INTRODUCTION
In recognizing the benefits of breast milk, many countries have provided educational programs and recommended breastfeeding (BF). Furthermore, the World Health Organization (WHO) and the United Nation's International Children's Emergency Fund (UNICEF) have strongly supported the practice of exclusive BF for approximately the first 6 months of infancy.
1 In 1991, the WHO and UNICEF launched the Baby-friendly Hospital Initiative (BFHI). Since its launch, the BFHI has grown considerably, with over 152 countries worldwide implementing the initiative. The initiative has measurable and proven impact and has increased the likelihood of infants being exclusively breastfed for the first 6 months of life.
2 A certificate from the BFHI is awarded if a hospital fulfills the “Ten steps for BFHI.” The American Academy of Pediatrics decided to support this Ten Steps program in 2009, and has recommended to abide by these initiatives to promote the rate of BF initiation just after birth, to prolong the duration, and exclusive BF practices. Most hospital maternity clinics are managed and regulated under the BFHI recommendations.
34
In Korea, the BFHI was initiated in 1993 by UNICEF Korea, and has led several institutions to execute promotional programs to increasing the rate of BF. Even though UNICEF Korea has worked diligently to increase the number of BFHs in Korea, the number of BFHI-certificates awarded to hospitals in Korea is less than 20 nationally.
The rate of exclusive breastfeeding (EBF) is still low in Korea. According to a recent government report, the rate of EBF was 52.6% at 1 month of age, 47.2% at 3 months, and decreased drastically to 9.4% at 6 months.
5
This rate is desperately low compared to the EBF rate of 22.3% at 6 months in the United States (U.S.).
6 Diverse efforts to promote human milk BF have been launched by the Korean Government as well as by several medical societies during the past 2 decades. However, the rate of BF practices continues to decrease. The Korean Ministry of Health and Welfare had established a master plan aiming for a 66.8% BF rate at 6 months after birth by the year 2020.
7 It is very important to divulge the importance, effectiveness, and benefits of the BFHI to successfully achieve the goals of this health program to increase the BF rate.
Doctors assume that everyone knows the absolute benefits of human breast milk. However, many infants are not currently benefiting from mother's breast milk. There is a degree of uncertainty regarding whether pregnant Korean women are sufficiently knowledgeable about human milk, what influences their intention to continue BF, and what factors deter successful human milk feeding. Recent studies have shown that maternal knowledge and interest were associated with a longer duration of BF and intention to breastfeed in Korea.
8 Moreover, recent studies have found that maternal knowledge about infant health benefits was directly related to their intention to exclusively breastfeed in diverse urban populations.
9 Another study has shown the significant roles hospitals play in BF initiation and promotion, with rooming-in care of infants, initial BF practices, and education during hospital stay as important practices.
10 Many other studies have focused on the socio-demographic characteristics of Korean women. These studies found that delivery method, education level, employment status before marriage, and the amount of prenatal care affected the initiation and duration of BF,
11 and showed that younger maternal age and higher maternal education levels were positively associated with EBF up to 6 months of age in Korea.
12
We performed this study to investigate whether there are any difference in the knowledge regarding human breast milk, participation in antenatal BF education programs, and postnatal intention to BF of the antenatal mothers planning to give birth at Baby-Friendly Hospitals (BFHs) and those at non-BFHs.
METHODS
Study design, samples, and surveys
This cross-sectional study examined the factors fostering successful human BF in Korean pregnant women. Questionnaire surveys were collected from pregnant women who visited the obstetric clinics of 1 university hospital, 3 private clinics in Seoul, and 1 private clinic in Gumi from January 2016 to August 2016. Two private clinics were already approved as BFHs. The pregnant women were randomly selected to receive the questionnaire. In this study, we analyzed the questionnaire results to investigate their intentions for EBF and duration of BF, and the factors affecting their decisions. We also analyzed differences between mothers who plan to give birth in BFHs and non-BFHs.
A total of 414 pregnant women responded to the questionnaire; 150 (36.2%) women were from BFHs and 264 (63.2%) were from non-BFHs. We excluded 57 women who had not yet decided on BF and the duration of BF. The final number of included respondents was 357, but the number of respondents per question was not constant due to non-responses.
A stand-alone questionnaire was designed to evaluate respondents' knowledge about human breast milk and interest about continuing BF. The questionnaire measured the following: maternal age at delivery, height, occupation, marital status, obstetric history, intended method of delivery, any pregnancy-associated complications, intentions for BF just after delivery and the duration of BF (no BF at all, 1–6, 6–12, 12–18 months, longer than 18 months), plans for exclusive BF (6 months), plans for rooming-in care, knowledge of human breastmilk, participation in antenatal BF education programs, attitude and opinion regarding BF as a working mother, sources of influence to support BF, and any possibility of succumbing to the temptation of formula-selling companies. We investigated the respondents' level of awareness of the benefits of BF to the infant and mother by scores based on upon their answers to items relative to BF benefits. We converted responses to 5 benefit items into scores of 100 points about awareness of the benefits of BF for infants and mothers. The 5 benefits listed for infants were as follows: 1) baby is less likely to get sick, 2) baby feels more comfortable, 3) brain development is more accelerated, 4) human milk is more easily digested, and 5) baby spits up human milk less. The 5 benefits listed for BF mothers were as follows: 1) the BF mother quickly recovers to original body weight, 2) BF enhances postnatal uterine contraction and lessens uterine bleeding, 3) BF prevents breast cancer and ovarian cancer, 4) BF delays ovulation and induces natural contraception, and 5) BF delays menstruation after birth. The median values of their scores for the benefits of BF to the infant and mother were 60 and 40 points, respectively.
Data collection and analysis
We developed a stand-alone questionnaire to investigate intentions for EBF and BF duration among pregnant women. In addition, intentions for EBF and BF duration were measured using a self-completed questionnaire. SPSS 23.0 (IBM Corp., Armonk, NY, USA) was used for all analysis. The χ2test was used to determine differences in intentions for EBF and BF duration according to the questionnaire results. We accepted factors as significant when the P value was less than 0.05. Afterwards, multivariate analysis was performed with logistic regression by selecting variables with a significance level less than 0.05 in the univariate analysis. Odds ratios (ORs) with associated 95% confidence intervals (CIs) were reported.
Ethics statement
The current study was approved by the Institutional Review Board (IRB) of the Hanyang University Hospital (IRB approval No. 2015-07-027).
RESULTS
Mother's antenatal plan for their baby's future feeding
The antenatal goal of EBF was planned only by 83 women (20%), 274 (66.2%) planned mixed feeding, and 57 (13.8%) had not yet determined their feeding plan. Despite the small number of women planning EBF, 216 (52%) planned to continue BF for more than 6 months, and 53 (12.8%) planned to continue even after 18 months (
Table 1).
Table 1
Mother's antenatal plan for their baby's future feeding

|
Characteristics |
No. (%) |
|
BF intention |
|
|
EBF |
83 (20.0) |
|
Mixed feeding |
274 (66.2) |
|
Undetermined |
57 (13.8) |
|
Total |
414 (100.0) |
|
BF duration (exclusive and mixed), mon |
|
|
> 18 |
53 (12.8) |
|
13–18 |
27 (6.5) |
|
7–12 |
136 (32.9) |
|
3–6 |
104 (25.1) |
|
< 3 |
37 (8.9) |
|
Undetermined |
57 (13.8) |
|
Total |
414 (100.0) |

Characteristics of study population
The characteristics of participants are summarized in
Table 2. We also analyzed the questionnaire data according to whether participants belonged to a BFH, according to their intention for EBF, and EBF for more than 6 months. The mothers' ages ranged between 23 and 45, with a mean of 32.53 ± 3.49 years. More than half of mothers (65.5%) were primiparous and most women (76.2%) were planning a normal spontaneous vaginal delivery (NSVD). Approximately 60% of respondents (59.4%) showed a preference for rooming-in care of their infants after delivery. Most women intended to BF just after delivery (92.7%).
Table 2
Characteristics of study population

|
Characteristics |
Categories |
No. (%) |
Mean ± SD |
|
Maternal age, yr |
|
357 (100) |
32.53 ± 3.49 |
|
Parity |
Primiparous |
234 (65.5) |
|
|
Multiparous |
123 (34.5) |
|
|
Method of delivery planned |
NSVD |
272 (76.2) |
|
|
Cesarean |
85 (23.8) |
|
|
Maternal educationa
|
High school graduate or below |
55 (15.4) |
|
|
College graduate or above |
298 (83.5) |
|
|
Gestational hypertension |
Yes |
12 (3.4) |
|
|
No |
335 (96.6) |
|
|
Occupation |
Employed |
197 (55.2) |
|
|
Housewife |
160 (44.8) |
|
|
Plans to BF just after birtha
|
Yes |
331 (92.7) |
|
|
No |
12 (3.4) |
|
|
Plans for rooming-ina
|
Yes |
212 (59.4) |
|
|
No |
90 (25.2) |
|
|
Awareness of benefits of BF for infant |
|
357 (100) |
56.60 ± 28.23 |
|
Awareness of benefits of BF for mother |
|
357 (100) |
45.71 ± 30.00 |
|
Antenatal education for successful BF |
Yes |
143 (40.1) |
|
|
No |
214 (59.9) |
|
|
Antenatal BF education instructora
|
Medical-professional |
119 (33.3) |
|
|
Non-medical-professional |
24 (6.7) |
|
|
Reason or support for initiating BFa
|
Mass media |
169 (47.3) |
|
|
Family or relatives |
34 (9.5) |
|
|
Mother-in-law |
28 (7.8) |
|
|
Professional support |
12 (3.4) |
|
|
Plans delivery at BFH |
Yes |
126 (35.3) |
|
|
No |
231 (64.7) |
|
|
Likely to decrease BF due to formula company gifta
|
Yes |
38 (10.6) |
|
|
No |
225 (63.0) |
|

The mean ± standard deviation of awareness of BF benefits for infant and mothers was 58.60 ± 28.23 and 45.71 ± 30.00, respectively. The selected responses concerning benefits of BF for infants were: 1) baby is less likely to get sick (81.8%), 2) baby feels more comfortable (73.9%), 3) brain development is more accelerated (72.6%), 4) human milk is more easily digested (71.3%), and 5) baby spits up human milk less (28.3%). The selected responses concerning benefits of BF for BF mothers were: 1) the BF mother quickly recovers to original body weight (68.6%), 2) BF enhances postnatal uterine contraction and lessens uterine bleeding (49.5%), 3) BF prevents breast cancer and ovarian cancer (46.6%), 4) BF delays ovulation and induces natural contraception (34.5%), and 5) BF delays menstruation after birth (31.4%). The median values of their scores for the benefits of BF to the infant and mother were 56.60 and 44.7 points, respectively. The respondents were well aware of the benefits of BF for babies and less aware of benefits for mothers.
The survey questioned participation in antenatal BF education programs. Less than half (40.1%) of respondents had attended prenatal BF education programs. Therefore, it can be assumed that Koreans still have a low awareness of antenatal BF education. However, among women who had attended antenatal BF education programs (n = 143), 119 respondents (82.6%) had received BF education from experts (i.e., an obstetrician, pediatrician, lactation consultant, and professional nurse specialized in BF counseling).
A mother's decision to breastfeed can be influenced by mass media (47.3%), her family or relatives (9.5%), a mother-in-law (7.8%), or obstetrician (3.4%). Over half (55.2%) of respondents were employed either full-time or part-time. Among these, 168 mothers (85.3%) had full-time jobs, but for only 88 mothers (52.4%) were workplaces equipped with lactation room facilities.
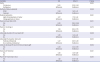
Responses of mothers with EBF intention
What factors significantly associated with strong intention of exclusive BF were investigated with expression in terms of OR and CI. Mothers who planned rooming-in care just after delivery had a significant intention to EBF (
P < 0.05). Logistic regression analysis revealed that the EBF intention (OR, 3.11; 95% CI, 1.55–6.23) was significantly higher among those who were planning for rooming-in after delivery compared to those who were not. Women who had sufficient knowledge of the many benefits of BF for infants (scores higher than 60 points) were 2.11 times more likely (OR, 2.11; 95% CI, 1.28–3.49) to have a positive association with EBF compared with those who did not. Moreover, sufficient knowledge of the many benefits of BF for the mother (
P = 0.001; OR, 2.59; 95% CI, 1.50–4.50), participation in antenatal BF education programs (
P < 0.000; OR, 3.87; 95% CI, 2.31–6.49), receiving BF education from a medical professional (
P < 0.05; OR, 3.62; 95% CI, 1.17–11.26), planning delivery at a BFH (
P = 0.01; OR, 2.32; 95% CI, 1.40–3.82), having a workplace with a lactation room (
P = 0.020; OR, 2.99; 95% CI, 1.16–7.71) were positively associated with intention for EBF. However, the intention to BF would likely decrease due to the receipt of a gift offered from a company selling milk formula (
P = 0.026; OR, 0.34; 95% CI, 0.13–0.92) and was negatively associated with intention for EBF (
Table 3).
Table 3
Responses of mothers with EBF intention

|
Variables |
OR |
95% CI |
P value |
|
Plans for rooming-in care |
|
|
0.001 |
|
Yes |
3.11 |
1.55–6.23 |
|
No |
Reference |
Reference |
|
Awareness of benefits of BF for infant |
|
|
0.003 |
|
≥ 60a
|
2.11 |
1.28–3.49 |
|
< 60a
|
Reference |
Reference |
|
Awareness of benefits of BF for mother |
|
|
0.001 |
|
≥ 40b
|
2.59 |
1.50–4.50 |
|
< 40b
|
Reference |
Reference |
|
Antenatal education for successful BF |
|
|
< 0.001 |
|
Yes |
3.87 |
2.31–6.49 |
|
No |
Reference |
Reference |
|
Antenatal BF education instructor |
|
|
0.019 |
|
Medical professionals |
3.62 |
1.17–11.26 |
|
Non-medical professional |
Reference |
Reference |
|
Plans delivery at BFH |
|
|
0.001 |
|
Yes |
2.32 |
1.40–3.82 |
|
No |
Reference |
Reference |
|
Lactation room-in workplace for employed women |
|
|
0.020 |
|
Yes |
2.99 |
1.16–7.71 |
|
No |
Reference |
Reference |
|
Likely to decrease BF due to formula company gift |
|
|
0.026 |
|
Yes |
0.34 |
0.13–0.92 |
|
No |
Reference |
Reference |

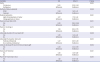
Responses by mothers with intention to breastfeed more than 6 months
Table 4 shows the personal and socio-environmental characteristics of pregnant women correlated with antenatal planning to continue BF in any form for over 6 months. Participants were divided into 2 groups based on BF duration: longer or shorter than 6 months.
Table 4
Responses by mothers with intention to breastfeed (exclusive or mixed feeding) more than 6 months

|
Variables |
OR |
95% CI |
P value |
|
Plans to BF just after birth |
|
|
< 0.001 |
|
Yes |
17.90 |
2.28–140.29 |
|
No |
Reference |
Reference |
|
Plans for rooming-in |
|
|
0.011 |
|
Yes |
1.90 |
1.15–3.14 |
|
No |
Reference |
Reference |
|
Awareness of benefits of BF for infant |
|
|
0.002 |
|
≥ 60a
|
2.08 |
1.30–3.34 |
|
< 60a
|
Reference |
Reference |
|
Awareness of benefits of BF for mother |
|
|
0.047 |
|
≥ 40b
|
1.58 |
1.00–2.49 |
|
< 40b
|
Reference |
Reference |
|
Antenatal education for successful BF |
|
|
< 0.001 |
|
Yes |
2.43 |
1.54–3.83 |
|
No |
Reference |
Reference |
|
Antenatal BF education instructor |
|
|
0.025 |
|
Medical Professionals |
2.75 |
1.11–6.82 |
|
Non-medical professional |
Reference |
Reference |
|
Lactation room-in workplace for employed women |
|
|
0.003 |
|
Yes |
3.25 |
1.47–7.21 |
|
No |
Reference |
Reference |
|
Likely to decrease BF due to formula company gift |
|
|
0.047 |
|
Yes |
0.50 |
0.25–1.00 |
|
No |
Reference |
Reference |

Women who were planning to start BF just after delivery were 17.90 times more likely to plan to continue BF for more than 6 months than those who did not plan to start BF after delivery (P < 0.000; OR, 17.90; 95% CI, 2.28–140.29). Planning for rooming-in after delivery (P < 0.05; OR, 1.90; 95% CI, 1.15–3.14), greater awareness of benefits of BF for the infant (P < 0.05; OR, 2.08; 95% CI, 1.30–3.34), greater awareness of benefits of BF for the mother (P < 0.05; OR, 1.58; 95% CI, 1.00–2.49), participation in antenatal BF education programs (P < 0.000; OR, 2.43; 95% CI, 1.54–3.83), receiving instruction from medical professionals (P < 0.05; OR, 2.75; 95% CI, 1.11–6.82), having a workplace with lactation room facilities (P < 0.05; OR, 3.25; 95% CI, 1.47–7.21) were significantly associated with planning to breastfeed for longer than 6 months. A woman who was planning to breastfeed for more than 6 months, but who had received formula as a gift and began to feed using formula was significantly associated with BF for less than 6 months' duration. (P = 0.047; OR, 0.50; 95% CI, 0.25–1.00).
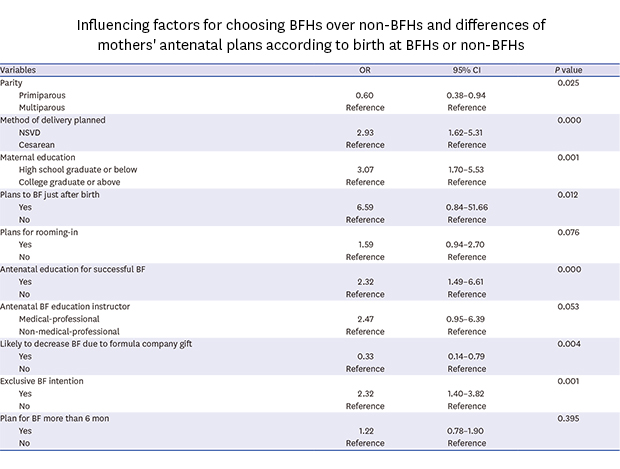
Influencing factors for choosing BFHs over non-BFHs
Table 5 shows that differences between mothers who were planning to give birth in an institution certified by the BFHI or a non-BFHI institution. Primiparous mothers (
P < 0.05; OR, 0.60; 95% CI, 0.38–0.94) and women who were more likely to decrease BF practice due to a formula company gift (
P < 0.005; OR, 0.33; 95% CI, 0.14–0.79) were more likely to give birth in non-BFHI institution. Conversely, women who were planning a NSVD delivery method (
P < 0.000; OR, 2.93; 95% CI, 1.62–5.31), women who were high school graduates or had lower education levels (
P < 0.005; OR, 3.07; 95% CI, 1.70–5.53), women who planned to start BF after delivery (
P < 0.05; OR, 6.59; 95% CI, 0.84–51.66), or women who participated in antenatal BF education programs (
P < 0.000; OR, 2.32; 95% CI, 1.49–3.61) were more likely to give birth in a BFHI institution.
Table 5
Influencing factors for choosing BFHs over non-BFHs and differences of mothers' antenatal plans according to birth at BFHs or non-BFHs
|
Variables |
OR |
95% CI |
P value |
|
Parity |
|
|
0.025 |
|
Primiparous |
0.60 |
0.38–0.94 |
|
Multiparous |
Reference |
Reference |
|
Method of delivery planned |
|
|
0.000 |
|
NSVD |
2.93 |
1.62–5.31 |
|
Cesarean |
Reference |
Reference |
|
Maternal education |
|
|
0.001 |
|
High school graduate or below |
3.07 |
1.70–5.53 |
|
College graduate or above |
Reference |
Reference |
|
Plans to BF just after birth |
|
|
0.012 |
|
Yes |
6.59 |
0.84–51.66 |
|
No |
Reference |
Reference |
|
Plans for rooming-in |
|
|
0.076 |
|
Yes |
1.59 |
0.94–2.70 |
|
No |
Reference |
Reference |
|
Antenatal education for successful BF |
|
|
0.000 |
|
Yes |
2.32 |
1.49–6.61 |
|
No |
Reference |
Reference |
|
Antenatal BF education instructor |
|
|
0.053 |
|
Medical-professional |
2.47 |
0.95–6.39 |
|
Non-medical-professional |
Reference |
Reference |
|
Likely to decrease BF due to formula company gift |
|
|
0.004 |
|
Yes |
0.33 |
0.14–0.79 |
|
No |
Reference |
Reference |
|
Exclusive BF intention |
|
|
0.001 |
|
Yes |
2.32 |
1.40–3.82 |
|
No |
Reference |
Reference |
|
Plan for BF more than 6 mon |
|
|
0.395 |
|
Yes |
1.22 |
0.78–1.90 |
|
No |
Reference |
Reference |

The planning for rooming-in care after delivery (P = 0.076; OR, 1.59; 95% CI, 0.94–2.70) and receiving BF education from a medical professional (P = 0.053; OR, 2.47; 95% CI, 0.95–6.39) were weakly associated with giving birth in a BFHI institution. Women who were planning to give birth in a BFHI institution were significantly associated with the initiation of EBF practices (P < 0.005; OR, 2.32; 95% CI, 1.40–3.82). Conversely, women who planned to give birth in a BFHI institution were not associated with more than 6 months' BF duration (P > 0.05).
DISCUSSION
In an international comparison of rates of human milk feeding habits during the neonatal period, Korea has reported a higher frequency than other countries (Korea, 95.6%; USA, 81.1%; the Netherlands, 81.0%; Germany, 96.0%; Italy, 91.0%). However, after 6 months, BF practice rates decrease rapidly (Korea, 25.6%; USA, 51.8%; the Netherlands, 37.0%; Germany, 48.0%; Italy, 47.0%).
6 The present study surveyed the characteristics of those who were willing to continue BF, and the findings of this study are likely to be valuable for future use in maternal education programs to encourage BF in Korea. The results of this study suggest that improving maternal knowledge about BF and interest could be an effective strategy to encourage successful BF practices.
We conducted a questionnaire survey of 414 pregnant women to explore knowledge and interest associated with providing BF support to pregnant women. Of the participants, 20.0% planned to initiate EBF, even in the face of physical difficulties related to BF, such as mastitis, breast engorgement, chest pain, and inverted nipples. However, 67.6% of women decided to combine bottle-feeding and BF. Korean mothers planned to stop BF at an average of 11.1 months, but the actual duration of BF was 5.6 months. This finding indicates that BF as planned was difficult to ensue due to physical impediments, including maternal factors, which were the main obstacles to BF, followed by “lack of breast milk” (43.3%) and the need to “return to work” (11.4%).
6
In order to encourage successful BF, government efforts are needed. The most relevant policies are 1) the establishment of lactation rooms in public places such as workplaces and universities (30.1%), 2) antenatal education for BF in hospitals (25.3%), and 3) the implementation of rooming-in care after delivery in hospitals.
6 To support these recommendations, we carried out an analysis of the association between socio-environmental characteristics, the establishment of lactation room facilities in the workplace, BF knowledge and interest, and intention for the duration of BF and the initiation of EBF.
First of all, we found an association between socio-environmental characteristics of pregnant women and their intention to initiate EBF and for a longer BF duration. Previous studies showed that a higher education level had a positive effect on the initiation of EBF and BF duration in Korea.
1112 However, in our study, there was no association between maternal education level and intentions for EBF or BF duration because most mothers (83.5%) had graduated college or higher, and there was no difference in the education level among these Korean mothers. In contrast, we found that giving birth at a BFHI institution increased by 3.07 times in mothers with lower education which is not consistent with a previous study.
13 The previous study showed that over 13 years of education led to a 2.2% increase in giving birth in BFHI hospitals compared with mothers with fewer than 12 years of education in the USA. In this study, 58% of low-educated women planned to give birth at a BFHI hospital, while only 31% of highly-educated women planned to give birth at a BFHI hospital.
In addition, this study confirmed that the BFHI hospital might have had a positive effect on intentions for EBF as also shown in previous studies.
1415 but this was not associated with BD duration. A BFHI institution may encourage the implementation of “Ten Steps to Successful Breastfeeding,” which include, rooming-in and BF after delivery, key practices in supporting BF.
The finding of this study showing that rooming-in after delivery is strongly associated with EBF and longer BF duration was consistent with a previous study,
1617 but giving birth at a BFH is weakly associated with rooming-in care after delivery (
P = 0.07). Conversely, BF just after delivery was very strongly associated with longer BF duration and giving birth at a BFHI institution, but was not associated with EBF intention. Women who intend to room-in showed a difference in their willingness to exclusively breastfeed, as maternal education level for this group was higher than university graduation. There was also a difference between employed women and housewives; employed women were more willing than housewives to room-in with their babies (employed women, 139; housewives, 73). This study showed that multiparous women were more likely to give birth at a BFH than primiparous women. Most women (76.2%) planned to give birth by NSVD, and of these 87.3% planned to give birth at a BFHI institution. There was a strong association between the delivery method and giving birth at a BFHI institution.
Next, we found that higher scores for BF knowledge and interest were associated with a stronger intention for EBF, longer BF duration, and giving birth at a BFH. BF knowledge was assessed in terms of the awareness of the benefits of BF to infants. Employed women were more aware of the benefits of BF for mothers and infants than were housewives.
In addition, an interest in BF was assessed as participation in prenatal BF education programs and being willing to continue BF even after receiving powdered milk formula as a gift. Prenatal BF education was one of the most important factors determining the initiation of EBF, but the rate of prenatal BF education in Korea was still relatively low compared to the results reported by other studies conducted in many other countries (Korea, 40.1%; Hong Kong, 56.2%).
18 Most women received prenatal BF education from professionals (83.2%), but a small number of women (16.8%) received prenatal BF education from non-professionals, such as general nurses or others who had BF experience. Regardless of who provided the BF education, it had a great influence on intentions for EBF and longer BF duration. The results of our investigation relative to the reasons for not receiving prenatal BF education were as follows: 1) no medical professionals recommended prenatal BF education (42.1%), 2) not enough time due to work constraints (29.7%), 3) medical professionals or internet recommended BF education, but the mother did not feel it was necessary (17.0%), and 4) the desire to rest (11.6%). These survey results suggest that an appropriate policy to support women in hospitals and workplaces is required.
Women were strongly influenced by mass media. However, this did not affect their intention for EBF and longer BF duration. Our study confirmed that the promotion of formula-based feeding was negatively associated with intentions for EBF, BF duration, and giving birth in a BFHI institution. Most mothers (85.6%) showed their willingness to continue BF even if they were gifted with powdered formula, but if they began using formula instead of BF then they will likely slowly stop BF. An intention to use formula instead of BF was 0.5 times more likely to have a negative association with intentions for BF duration over 6 months. The free gift of formula was strongly associated with shorter BF duration and was consistent with a previous study.
19 The promotional material provided by formula companies does have some positive aspects, such as providing childcare information, however it may likely strongly influence the choice to use formula, which can be a great inhibitor of BF. As indicated by the results of our study, the provision of lactation room facilities in the workplace is strongly associated with the intention for EBF and longer duration, which confirms that the government should support the establishment of workplace lactation rooms. The beneficial effect of a government-driven workplace lactation facility in Indonesia was already reported in 2015.
20
We also compared and analyzed the characteristics of mothers planning to give birth in a BFHI-affiliated institution. As a result, a mother who plans to give birth at a BFH has a strong willingness to continue with EBF regardless if a company gives a gift of formula. It is important to provide an environment where a mother can exclusively breastfeed after give birth in hospitals. The BFHI was developed to support the implementation of the “Ten Steps for Successful Breastfeeding” to provide an environment for exclusively breastfeed infants, it will lead to increasing the initiation of EBF practices. However, although UNICEF Korea launched an awareness campaign for the BFHI in 1993, as of February 2018, only 16 maternal and child health care centers were officially awarded BFHI certificates.
21 This number is significantly lower than the number of 20,000 BFHI-affiliated hospitals worldwide. In addition, according to a recent report, the rate of births in designated hospitals and maternity wards is extremely low at 5.0%.
22 The BFHI has effectively enhanced the BF rate globally, probably through eager participation of diverse organizations of medical professionals as well as government-driven public policies advocating these initiatives. The spread of the importance of the BFHI has a greater likelihood of being accomplished if these initiatives are included in the curriculums of medical schools and postgraduate medical training programs. This view has already been strongly asserted in the article by Kim
23 in 2017, which suggested that medical education programs for BF would help medical trainees and students to achieve a basic knowledge of BF, to perform successful BF techniques, and to possess the ability to solve BF-associated difficulties and clinical issues.
This study illuminates the beneficial effects of BFH upon antenatal pregnant women concerning awareness of the importance of human milk, and this kind of comparison study has not been reported yet in Korea.
The number of BFH in Korea is few, a large scale survey could not be performed. And, the number of the pregnant women from BFH are quite smaller than that from non-BFH. These are limitations of this study. If a large and multi-locational study would be performed in the future, more significant results may be warranted.
In conclusion, we found that desirable indices were significantly higher in the respondents who also planned delivery at a BFH in this study. If the BFHI becomes more widespread nationwide and better implemented, the BF rate would likely increase in Korea. The present findings will be useful as a basic source for campaigning in favor of the BFHI in Korea.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download