1. Tanner CM, Goldman SM. Epidemiology of Parkinson's disease. Neurol Clin. 1996; 14(2):317–335. PMID:
8827174.

2. Aarsland D, Larsen JP, Lim NG, Janvin C, Karlsen K, Tandberg E, et al. Range of neuropsychiatric disturbances in patients with Parkinson's disease. J Neurol Neurosurg Psychiatry. 1999; 67(4):492–496. PMID:
10486397.

3. Chaudhuri KR, Healy DG, Schapira AH. National Institute for Clinical Excellence. Non-motor symptoms of Parkinson's disease: diagnosis and management. Lancet Neurol. 2006; 5(3):235–245. PMID:
16488379.

4. Schapira AH, Chaudhuri KR, Jenner P. Non-motor features of Parkinson disease. Nat Rev Neurosci. 2017; 18(7):435–450. PMID:
28592904.

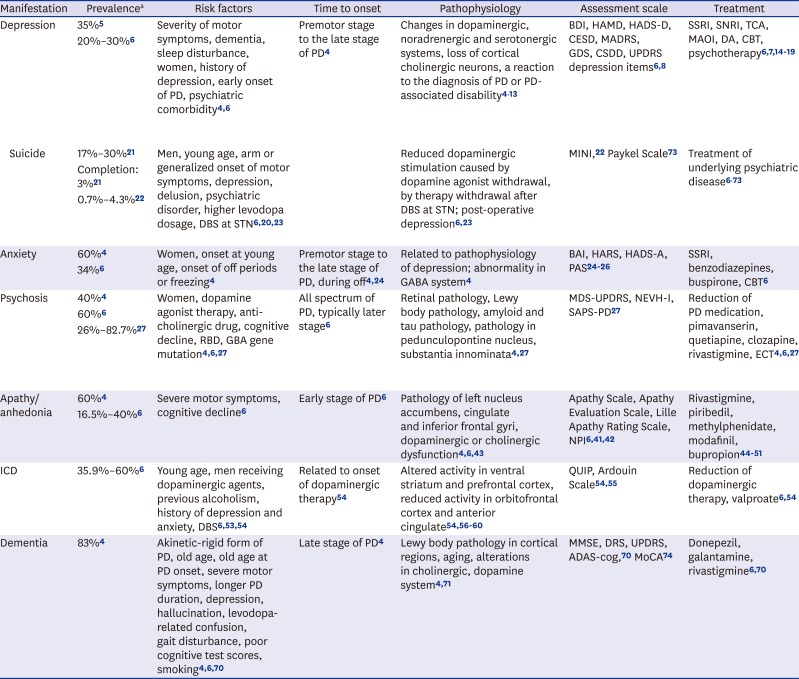
5. Reijnders JS, Ehrt U, Weber WE, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinson's disease. Mov Disord. 2008; 23(2):183–189. PMID:
17987654.

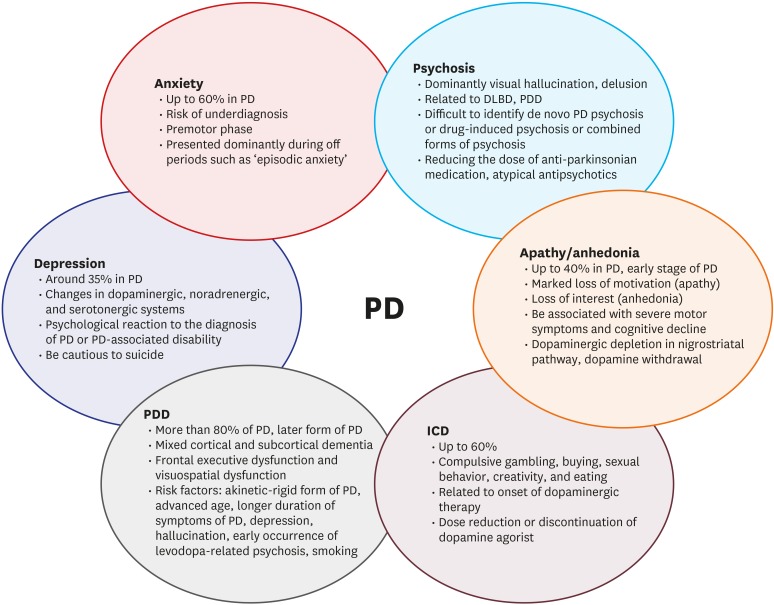
6. Aarsland D, Kramberger MG. Neuropsychiatric symptoms in Parkinson's disease. J Parkinsons Dis. 2015; 5(3):659–667. PMID:
26406147.
7. Starkstein SE, Brockman S. Management of depression in Parkinson's disease a systemic review. Mov Disord. 2017; 4(4):470–477.
8. Torbey E, Pachana NA, Dissanayaka NN. Depression rating scales in Parkinson's disease: a critical review updating recent literature. J Affect Disord. 2015; 184:216–224. PMID:
26114228.

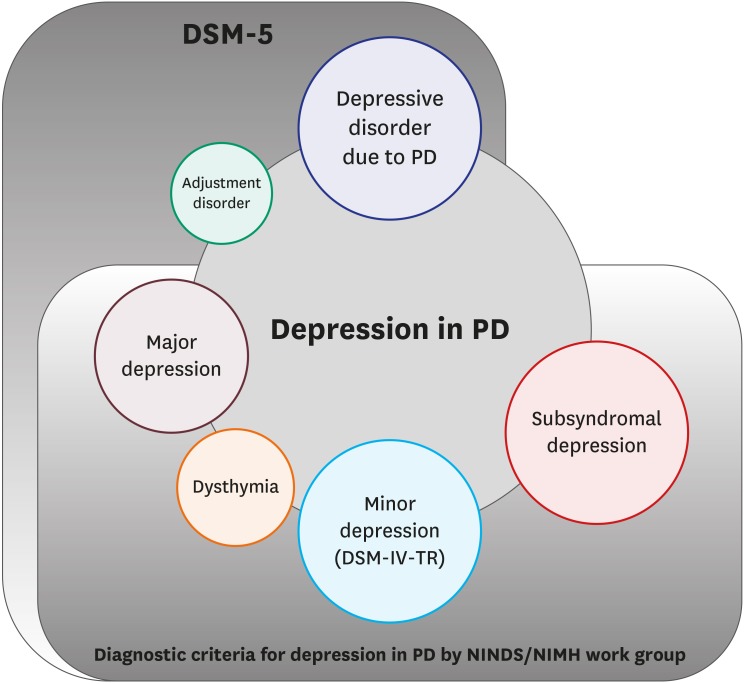
9. Marsh L, McDonald WM, Cummings J, Ravina B. NINDS/NIMH Work Group on Depression and Parkinson's Disease. Provisional diagnostic criteria for depression in Parkinson's disease: report of an NINDS/NIMH Work Group. Mov Disord. 2006; 21(2):148–158. PMID:
16211591.

10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association;2013.
11. Reijnders JS, Ehrt U, Weber WE, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinson's disease. Mov Disord. 2008; 23(2):183–189. PMID:
17987654.

12. Burn DJ. Beyond the iron mask: towards better recognition and treatment of depression associated with Parkinson's disease. Mov Disord. 2002; 17(3):445–454. PMID:
12112190.

13. Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain. 2005; 128(Pt 6):1314–1322. PMID:
15716302.

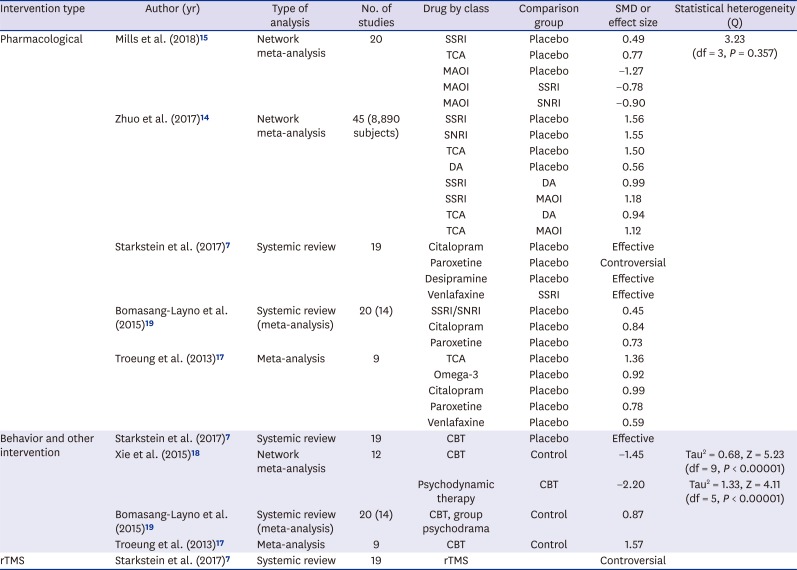
14. Zhuo C, Xue R, Luo L, Ji F, Tian H, Qu H, et al. Efficacy of antidepressive medication for depression in Parkinson disease: a network meta-analysis. Medicine (Baltimore). 2017; 96(22):e6698. PMID:
28562526.
15. Mills KA, Greene MC, Dezube R, Goodson C, Karmarkar T, Pontone GM. Efficacy and tolerability of antidepressants in Parkinson's disease: a systematic review and network meta-analysis. Int J Geriatr Psychiatry. 2018; 33(4):642–651. PMID:
29235150.

16. Menza M, Dobkin RD, Marin H, Mark MH, Gara M, Buyske S, et al. A controlled trial of antidepressants in patients with Parkinson disease and depression. Neurology. 2009; 72(10):886–892. PMID:
19092112.

17. Troeung L, Egan SJ, Gasson N. A meta-analysis of randomised placebo-controlled treatment trials for depression and anxiety in Parkinson's disease. PLoS One. 2013; 8(11):e79510. PMID:
24236141.

18. Xie CL, Wang XD, Chen J, Lin HZ, Chen YH, Pan JL, et al. A systematic review and meta-analysis of cognitive behavioral and psychodynamic therapy for depression in Parkinson's disease patients. Neurol Sci. 2015; 36(6):833–843. PMID:
25724804.

19. Bomasang-Layno E, Fadlon I, Murray AN, Himelhoch S. Antidepressive treatments for Parkinson's disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2015; 21(8):833–842. PMID:
26037457.

20. Lee T, Lee HB, Ahn MH, Kim J, Kim MS, Chung SJ, et al. Increased suicide risk and clinical correlates of suicide among patients with Parkinson's disease. Parkinsonism Relat Disord. 2016; 32:102–107. PMID:
27637284.

21. RN WL, Masoon MA, Acharyya S, NG HL, Tay KY, Au WL, et al. Suicide in Parkinson's disease. Mov Disord Clin Pract. 2018; 5(2):177–182. PMID:
30363456.

22. Kostić VS, Pekmezović T, Tomić A, Jecmenica-Lukić M, Stojković T, Spica V, et al. Suicide and suicidal ideation in Parkinson's disease. J Neurol Sci. 2010; 289(1-2):40–43. PMID:
19737673.

23. Voon V, Krack P, Lang AE, Lozano AM, Dujardin K, Schüpbach M, et al. A multicentre study on suicide outcomes following subthalamic stimulation for Parkinson's disease. Brain. 2008; 131(Pt 10):2720–2728. PMID:
18941146.

24. Chen JJ, Marsh L. Anxiety in Parkinson's disease: identification and management. Ther Adv Neurol Disorder. 2014; 7(1):52–59.

25. Shulman LM, Taback RL, Rabinstein AA, Weiner WJ. Non-recognition of depression and other non-motor symptoms in Parkinson's disease. Parkinsonism Relat Disord. 2002; 8(3):193–197. PMID:
12039431.

26. Leentjens AF, Dujardin K, Pontone GM, Starkstein SE, Weintraub D, Martinez-Martin P. The Parkinson Anxiety Scale (PAS): development and validation of a new anxiety scale. Mov Disord. 2014; 29(8):1035–1043. PMID:
24862344.

27. Ffytche DH, Creese B, Politis M, Chaudhuri KR, Weintraub D, Ballard C, et al. The psychosis spectrum in Parkinson disease. Nat Rev Neurol. 2017; 13(2):81–95. PMID:
28106066.

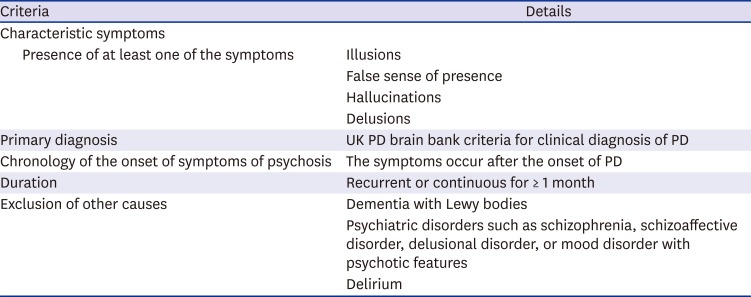
28. Ravina B, Marder K, Fernandez HH, Friedman JH, McDonald W, Murphy D, et al. Diagnostic criteria for psychosis in Parkinson's disease: report of an NINDS, NIMH work group. Mov Disord. 2007; 22(8):1061–1068. PMID:
17266092.

29. Ballanger B, Strafella AP, van Eimeren T, Zurowski M, Rusjan PM, Houle S, et al. Serotonin 2A receptors and visual hallucinations in Parkinson disease. Arch Neurol. 2010; 67(4):416–421. PMID:
20385906.

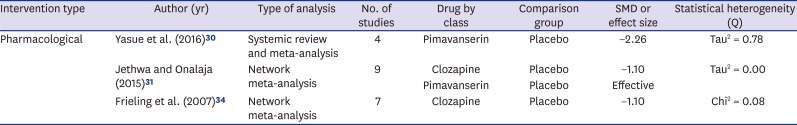
30. Yasue I, Matsunaga S, Kishi T, Fujita K, Iwata N. Serotonin 2A receptor inverse agonist as a treatment for Parkinson's disease psychosis: a systematic review and meta-analysis of serotonin 2A receptor negative modulators. J Alzheimers Dis. 2016; 50(3):733–740. PMID:
26757194.

31. Jethwa KD, Onalaja OA. Antipsychotics for the management of psychosis in Parkinson's disease: systematic review and meta-analysis. BJPsych Open. 2015; 1(1):27–33. PMID:
27703720.

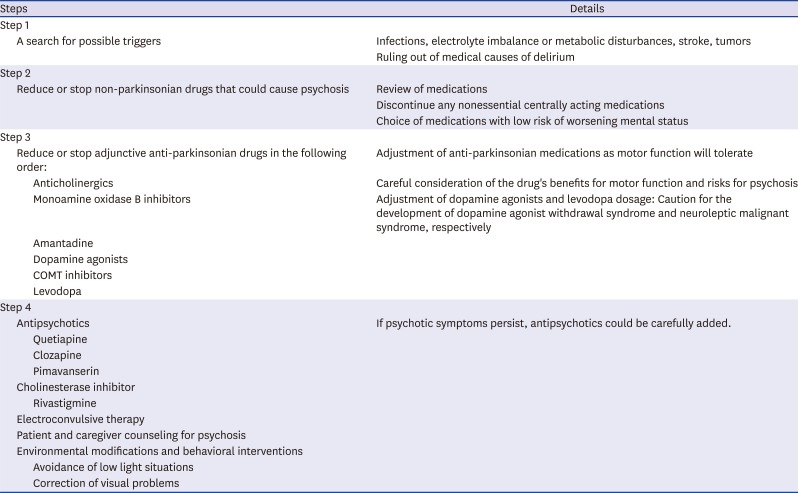
32. Martinez-Ramirez D, Okun MS, Jaffee MS. Parkinson's disease psychosis: therapy tips and the importance of communication between neurologists and psychiatrists. Neurodegener Dis Manag. 2016; 6(4):319–330. PMID:
27408981.

33. Schneider RB, Iourinets J, Richard IH. Parkinson's disease psychosis: presentation, diagnosis and management. Neurodegener Dis Manag. 2017; 7(6):365–376. PMID:
29160144.

34. Frieling H, Hillemacher T, Ziegenbein M, Neundörfer B, Bleich S. Treating dopamimetic psychosis in Parkinson's disease: structured review and meta-analysis. Eur Neuropsychopharmacol. 2007; 17(3):165–171. PMID:
17070675.

35. National Institute for Health and Care Excellence. Parkinson's Disease: Diagnosis and Management in Primary and Secondary Care (Clinical Guideline CG35). London: National Institute for Health and Care Excellence;2006.
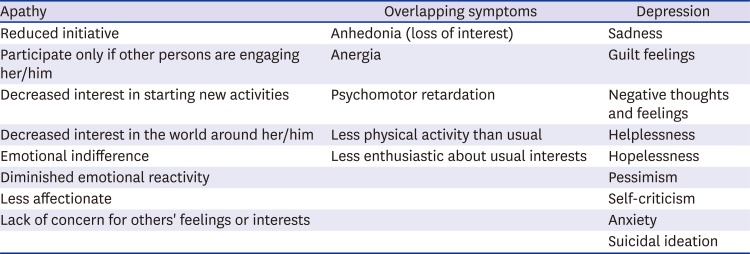
36. Marin RS. Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci. 1991; 3(3):243–254. PMID:
1821241.
37. Lanctôt KL, Agüera-Ortiz L, Brodaty H, Francis PT, Geda YE, Ismail Z, et al. Apathy associated with neurocognitive disorders: recent progress and future directions. Alzheimers Dement. 2017; 13(1):84–100. PMID:
27362291.

38. Kaji Y, Hirata K. Apathy and anhedonia in Parkinson's disease. ISRN Neurol. 2011; 2011:219427. PMID:
22389809.

39. Pagonabarraga J, Kulisevsky J, Strafella AP, Krack P. Apathy in Parkinson's disease: clinical features, neural substrates, diagnosis, and treatment. Lancet Neurol. 2015; 14(5):518–531. PMID:
25895932.

40. Drijgers RL, Dujardin K, Reijnders JS, Defebvre L, Leentjens AF. Validation of diagnostic criteria for apathy in Parkinson's disease. Parkinsonism Relat Disord. 2010; 16(10):656–660. PMID:
20864380.

41. Sockeel P, Dujardin K, Devos D, Denève C, Destée A, Defebvre L. The Lille apathy rating scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2006; 77(5):579–584. PMID:
16614016.

42. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994; 44(12):2308–2314. PMID:
7991117.

43. Dujardin K, Langlois C, Plomhause L, Carette AS, Delliaux M, Duhamel A, et al. Apathy in untreated early-stage Parkinson disease: relationship with other non-motor symptoms. Mov Disord. 2014; 29(14):1796–1801. PMID:
25370724.

44. Devos D, Moreau C, Maltête D, Lefaucheur R, Kreisler A, Eusebio A, et al. Rivastigmine in apathetic but dementia and depression-free patients with Parkinson's disease: a double-blind, placebo-controlled, randomised clinical trial. J Neurol Neurosurg Psychiatry. 2014; 85(6):668–674. PMID:
24218528.

45. Thobois S, Lhommée E, Klinger H, Ardouin C, Schmitt E, Bichon A, et al. Parkinsonian apathy responds to dopaminergic stimulation of D2/D3 receptors with piribedil. Brain. 2013; 136(Pt 5):1568–1577. PMID:
23543483.

46. Camargos EF, Quintas JL. Apathy syndrome treated successfully with modafinil. BMJ Case Rep. 2011; 2011:pii: bcr0820114652.

47. Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson's disease. Mov Disord. 2011; 26(Suppl 3):S42–S80. PMID:
22021174.

48. Lou JS. Fatigue in Parkinson's disease and potential interventions. NeuroRehabilitation. 2015; 37(1):25–34. PMID:
26409691.
49. Peña E, Mata M, López-Manzanares L, Kurtis M, Eimil M, Martínez-Castrillo JC, et al. Antidepressants in Parkinson's disease. Recommendations by the movement disorder study group of the Neurological Association of Madrid. Neurologia. 2016; 33(6):395–402.

50. Grandas F, López-Manzanares L. Bupropion-induced parkinsonism. Mov Disord. 2007; 22(12):1830–1831. PMID:
17534961.

51. Cheng WC, Liu CM, Hsieh MH, Hwang TJ. Bupropion-related parkinsonism and dystonia. J Clin Psychopharmacol. 2009; 29(6):616–618. PMID:
19910737.

52. Corvol JC, Artaud F, Cormier-Dequaire F, Rascol O, Durif F, Derkinderen P, et al. Longitudinal analysis of impulse control disorders in Parkinson disease. Neurology. 2018; 91(3):e189–e201. PMID:
29925549.

53. Weintraub D, Siderowf AD, Potenza MN, Goveas J, Morales KH, Duda JE, et al. Association of dopamine agonist use with impulse control disorders in Parkinson disease. Arch Neurol. 2006; 63(7):969–973. PMID:
16831966.

54. Leeman RF, Billingsley BE, Potenza MN. Impulse control disorders in Parkinson's disease: background and update on prevention and management. Neurodegener Dis Manag. 2012; 2(4):389–400. PMID:
23606908.

55. Rieu I, Martinez-Martin P, Pereira B, De Chazeron I, Verhagen Metman L, Jahanshahi M, et al. International validation of a behavioral scale in Parkinson's disease without dementia. Mov Disord. 2015; 30(5):705–713. PMID:
25809278.

56. Lee JY, Seo SH, Kim YK, Yoo HB, Kim YE, Song IC, et al. Extrastriatal dopaminergic changes in Parkinson's disease patients with impulse control disorders. J Neurol Neurosurg Psychiatry. 2014; 85(1):23–30. PMID:
24023269.

57. Steeves TD, Miyasaki J, Zurowski M, Lang AE, Pellecchia G, Van Eimeren T, et al. Increased striatal dopamine release in Parkinsonian patients with pathological gambling: a [11C] raclopride PET study. Brain. 2009; 132(Pt 5):1376–1385. PMID:
19346328.

58. Rao H, Mamikonyan E, Detre JA, Siderowf AD, Stern MB, Potenza MN, et al. Decreased ventral striatal activity with impulse control disorders in Parkinson's disease. Mov Disord. 2010; 25(11):1660–1669. PMID:
20589879.

59. Voon V, Sohr M, Lang AE, Potenza MN, Siderowf AD, Whetteckey J, et al. Impulse control disorders in Parkinson disease: a multicenter case--control study. Ann Neurol. 2011; 69(6):986–996. PMID:
21416496.

60. van Eimeren T, Pellecchia G, Cilia R, Ballanger B, Steeves TD, Houle S, et al. Drug-induced deactivation of inhibitory networks predicts pathological gambling in PD. Neurology. 2010; 75(19):1711–1716. PMID:
20926784.

61. Castrioto A, Thobois S, Carnicella S, Maillet A, Krack P. Emotional manifestations of PD: Neurobiological basis. Mov Disord. 2016; 31(8):1103–1113. PMID:
27041545.

62. Hälbig TD, Tse W, Frisina PG, Baker BR, Hollander E, Shapiro H, et al. Subthalamic deep brain stimulation and impulse control in Parkinson's disease. Eur J Neurol. 2009; 16(4):493–497. PMID:
19236471.

63. Rodriguez-Oroz MC, López-Azcárate J, Garcia-Garcia D, Alegre M, Toledo J, Valencia M, et al. Involvement of the subthalamic nucleus in impulse control disorders associated with Parkinson's disease. Brain. 2011; 134(Pt 1):36–49. PMID:
21059746.

64. Okun MS, Weintraub D. Should impulse control disorders and dopamine dysregulation syndrome be indications for deep brain stimulation and intestinal levodopa? Mov Disord. 2013; 28(14):1915–1919. PMID:
24243803.

65. Kim A, Kim YE, Kim HJ, Yun JY, Yang HJ, Lee WW, et al. A 7-year observation of the effect of subthalamic deep brain stimulation on impulse control disorder in patients with Parkinson's disease. Parkinsonism Relat Disord. 2018; pii: S1353-8020(18)30313-4.

66. Aarsland D, Brønnick K, Ehrt U, De Deyn PP, Tekin S, Emre M, et al. Neuropsychiatric symptoms in patients with Parkinson's disease and dementia: frequency, profile and associated care giver stress. J Neurol Neurosurg Psychiatry. 2007; 78(1):36–42. PMID:
16820421.

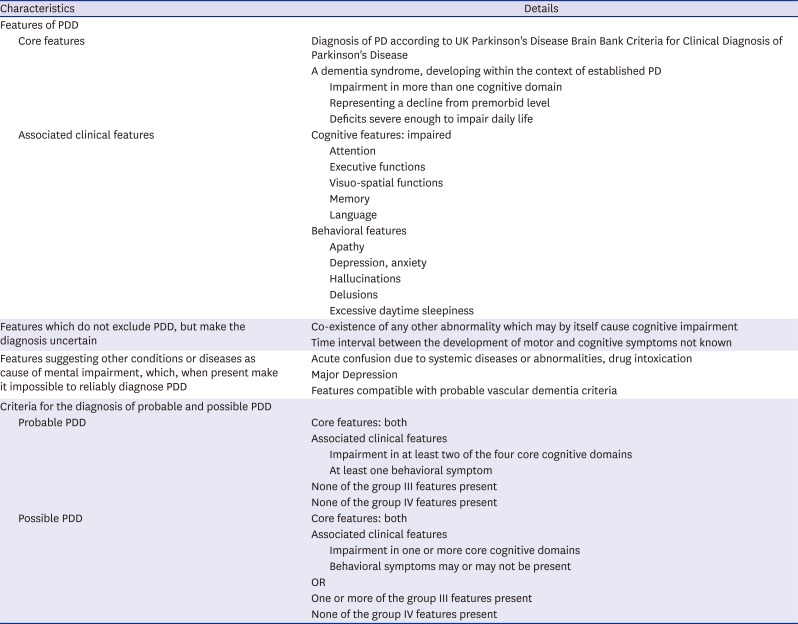
67. Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson's disease. Mov Disord. 2007; 22(12):1689–1707. PMID:
17542011.

68. Litvan I, Goldman JG, Tröster AI, Schmand BA, Weintraub D, Petersen RC, et al. Diagnostic criteria for mild cognitive impairment in Parkinson's disease: Movement Disorder Society Task Force guidelines. Mov Disord. 2012; 27(3):349–356. PMID:
22275317.

69. McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology. 2017; 89(1):88–100. PMID:
28592453.
70. Wood LD, Neumiller JJ, Setter SM, Dobbins EK. Clinical review of treatment options for select nonmotor symptoms of Parkinson's disease. Am J Geriatr Pharmacother. 2010; 8(4):294–315. PMID:
20869620.

71. Halliday G, Lees A, Stern M. Milestones in Parkinson's disease--clinical and pathologic features. Mov Disord. 2011; 26(6):1015–1021. PMID:
21626546.

72. Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980; 137(5):535–544. PMID:
7369396.
73. Nazem S, Siderowf AD, Duda JE, Brown GK, Ten Have T, Stern MB, et al. Suicidal and death ideation in Parkinson's disease. Mov Disord. 2008; 23(11):1573–1579. PMID:
18618660.

74. Hoops S, Nazem S, Siderowf AD, Duda JE, Xie SX, Stern MB, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology. 2009; 73(21):1738–1745. PMID:
19933974.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download