Abstract
Electronic cigarettes (ECs) are a device that aerosolize liquid nicotine by heating a solution of nicotine, glycerol and flavoring agents. The awareness and the usage of ECs has increased in many countries. Due to the online sales and the absence of EC regulations, the prevalence of EC usage is especially high in adolescents and young adults. Due to the large amount and the high nicotine concentration of EC liquid, the ingestion for suicide can lead to cardiac death. We had two patients, a 27-year-old male who ingested about 23 mg/kg of nicotine and a 17-year-old female who ingested about 30 mg/kg of nicotine. Both patients presented seizure-like movement and cardiac arrest. They had metabolic acidosis and transient cardiomyopathy. They were ultimately discharged with a cerebral performance category of 2 and 4, respectively. Increasing EC use may produce more cases of medical problems or suicide by nicotine intoxication.
Go to : 
Graphical Abstract
Go to : 
Electronic nicotine delivery systems or electronic cigarettes (ECs) are devices that aerosolize liquid nicotine by heating a solution of nicotine, glycerol, and flavoring agents.1 There has been an increase in awareness and the usage of EC in many countries.123 Moreover, the prevalence of EC usage in adolescents and young adults has been reported to be higher than in older adults.123 The online sales and improper regulations of EC have an impact on the increment of EC usage, especially in young adults.1456 Without the common regulations of EC, the products on sale have varied levels of nicotine concentration labeled on their packages across several countries.4
With an increase in EC usage, there has been an augmentation in concerns about the toxic exposures to nicotine.67 In adults, 0.7% of exposures were intentional to commit suicide.6 Two cases of death have been reported due to consumption of electrical cigarette liquid (EC liquid).67
We present case reports of two patients with cardiac arrest resulting from the ingestion of EC liquid with an attempt to commit suicide.
Go to : 
A 27-year-old male was admitted to the emergency room (ER) with return of spontaneous circulation (ROSC) after cardiac arrest on 27 December 2015. He bought 10 bottles of EC liquid 3 hours before arrival to the ER. He was found showing seizure-like movements. At the scene, a disposable cup with brownish liquid and a suicide note were found. At the arrival of paramedics, he was found pulseless with the first-monitored rhythm as asystole. Cardiopulmonary resuscitation (CPR) was provided for 13 minutes until ROSC. The brand names of the EC liquid were DIY Flavor Shack® with a nicotine concentration of 16 mg/mL and Halo® with a nicotine concentration of 18 mg/mL. The actual amount of consumption was not detected.
At the time of arrival to ER, the vital signs were as follows: blood pressure (BP) 105/57 mmHg, pulse rate (PR) 111 beats per minute (bpm), respiratory rate (RR) 19 bpm, and body temperature (BT) 34.5°C. He was comatose with fixed pupil size of 3 mm. For post-cardiac arrest care, targeted temperature management (TTM) with 33°C was started. Activated charcoal was given via levin tube and continuous venovenous hemodiafiltration (CVVHDF) was started. Initial laboratory tests were not notable. The results included the following: pH 7.154, PCO2 47.3 mmHg, PO2 497.6 mmHg, FiO2 100%, base deficit 12.4 mmol/L, HCO3 316.3 mmol/L, SaO2 99.8%, lactic acid 9.30 mmol/L, creatine kinase (CK) 140 U/L, creatine kinase-myocardial band (CK-MB) 1.0 µg/L, high-sensitivity troponin I 0.031 ng/mL (at 3rd day of admission, high-sensitivity troponin I 4.097 ng/mL), S100 0.218 µg/L (at 2nd day of admission, 0.060 µg/L), and serum ethanol 164.56 mg/dL. The level of plasma nicotine was not measured due to the limitation of the facility's capacity.
Electrocardiography (ECG) showed sinus tachycardia with a rate of 110 bpm and ST segment depression in leads V4 to V6. Echocardiography showed decreased left ventricular (LV) systolic function with an ejection fraction (EF) of 35% and regional wall motion abnormalities (RWMAs) at the mid and proximal left ventricle. On the 5th day of admission, echocardiography showed the systolic function with EF 58% and the full recovery of RWMAs.
After 24-hour TTM, he was alert and aware. He did not remember events during the previous two months. Brain magnetic resonance imaging (MRI) showed bilateral hippocampal disruption. Amnesia was recovered on the 9th day of admission. On the 6th day of admission, he had involuntary myoclonic movement of all the extremities without any changes in brain MRI. On the 13th day of admission, he was discharged to home with a cerebral performance category (CPC) of 2.
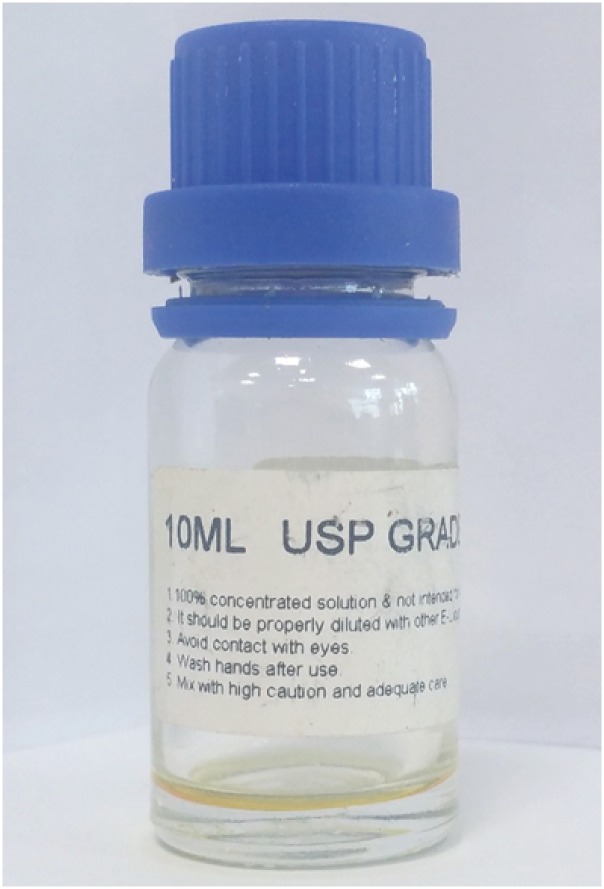
A 17-year-old female was admitted to ER with cardiac arrest on 12 April 2016. She had ingested 10 mL EC liquid named ‘Pure Nicotine®’ with a nicotine concentration of 210 mg/mL (Fig. 1). She showed generalized tonic clonic movement for 5 minutes. After fifteen minutes, paramedics arrived and recognized that she was unresponsive with a pulse and fully dilated pupils. As arrest with the rhythm of asystole was noted during transportation, CPR was performed for 8 minutes.
After ROSC, the vital signs were as follows: BP 60–34 mmHg, PR 116 bpm, RR 26 bpm, and BT 35.3°C. She was comatose with a fixed pupil size of 3 mm. Activated charcoal was given via levin tube and CVVHDF was done for 2 days. For post-cardiac arrest care, TTM with 36°C was started. Initial laboratory tests were not notable. The results included the following values: pH 6.881, PCO2 65.9 mmHg, PO2 439.1 mmHg, FiO2 100%, base deficit 22.0 mmol/L, HCO3 12.1 mmol/L, SaO2 99.6%, lactic acid 14.3 mmol/L, CK 54 U/L, CK-MB 0.3 µg/L, high-sensitivity troponin I 0.007 ng/mL (at 3rd day of admission, high-sensitivity troponin I 0.427 ng/mL), and S100 0.700 µg/L (at 2nd day of admission, 0.520 µg/L). The level of plasma nicotine was also not measured.
Initial ECG showed sinus tachycardia with a rate of 109 bpm. Echocardiography showed decreased LV systolic function with an EF of 48% and RWMAs at the mid left ventricle. On the 17th day of admission, echocardiography showed the systolic function with an EF of 69% and the full recovery of RWMAs.
After 24-hour TTM, rewarming was done to 36.5°C, she was semicomatose without awareness. Somatosensory evoked potential on the 4th day of admission showed bilateral absence of N20 on median nerve. Generalized myoclonic movement was noted. Electroencephalogram on the 4th day of admission showed generalized suppression without seizure. Although spontaneous eye opening was noted, neither awareness nor intentional movement was noted. On the 32nd day of admission, she was transferred to a rehabilitation facility with a CPC of 4.
Go to : 
In the present study, we presented two cases with cardiac arrest resulting from intentional ingestion of EC liquid, which are the first reports in Korea. The latter patient was the first adolescent to date with an attempt of committing suicide by ingestion of EC liquid.
The intoxication caused by nicotine from EC liquid is reported to have only minor effects.6 Over 20% of exposure showed no symptoms and common symptoms were vomiting, nausea, ocular irritation, and dizziness.6 Unintentional exposures and adverse reactions were included in a previous study, which accounted for about 92% among the total exposures.6 Intentional exposures with suicidal ideation accounted for 12 cases.6 In cases of intentional exposures, a large amount of EC liquid leads to cardiac arrest.7 There were two fatal cases leading to death.67 In both the cases, exposure to EC liquid led to seizure and cardiac arrest.67 In our cases, intentional ingestion led to seizures, myocardial dysfunctions, and cardiac arrests. As the LD50 for nicotine in humans is 1 mg/kg, doses in our cases exceeded the lethal dose.8
According to a previous research study, the most common age group of exposure to EC was children under 5 years of age.6 The next common group was adults aged between 20–39 years.6 The prevalence of EC usage in young adults (20–28 years) was higher than in older adults (more than 45 years).1 The advertisements and the sales of EC are easily accessible online, which create more opportunities for young adults to come in contact with it.1 Adolescents have similar opportunities like young adults to come in contact with EC via the internet.12 Furthermore, the tendency to seek new experiences has an influence on exposure to EC in adolescents.1 It is hypothesized that with an increase in exposure to EC in adolescents, intentional ingestion of EC liquid for suicide might also increase. Our case is the first report to describe the ingestion of EC liquid with an attempt to commit suicide in adolescents.
In previous studies, the necessity for regulations of EC liquid has been presented.2345 The majority of the products have their own concentration of nicotine and the amount is detailed on the package.45 However, in many products, the label shows inaccurate information about the amount and the concentration of nicotine.45 For these reasons, the Unites States Food and Drug Administration made regulations about the product approval, warning labels and packaging requirements.9 However, there are no regulations about the labels and packaging requirements in Korea.5 A product named ‘Pure Nicotine®’ is on sale in Korea and has been mentioned in previous studies because of the high concentration of nicotine (Fig. 1).45 The label indicates a nicotine concentration of 210 mg/mL; however, the concentration was actually determined to be 150 mg/mL in this product.4 Compared to other products that have a nicotine concentration between 0 to 36 mg/mL, the amount of nicotine in ‘Pure Nicotine®’ is significantly high and usage via inhalation without dilution can cause adverse effects.4 In our case, one of the patients was exposed to 10 mL of ‘Pure Nicotine®,’ which led to cardiac arrest.
With an increase in EC usage and the absence of proper regulation for EC liquid, the concerns about the toxic exposure have also increased.5 The presented cases caution that the ingestion of EC liquid can be one of the emerging methods for suicide, especially in young adults and adolescents.
Go to : 
Notes
Author Contributions: Investigation: Park EJ. Writing - original draft: Park EJ, Min YG. Writing - review & editing: Min YG.
Go to : 
References
1. Lee JA, Kim SH, Cho HJ. Electronic cigarette use among Korean adults. Int J Public Health. 2016; 61(2):151–157. PMID: 26564162.

2. Lee S, Grana RA, Glantz SA. Electronic cigarette use among Korean adolescents: a cross-sectional study of market penetration, dual use, and relationship to quit attempts and former smoking. J Adolesc Health. 2014; 54(6):684–690. PMID: 24274973.

3. Schoenborn CA, Gindi RM. Electronic cigarette use among adults: United States, 2014. NCHS Data Brief. 2015; (217):1–8.
4. Goniewicz ML, Gupta R, Lee YH, Reinhardt S, Kim S, Kim B, et al. Nicotine levels in electronic cigarette refill solutions: a comparative analysis of products from the U.S., Korea, and Poland. Int J Drug Policy. 2015; 26(6):583–588. PMID: 25724267.

5. Kim S, Goniewicz ML, Yu S, Kim B, Gupta R. Variations in label information and nicotine levels in electronic cigarette refill liquids in South Korea: regulation challenges. Int J Environ Res Public Health. 2015; 12(5):4859–4868. PMID: 25950652.
6. Vakkalanka JP, Hardison LS Jr, Holstege CP. Epidemiological trends in electronic cigarette exposures reported to U.S. Poison Centers. Clin Toxicol (Phila). 2014; 52(5):542–548. PMID: 24792781.

7. Chen BC, Bright SB, Trivedi AR, Valento M. Death following intentional ingestion of e-liquid. Clin Toxicol (Phila). 2015; 53(9):914–916. PMID: 26457570.

8. Soghoian S. Nicotine. In : Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, editors. Goldfrank's Toxicologic Emergencies. 9th ed. New York, NY: McGraw-Hill Medical;2011. p. 1187–90.
9. FDA proposes to extend its tobacco authority to additional tobacco products, including e-cigarettes. Accessed April 24,2014. https://wayback.archive-it.org/7993/20170112124812/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm394667.htm.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download