This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Stroke is the number one cause of adulthood disability in Korea. Rehabilitation after stroke can minimize functional disability, enhance recovery toward independence, and optimize community reintegration. The inter-departmental stroke meeting (IDSM) is a potential method to improve rehabilitation outcomes in patients with stroke. We aimed to analyze the effect of IDSM on rehabilitation after acute ischemic stroke management.
Methods
Medical records of 753 patients with acute ischemic stroke admitted to the neurology department of our medical center between January and December 2014 were reviewed retrospectively. In May 2014, weekly IDSMs were initiated. All physicians responsible for the patient's care reviewed patient treatment, methods of secondary prevention, and future rehabilitation plans.
Results
The transfer rate significantly increased after initiation of IDSM (phase 2, 3) and the length of stay (LOS) before transfer to the rehabilitation department decreased significantly from 9.68 ± 8.50 days to 5.75 ± 2.12 days. There was a reduction in the total LOS from 52 ± 28.57 days to 35 ± 27.21 days after IDSMs were introduced. In non-transferred patients also, the total LOS reduced significantly. The transfer rate increased significantly and the LOS before transfer to the rehabilitation department decreased significantly after implementation of IDSM in a subgroup of patients with moderate to severe stroke.
Conclusion
The introduction of IDSM was significantly correlated with improvements in transfer rates and reduction of LOS in hospital. This finding shows that IDSMs are an important intervention to improve therapeutic progress and outcomes for patients with stroke.
Keywords: Stroke, Cerebrovascular Disease, Rehabilitation, Communication
INTRODUCTION
Stroke is the third leading cause of death and a primary cause of long-term disability in Korea, with more than 60% of surviving stroke patients burdened with residual neurologic deficits.
1 Rehabilitation for patients with stroke has a positive effect on the minimization of functional disabilities, as well as promoting an earlier return to independence and normal life. In addition, studies of the initiation of early rehabilitation treatment have reported better effects on the enhancement of muscle strength and recovery of physical functions in patients with stroke.
2 Thus, how promptly and frequently rehabilitation treatment can be provided to patients with stroke is a very important consideration for clinicians.
3 The decision to initiate rehabilitation after stroke depends on many factors, including patient status, availability of services, and clinician preferences; furthermore, evidence links greater adherence to published practice guidelines with improved functional outcomes.
1 The selection of inpatients for rehabilitation and the timing of transfer from acute care are important clinical decisions that impact quality of care and patient flow.
4
Severe stroke, characterized by various clinical symptoms, requires a multidisciplinary approach.
5 Although not all patients with stroke need rehabilitation, there is still a range of barriers to sufficient rehabilitation for patients who need prompt treatment at specific times, and this influences the prognosis of patients. Hence, we used the inter-departmental stroke meeting (IDSM) as a method to improve rehabilitation treatment of patients. Currently, there are very few studies on effective methods and tools to administer rehabilitation treatment to patients with stroke. Thus, we evaluated the effectiveness of IDSMs for the management of patients with stroke by comparing transfer rates and length of stay (LOS) before and after initiation of IDSMs at our hospital.
METHODS
Subjects
Medical records of patients with acute ischemic stroke admitted to the neurology (NR) department of our medical center, which is equipped with emergency care facilities, between January 2014 and December 2014 were reviewed retrospectively. A total of 753 patients hospitalized during this period were included. Patients were classified into 3 groups: those admitted between January 2014 and April 2014 (phase 1), those admitted between May 2014 and August 2014 (phase 2), and those admitted between September 2014 and December 2014 (phase 3). Phase 1 patients did not have IDSMs and phase 2 and 3 patients did have IDSMs. Demographics and stroke-related characteristics included age, sex, level of education, socio-economic status, insurance, modified Ranking Scale (mRS), National Institute of Health Stroke Scale (NIHSS), brain lesion location (left, right, or both), stroke lesion site (cortical, subcortical, multiple, or infratentorial), and mortality.
IDSM
IDSMs were conducted for all patients hospitalized for acute ischemic stroke in the NR department of our hospital in phase 2 and 3. The IDSM agenda was proposed by neurologist and physiatrist, and neurologist led the meeting. IDSMs were held weekly from May 2014 for each patient with stroke. The IDSMs were performed very early phase (within 7 days) after the patient was admitted to the stroke unit with an acute ischemic stroke. During the study period, a total 753 patients were discussed and the meeting lasted for one hour. The meeting discussed not only the patient's pure medical issue, but also comprehensive patient care. During the meeting, all physicians involved in the patient's care, such as the neurologist, neurosurgeon and physiatrist participated in a review of the patient that included analysis of brain imaging studies, such as magnetic resonance images and computed tomography and the effectiveness of interventions (intravenous tissue plasminogen activator or intraarterial thrombectomy). The provision of medication for secondary prevention, patient prognosis, and future rehabilitation plans (early rehabilitation and transference to rehabilitation department) were also discussed. The most common issues with meeting were when to start the patient's early rehabilitation therapy, the discharge of patients who had mild sequela of stroke, or short-term rehabilitation therapy.
Outcome evaluation
In order to investigate the beneficial effect of IDSMs, we compared the transfer rate to rehabilitation medicine (RM), hospital LOS before transfer, RM LOS, total hospital LOS, and in hospital mortality for patients admitted during 3 phases: January 2014 to April 2014 (phase 1), May 2014 to August 2014 (phase 2), and September 2014 to December 2014 (phase 3). In addition, we compared the transfer rate to RM, hospital LOS before transfer, RM LOS, and total hospital LOS in patients with moderate to severe impairment (mRS score of 3–5). Hospital LOS before transfer was defined as the LOS in NR for acute management before being transferred to the RM department. Total hospital LOS was defined as the sum of the hospitalization period in NR plus the period of hospitalization in the RM department for comprehensive rehabilitation treatment. In addition, the mortality of all patients admitted to the NR for stroke was compared and analyzed for each period. There was no increase in neurologists or physiatrists, rehabilitation beds, physical therapists, or occupational therapists during the 3 phases period, and there was no change in policy or administration, reimbursement system, or introduction of hospital accreditation.
Statistical analysis
For data analysis, we used SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) for Windows. An analysis of variance (ANOVA) was used for numerical variables and a χ2 test or linear by linear association test for categorical variables to compare the transfer rate and LOS before and after the introduction of IDSMs. In addition, we compared the transfer rate and all LOS measurements in patients with moderate to severe impairment (e.g., mRS 3–5).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Chungnam National University College of Medicine (No. CNUH 2017-06-046). Informed consent was submitted by all subjects when they were enrolled.
RESULTS
Demographics
The mean age of patients was 69.99 ± 11.57 years and 58.2% were male. There were 249 (33.1%) patients admitted between January 2014 and April 2014, 261 (34.7%) patients between May 2014 and August 2014, and 243 (32.3%) patients between September 2014 and December 2014. There were no statistically significant differences between groups for demographics such as age, sex, level of education, socio-economic status, insurance, mRS, NIHSS, and mortality (
Table 1).
Table 1
Demographic and clinical characteristics

|
Parameters |
Total |
Phase 1 |
Phase 2 |
Phase 3 |
P value |
|
No. (% of male) |
753 (58.2) |
249 (57.4) |
261 (54.8) |
243 (62.6) |
0.469 |
|
Age at onset, yr |
69.9 (± 11.57) |
69.7 (± 11.61) |
71.1 (± 10.82) |
69.1 (± 12.23) |
0.416 |
|
Education |
|
|
|
|
0.488 |
|
≤ 12 year school age |
657 (87.3) |
214 (85.9) |
230 (88.1) |
213 (87.7) |
|
> 12 year school age |
96 (12.7) |
35 (14.1) |
31 (11.9) |
30 (12.3) |
|
Economy |
|
|
|
|
0.590 |
|
Low income |
497 (66.0) |
175 (70.3) |
171 (65.5) |
151 (62.1) |
|
Middle income |
236 (31.3) |
65 (26.1) |
84 (32.2) |
87 (35.8) |
|
High income |
20 (2.7) |
9 (3.6) |
6 (2.3) |
5 (2.1) |
|
Insurance |
|
|
|
|
|
|
% of NHS |
712 (94.6) |
231 (92.8) |
248 (95.0) |
233 (95.9) |
0.638 |
|
mRS at end of acute management |
1.93 (1.72) |
1.89 (1.62) |
2.03 (1.79) |
1.86 (1.75) |
0.520 |
|
Initial NIHSS |
3.96 (4.47) |
3.77 (4.14) |
4.00 (4.40) |
4.10 (4.86) |
0.690 |
|
Lesion locationa
|
|
|
|
|
< 0.001 |
|
Left |
292 (38.8) |
80 (32.1) |
108 (41.4) |
104 (42.8) |
|
Right |
293 (38.9) |
96 (38.6) |
87 (33.3) |
110 (45.3) |
|
Multifocal |
168 (22.3) |
73 (29.3) |
66 (25.3) |
29 (11.9) |
|
Lesion sitea
|
|
|
|
|
< 0.001 |
|
Cortical |
251 (33.3) |
61 (24.5) |
97 (37.2) |
93 (38.3) |
|
Subcortical |
205 (27.2) |
62 (24.9) |
74 (28.4) |
69 (28.4) |
|
Multiple |
186 (24.7) |
89 (35.7) |
49 (18.8) |
48 (19.8) |
|
Infratentorial |
111 (14.7) |
37 (14.9) |
41 (15.7) |
33 (13.6) |
|
Mortality during admission |
21 (2.8) |
6 (2.4) |
8 (3.1) |
7 (2.9) |
0.749 |
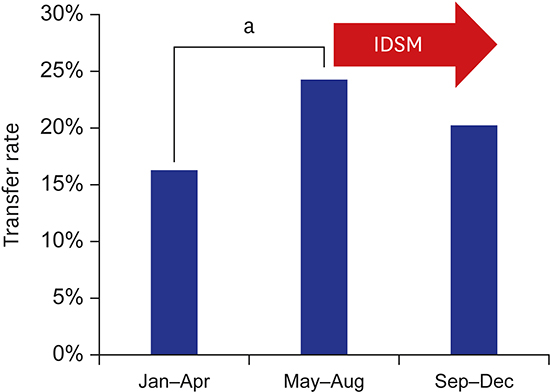
Transfer to the rehabilitation ward
The number of patients who were transferred to the rehabilitation ward was 152 (20.2%). Patients who had IDSMs had significantly higher transfer rates. The difference in transfer rate between phase 1 (16.1%) and phase 2 (24.5%) was statistically significant (
P = 0.035) (
Fig. 1). The difference in transfer rates between phase 2 (24.5%) and phase 3 (19.8%) was not significant (χ
2 test [
P = 0.198]). However, it does show that the higher transfer rates seen in phase 2 were maintained in phase 3.
Fig. 1
Characteristics of rehabilitative transfers in the tertiary hospital before and after implementation of IDSMs. The transfer rate to department of rehabilitation medicine increases after the initiation of IDSMs in phase 2 and this is maintained in phase 3.
IDSM = inter-departmental stroke meeting.
aP = 0.035 by χ2 test.

LOS before transfer, RM LOS, total LOS, and mortality during admission
The LOSs before transfer in transferred patients were 9.68 ± 8.50, 6.08 ± 3.34, and 5.75 ± 2.12 days in phase 1, 2, and 3, respectively. ANOVA for LOS before transfer showed a significant difference among groups (F = 8.28;
P < 0.001). The post hoc analysis using Bonferroni method between groups showed a significant decrease in LOS before transfer not only between phase 1 and 2 (
P = 0.001), but also phase 1 and 3 (
P = 0.001) (
Fig. 2). For total LOS there was reduction in LOS from 52 days to 35 days between phase 1 and phase 3 (
P = 0.035) (
Fig. 3). In contrast, a decrease in LOS within the entire hospital was not observed during the 3 phases. Total LOS in transferred patients in the 3 phases were 52.20 ± 28.57, 40.14 ± 27.73, and 35.35 ± 27.21 days, respectively. ANOVA for total LOS in transferred patients showed a significant difference among phases (F = 4.21;
P = 0.017). The post hoc analysis by Bonfferoni method showed a significant total LOS decrease between phase 1 and phase 3 (
P < 0.163). Total LOSs in non-transferred patients in the 3 phases were 6.78 ± 6.35, 6.07 ± 6.07, 5.28 ± 3.39 days, respectively. ANOVA for total LOS in non-transferred patients showed a significant difference among phases (F = 3.82;
P = 0.025). The post hoc analysis by Bonfferoni method showed a significant total LOS decrease between phase 1 and phase 3 (
P = 0.184). Although analysis of the differences in LOS after the transfer to the RM was not statistically significant, RM LOS did reduce from 43 to 30 days (
Fig. 4). The RM LOSs of transferred patients in the 3 phases were 42.53 ± 25.28, 34.06 ± 27.07, and 29.60 ± 27.35, respectively. ANOVA for RM LOS showed no significant difference (F = 2.61;
P = 0.781); however, there was trend towards a decrease in RM LOS. The mortality rates during admission in the 3 phases were 2.4%, 3.1%, and 2.9%, respectively and these differences were not significant (
P = 0.892).
Fig. 2
The LOS before transfer to the rehabilitation department. The LOS before transfer to the rehabilitation department decreases in phase 2 and phase 3 after the introduction of IDSMs. Values are expressed as mean ± standard deviation.
IDSM = inter-departmental stroke meeting, LOS = length of stay, ANOVA = analysis of variance.
aP = 0.035 by ANOVA followed by Tukey honestly significant difference.
Fig. 3
The total hospital LOS after the implementation of IDSMs. Total LOS decreases after the introduction of IDSMs regardless of transfer to rehabilitation ward. Red bars represent patients with stroke transferred to the rehabilitation ward. Blue bars represent patients with stroke who were not transferred. Sky blue bars represent the total population of patients admitted to our hospital. Values are expressed as mean ± standard deviation.
LOS = length of stay, IDSM = inter-departmental stroke meeting, ANOVA = analysis of variance.
aP = 0.035 by ANOVA.

Fig. 4
The transfer rate of patients with a mRS score of 3–5. Transfer rates significantly increase with increasing phase in patients with an mRS score of 3–5. However, no significant changes are seen in patients with an mRS score of 0–2.
mRS = modified Ranking Scale, ANOVA = analysis of variance.
aP = 0.035 by post hoc analysis between groups after ANOVA.

Subgroup analysis of patients with moderate to severe ischemic stroke (mRS 3–5)
In patients with moderate to severe stroke, transfer rates were significantly higher in phase 3 (48.1%) compared to phase 1 (39.5%) (P = 0.035). The transfer rates for phase 2 (42.3%) were significantly higher than transfer rates in phase 1 (39.5%) (P = 0.035). Furthermore, transfer rates were significantly higher in phase 3 (43.3%) than phase 2 (42.3%) (P = 0.035).
For patients with moderate to severe stroke, the LOSs before transfer were 10.43 ± 9.61, 6.39 ± 3.74, and 5.69 ± 2.20 days in phases 1, 2, and 3, respectively. Phase 2 LOSs before transfer were significantly shorter than in phase 1 (P = 0.035). Furthermore, phase 3 LOSs were significantly shorter than in phase 1 (P = 0.035).
DISCUSSION
This study showed that introduction of IDSMs had a significant and positive effect on the rehabilitation process of patients with stroke. The introduction of IDSMs significantly increased patient transfer rates to the rehabilitation department, and the hospitalization LOS before rehabilitation transfer was greatly reduced. The same trend was observed in phase 3 with continued IDSMs whereby LOS before transfer and total LOS were significantly reduced.
There are few studies on the effect of interdisciplinary meetings for the improvement of treatment quality.
6 Moreover, this study is the very first report to analyze the effect of multidisciplinary meetings on patients with stroke. One study conducted research on the effect of multidisciplinary team treatment on the management of cancer patients.
7 Although it is difficult to compare the results of cancer patients research with that of our study, Licitra et al.
7 studied the effect of multidisciplinary meetings during the rehabilitation process for patients with rheumatic arthritis and concluded that multidisciplinary team treatment had positive effects including reduction of cancer treatment time and improvement of outcomes. Another study by Verhoef et al.
8 studied the use of rehabilitation tools in multidisciplinary team meetings. They undertook direct research on multidisciplinary team meetings and concluded that the use of rehabilitation assessment tools had a positive effect in multidisciplinary meetings. Two other studies on interventions to improve communication in team meetings are also worthy of attention. One of these studies conducted research on the effect of introduction of structured team meeting forms and the nomination of a coordinator,
9 while the other studied the effect of training leaders of multidisciplinary teams.
10
Our study found that IDSMs enhanced transfer rates of patients with stroke to the rehabilitation department and reduced the rehabilitation time greatly. Thus, we conclude that there are many barriers such as consensus of patient and doctor opinions, provision of insufficient information on the necessity of rehabilitation treatment for patients, and the failure of doctors in other disciplines to recognize the necessity for rehabilitation and therefore not refer patients to RM. The IDSMs may be the very tool to solve these problems. Our study proved that implementation of IDSMs not only increase transfer rates but also significantly reduced the time taken for patients to be transferred to RM. Our study did not reveal any other factors influencing transfer rates and LOS reduction other than the application of IDSMs. Therefore, we think it reasonable to assume that this reduction in hospital LOS enabled early rehabilitation treatment of patients, which ultimately improved outcomes.
Even though this study demonstrated the positive effect of IDSMs on the treatment and management of patients with stroke, it had several limitations. First, the patient data analyzed before and after the implementation of IDSMs were for a relatively short period of only 1 year. Second, the analysis was conducted on the effect of IDSMs on transfer rate and LOS in a single hospital, which prevents the generalization of our findings to the general population. Third, as this study did not conduct long-term analysis of the functional outcomes of patients with stroke, future studies are required. Nevertheless, this study is significant in that it is the very first analysis on the effect of IDSMs on transfer rates and LOS in patients with stroke.
Clinicians are well aware that rehabilitation treatment for patients with acute ischemic stroke and functional disabilities enhance patient function and improve prognosis. This is the first study in Korea to show the effect of IDSMs on the provision of rehabilitation treatment to these patients. Our study suggests that IDSMs help rehabilitation treatment in these patients. In addition, we also demonstrated that the application of IDSMs reduces LOS. Further studies are required to assess the effect of IDSMs on long-term outcomes, such as functional ambulatory category, mRS, and activities of daily living.
ACKNOWLEDGMENTS
We thank the following coordinators of the Regional Comprehensive Stroke Centers for data collection (Hee Seon Yu, RN and Na Young Youn, RN).
References
1. Bates BE, Kwong PL, Xie D, Valimahomed A, Ripley DC, Kurichi JE, et al. Factors influencing receipt of early rehabilitation after stroke. Arch Phys Med Rehabil. 2013; 94(12):2349–2356.

2. Eakin MN, Ugbah L, Arnautovic T, Parker AM, Needham DM. Implementing and sustaining an early rehabilitation program in a medical intensive care unit: a qualitative analysis. J Crit Care. 2015; 30(4):698–704.

3. Lynch EA, Cumming T, Janssen H, Bernhardt J. Early mobilization after stroke: changes in clinical opinion despite an unchanging evidence base. J Stroke Cerebrovasc Dis. 2017; 26(1):1–6.

4. Poulos CJ, Magee C, Bashford G, Eagar K. Determining level of care appropriateness in the patient journey from acute care to rehabilitation. BMC Health Serv Res. 2011; 11(1):291.

5. Kim J, Hwang YH, Kim JT, Choi NC, Kang SY, Cha JK, et al. Establishment of government-initiated comprehensive stroke centers for acute ischemic stroke management in South Korea. Stroke. 2014; 45(8):2391–2396.

6. Verhoef J, Toussaint PJ, Putter H, Zwetsloot-Schonk JH, Vliet Vlieland TP. Pilot study of the development of a theory-based instrument to evaluate the communication process during multidisciplinary team conferences in rheumatology. Int J Med Inform. 2005; 74(10):783–790.

7. Licitra L, Keilholz U, Tahara M, Lin JC, Chomette P, Ceruse P, et al. Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral Oncol. 2016; 59:73–79.

8. Verhoef J, Toussaint PJ, Putter H, Zwetsloot-Schonk JH, Vliet Vlieland TP. The impact of the implementation of a rehabilitation tool on the contents of the communication during multidisciplinary team conferences in rheumatology. Int J Med Inform. 2007; 76(11-12):856–863.

9. Halstead LS, Rintala DH, Kanellos M, Griffin B, Higgins L, Rheinecker S, et al. The innovative rehabilitation team: an experiment in team building. Arch Phys Med Rehabil. 1986; 67(6):357–361.
10. Engström B. Communication and decision-making in a study of a multidisciplinary team conference with the registered nurse as conference chairman. Int J Nurs Stud. 1986; 23(4):299–314.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download