding sensation to the needle is quite different between the anterior and posterior ribs, and between the true and false or floating ribs.
The needle should be anchored and advanced, while rotating and adjusting the C-arm fluoroscope from the true anteroposterior view to the oblique or lateral view, in order to observe the thickness of the targeted rib. It is difficult for the needle to anchor to the outer cortex of the rib due to its waxy surface, and sometimes hammering may be necessary in order to be successful.
Scapuloplasty
When performing a scapuloplasty, it was important to decide the anchoring and approach of the needle to the targeted osteolytic scapular body from imaging studies, matched with tenderness on physical examination. A 10-cm long, 11-gauge needle was suitable in most cases.
The medial or lateral border was selected as an anchoring point, because the suprascapular nerve and artery traverse through the scapula notch on the superior border. More specifically, the suprascapular nerve passes below the superior transverse scapular ligament, while the suprascapular artery passes over it.
The suprascapular nerve, originating from the union of the ventral rami of the C5 and C6 cervical nerves, is a mixed peripheral nerve. It contains motor innervation for the suprascapular and infrascapular muscles, and sensory innervation for the acromioclavicular and glenohumeral joints.
2
The suprascapular artery is the first (lower) branch of the thyrocervical trunk, and creates an anastomotic network with the dorsal scapular artery in order to supply the suprascapular and infrascapular muscles at the dorsal scapula.
5
Ilioplasty
The entry point for ilioplasty was usually selected on the iliac crest between the anterior superior iliac spine and posterior superior iliac spine, but closer to the latter. There is no important blood or nerve supply on the iliac crest. It can be a palpable bony prominence in a prone position.
It was easier to handle the needle, from anchoring it on the iliac crest to advancing into the iliac wing, body, and upper acetabulum, if both anterior superior iliac spines are supported by a pillow. If the acetabular involvement of the iliac bone was found (the upper part of the acetabulum is involved), a longer needle over 10 cm was needed.
Ischioplasty
The patient was placed in a prone position. The needle was inserted from the right ischial tuberosity through the ramus to the body. After confirmation of no leakage of the contrast medium into the vessel, the cement was inserted into the ischial body, ramus, and tuberosity, in a reserve order, while retracting the needle.
The ischium, the posteroinferior part of the hip bone, is composed of a body with a superior and an inferior ramus. The ischial tuberosity bears the weight of the body when sitting, therefore, metastatic osteolytic lesions in this area may aggravate pain in a sitting position, compared with standing or lying on the back. After anchoring in the ischial tuberosity, the needle was usually advanced to the superior ramus toward the posteroinferior acetabulum in a prone position.
Humeroplasty and femoroplasty
A long bone consists of a shaft with a proximal and a distal end. Bony metastasis was commonly found in the humeral or femoral head, rather than the shaft. The humeral head was more suitable for performing osteoplasty than the femoral head because it bears less weight.
6
The humeral head receives blood supply from the anterior and posterior humeral circumflex artery with the arcuate artery originating from the axillary artery. The tendon of the long head of the biceps brachii, originating from the supra-glenoid tubercle, runs between the lesser and greater tubercle. Caution should be paid not to penetrate these structures.
The femoral head and neck received blood supply from medial and lateral circumflex femoral arteries originating from deep artery of the thigh, which is a branch of the femoral artery from the external iliac artery. The femoral nerve innervates the femoral head and neck.
Osteoplasty in a femoral head alone without intramedullary nailing is not recommended, even though anatomic or surgical neck fractures do not seem to exist. It was safe to perform osteoplasty for painful metastasis in the greater or lesser trochanter after intramedullary nailing.
Sternoplasty
Sternoplasty was usually the final procedure in multiple metastatic patients who have already received vertebroplasty, costoplasty, and scapuloplasty at the same or adjacent level. Patients with pain due to metastasis to the sternum complained of anterior chest pain at every respiration. The body of the sternum, rather than the manubrium or xiphoid process, was the most frequent painful metastatic part. The costal cartilages from the 2nd to the 7th ribs attach to the body of the sternum.
A 5-cm, 13-gauge needle was appropriate to perform a sternoplasty perpendicular to the anterior surface of the sternal body. The outline of the sternum was unapparent in an anteroposterior fluoroscopic view. Therefore, it was better to draw an outline of the sternal body while palpating the space between the costal cartilages. It was important to anchor the needle under a lateral fluoroscopic view because the anchoring was the first and final step of sternoplasty just as in costoplasty.
Variables, data sources/measurement, bias, and study size
The origin of the cancer metastasis, performed POP sites, coexisting sites of bony metastasis determined by bone scans, necessity of adjacent joint injections, pain measurement at the POP site (visual analogue scale [VAS] from 0 to 10) before and 1 week after POP, Karnofsky Performance Scale (KPS, 0%–100%)
7 before and 1 week after POP, complications related to the POPs, and life expectancy (days) after POP were evaluated from the medical records.
Statistical methods
Demographic data include age, sex, total numbers of the origins of the cancer metastasis, performed POP sites, coexisting sites of bony metastasis determined by bone scans, and necessity of adjacent joint injections.
Changes in the VAS score before and 1 day after POP and in the KPS before and 1 week after POP were expressed as a mean ± standard deviation (SD) or median and interquartile range (IQR). The scores before and after POP were analyzed with paired t-test or Wilcoxon signed-rank test depending on the result of Shapiro-Wilk normality test. P value less than 0.05 was considered statistically significant. The statistical analyses were performed using SPSS 12.0 (IBM Corporation, Somers, NY, USA).
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Pusan National University Hospital (clinical trial number: 05-2016-159). Informed consent was waived by the board because of retrospective nature of this study.
RESULTS
Participants
A total of 47 (M/F = 28/19) patients, aged 35 to 87, had received 55 POPs from 2009 to 2016.
Mean age of total patients was 60.9 ± 11.1 years old. Mean age by sex (M/F) were 64.5 ± 6.3 and 55.2 ± 14.3 years old. According to the origin of the cancer metastasis, mean age was 60.8 ± 8.6 in 29 cases of lung cancer, 68.6 ± 9.2 in 7 cases of liver cancer, 45.8 ± 8.1 in 5 cases of breast cancer, 51.0 ± 15.7 in 4 cases of colon cancer, and 68.5 ± 13.4 in 2 cases of kidney cancer. Other cancers developed from only 1 case each: a 68-year-old with esophagus cancer, a 66-year-old with gall bladder cancer, a 62-year-old with stomach cancer, a 72-year-old with prostate cancer, a 55-year-old with sarcoma, a 71-year-old with ureter cancer, and a 79-year-old with a metastasis of unknown origin.
According to performed POP sites, mean age was 64.3 ± 10.2 in 19 cases of the rib, 60.3 ± 6.6 in 11 cases of the scapula, 58.3 ± 17.3 in 9 cases of the ilium, 58.5 ± 10.4 in 8 cases of the humeral head, 57.7 ± 9.5 in 3 cases of the ischium, 70.0 ± 4.2 in 2 cases of the femur, and 48.0 ± 1.4 in 2 cases of the sternum, respectively.
Data and main results
The most common sites for the origin of the cancer, in order of frequency, were the lung, liver, breast, colon, and kidney. The most frequently performed sites were the rib, scapula, ilium, humeral head, ischium, femur, and sternum, in that order. Costoplasties and scapuloplasties were performed in patients with lung cancer.
All POP cases revealed multiple bony metastases over 3 different structures on whole bone scans. All patients receiving POPs, excluding costoplasty and ischioplasty, needed adjacent joint injections before or after POPs.
Efficacy
The median VAS score for pain measurement decreased from 7.8 ± 1.8 to 2.8 ± 0.8 one day after the POPs (P < 0.05). The median KPS score increased from 35.4% ± 9.9% to 67.7% ± 11.1% one week after the POPs (P < 0.05). The mean life expectancy after performing POPs, for patients which died afterwards (35/46), was 99.3 ± 161.2 days, ranging from 1 to 767 days. Pain due to metastatic lesions was reduced significantly immediately after the POPs and sustained until the end of the patients' lives.
Complications
There were no complications related to the procedures.
DISCUSSION
Even though pain in the isolated POP sites may be difficult to measure due to overlapping systemic pain, the POPs provided immediate pain relief and better physical performance results in patients with painful bony metastasis when the patient changed positions or moved into a dependent position. No complications related to the POPs were found. The most common origins of the cancer were the lung, liver, breast, and colon: the extraspinal POPs were most frequently performed on the rib, scapula, ilium, and humeral head.
Localized metastatic pain decreased from the severe to mild pain ranges. Physical performance increased from the status of severely disabled (30%, which indicates hospital admission) or disabled (40%, requiring special care and assistance) to the status of requiring occasional assistance (60%, capable of care for most of their personal needs by themselves) or caring for themselves (70%, inability to carry on normal activity or do their work).
7
The meaningful data in this study was the mean life expectancy after POPs. Seventy-six percent of patients had lived over 2 months (which was the mean length) after POPs. However, an 87-year-old patient who had received the costoplasty due to metastasis from hepatocellular carcinoma died on the first day after the procedure because of an episode of uncontrolled acute esophageal variceal bleeding. Controversies surrounding the timing of POPs and the patients' general condition and life expectancy may arise.
8
It is at least certain that no analgesic can replace the role of POPs, relating to the relief of persistent and incidental breakthrough pain originating from bony metastasis. In addition, physical performance in ordinary life, such as coughing, sleeping, voiding, defecation, and walking, is also improved. There is no comparative study for proving an increased life span after POPs. POP, a minimally invasive procedure, can be performed within 30 minutes, under local anesthesia or monitored anesthetic care without the risk of complications related to the procedure.
There is no consensus on what the adequate filling volume for various bones are in POPs. For PVPs, 15% of the volume of the medulla in the vertebral body is enough to have adequate support strength and stiffness.
9 The mechanisms of pain relief from PVP are known to be augmentation and the chemical/thermal neurolysis of ingrown nerves.
10111213 Therefore, it is not necessary to completely fill the osteolytic lesions with bone cement.
There were sensational articles which claimed that use of augmentation using PVP was unnecessary.
1415 The results of PVP, or of only inserting the vertebral needle (sham operation), were sometimes similar in the short term. However, decompression, removing the air in the vertebral body, may result in pain relief due to reducing the irritation of the ingrown nerves under weight-bearing conditions, which also takes place during augmentation with bone cement.
Injections in adjacent joints, before and after the procedures, were necessary when performing POPs on the humeral head, femoral trochanter, scapula, and ilium. The reasons for performing facet joint injections prior to PVP are: 1) the injected bone cement obscures the facet joint under the fluoroscope; 2) patients can lie on their back during the PVP after removing adjacent facet joint pain; and 3) it is easier to identify the exact painful vertebrae among multiple collapsed osteoporotic or osteolytic compression fractures.
1213 The necessity of adjacent joint injections before POPs does not seem that different from that of adjacent facet joint injections before PVPs. But facet joint injections are also necessary because the compressed vertebra, the anterior structure, creates a greater load on the facet joints, the posterior element of the spine. In contrast, long-term immobilization of the shoulder or hip joint due to metastatic bone pain may cause joint fibrosis, producing another source of pain and limitation of motion in the joint, which may be relieved by adjacent joint injections.
POP under C-arm fluoroscopic guidance is a familiar method. If the understanding of the anatomy of the targeted bone, such as its curvature and thickness, is not sufficient, it is helpful to perform the POP while observing a skeleton model. Another option is to use a real-time, intraoperative 2- or 3-dimensional imaging system (O-arm® surgical imaging system; Medtronic, Minneapolis, MN, USA). The system provides intraoperative computed tomographic views in a familiar operating room; however, it produces a limited, round field for operation with its relative bulk, and also interrupts the operation, due to the need to evacuate from the radiation hazard while studying the 3-dimensional images, which may increase procedural time.
In our experience, there were some precautions needed when inserting the needle into the targeted bone to avoid predicted complications. First of all, the most important thing was to choose a needle with a cannula of the appropriate thickness and length, and a stylet with a suitable bevel length, in order to avoid penetrating, or not reaching, the targeted area. Second, it was also important to avoid the major vessels and nerves. Third, it was better to choose the shortest available route to the targeted bone which could reduce pain and time.
Despite good results, this was a retrospective study without a control group and the number of patients was small. A prospective study with a larger number of patients is required while comparing the results with those of sham operations, however the latter would widely be considered inhumane.
Metastatic extraspinal bone pain presents as movement-related incidental breakthrough pain (when it is increasing in a dependent position) and constant continuous pain.
3 POPs provided reliable pain relief for localized metastatic bone pain which cannot be reduced by opioid or non-opioid analgesics. In addition, POPs also produced better physical performance. There were no complications related to the procedures. The mean life expectancy after performing the POPs was over 2 months. Therefore, POPs like PVPs, were minimally invasive procedures with a minimal risk, and provided immediate pain relief and increased physical performance.
The most common sites for the origin of the cancer, in order of frequency, were the lung, liver, breast, colon, and kidney.
16 The most frequently performed sites were the rib, scapula, ilium, humeral head, ischium, femur, and sternum, in that order. Adjacent joint injections were necessary prior to the POPs.
17
Basically, it is essential for operators to understand the shape, curvature, and thickness of the metastasized flat or long bone, exact location of the painful metastasized bone, and important vascular and nervous supplies in the pathway of needle approach.