INTRODUCTION
Scombroid fish poisoning is a foodborne disease associated with ingestion of histamine-contaminated fish of the Scombroidae family (e.g., tuna, sardines, and mackerel).
1 Histamine is generated by bacteria from free histidine in fish that is not kept refrigerated.
2 Scombroid fish poisoning is characterized by allergic reactions including flushing, headache, dizziness, abdominal cramps, and palpitations developing within 20–30 minutes of ingestion; most symptoms resolve within 6–8 hours.
3 As fish consumption has increased, outbreaks of scombroid fish poisoning have become common in many countries.
4 However, this is the first reported outbreak in Korea.
On November 3, 2016, an emergency medical dispatch team (summoned by a school by calling “119”) informed a regional Public Health Center that a large number of elementary school students had been transferred to several hospitals because of acute symptoms. An outbreak control team found that most students had experienced flushing and headache within 2 hours of eating lunch at their elementary school and reported the situation to the Department of Public Health of the Seoul Metropolitan Government. Histamine poisoning was suspected because of the rapid onset of allergic symptoms. An epidemiological investigation was quickly mounted.
Go to :

METHODS
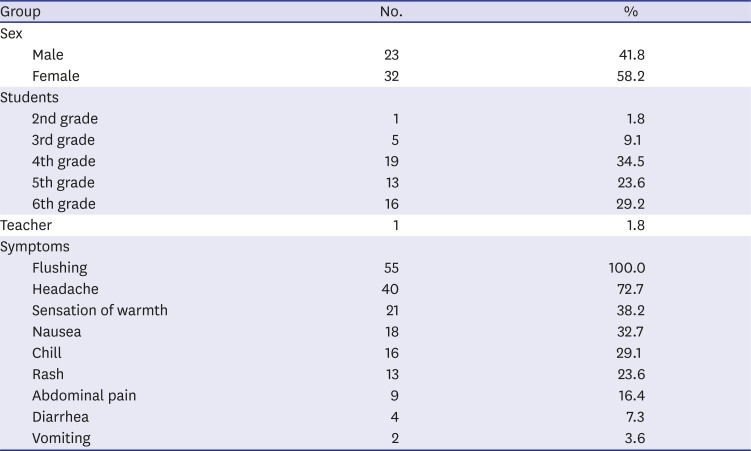
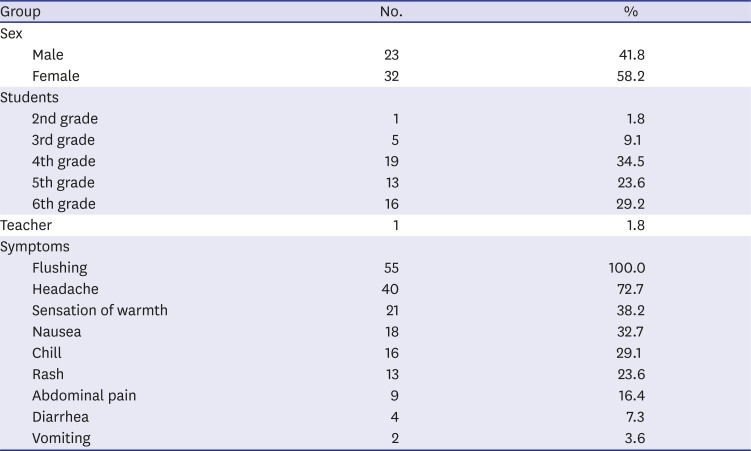
Epidemiological investigation
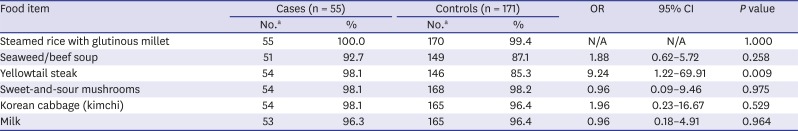
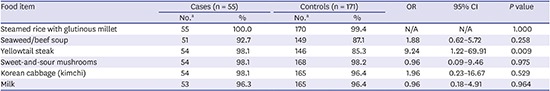
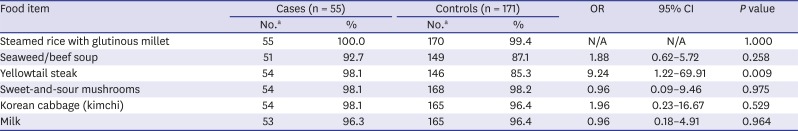
A case-control study was conducted among school members who had eaten lunch in the school. A case was defined as flushing accompanied by symptoms, such as headache, rash, a sense of warmth, chill, and gastrointestinal symptoms (nausea, abdominal pain, diarrhea, and vomiting). For every case, we randomly selected three school members who did not report symptoms after lunch (controls). All cases and controls completed questionnaires exploring demographic characteristics, food items consumed at lunch, and (for cases), symptoms and onset times. Rectal swabs were taken from 63 symptomatic children and 7 food handlers. Samples of food served over the 2 preceding days (including the offending lunch) were collected, and serving utensils were swabbed. Microbiological tests were performed by the Seoul Institute of Health and the Environment. Efforts were made to isolate Salmonella, Shigella, Staphylococcus aureus, Vibrio species, Listeria monocytogenes, Yersinia enterocolitica, Bacillus cereus, pathological Escherichia coli, Clostridium perfringens, and Campylobacter jejuni. Additionally, polymerase chain reactions seeking genomic material of viral pathogens, including rotavirus, norovirus, adenovirus, astrovirus, and sapovirus were performed. Histamine levels in leftover yellowtail fish steak (suspected food item) was measured via high-performance liquid chromatography (using a fluorescence detection method) by the Gyeongin Regional Office of Food and Drug Safety.
Statistical analysis
The relationship between consumption of certain food items and illness was assessed by calculating odds ratios (ORs) with 95% confidence intervals (CIs) with the aid of SPSS software (Version 20.0; IBM Corp., Armonk, NY, USA). A P value ≤ 0.05 was considered to reflect significance.
Ethics statement
This study was not subject to Institutional Review Board review. It was the result of an epidemiological investigation conducted by the local government in accordance with Article 18 of the Act on the Prevention and Control of Infectious Diseases.
Go to :

DISCUSSION
Histamine can be rapidly produced in fish stored at ≥ 20°C, and elevated levels of histamine (> 200 mg/kg) have been reported after food storage for > 15 hours at 20°C–35°C.
5 Histamine is heat-stable (thus not destroyed by cooking); it is essential for maintaining the cold chain.
6 The histamine level in fresh fish is < 0.1 mg/kg
7; however, most outbreaks have been associated with fish histamine levels ≥ 200 mg/kg and often > 500 mg/kg,
8 although some outbreaks were associated with levels < 200 mg/kg.
91011
The present outbreak of food poisoning was caused by histamine contamination; the histamine level in leftover yellowtail steak was > 200 mg/kg, and the cases exhibited the classic symptoms of scombroid fish poisoning. However, the 2017 Korean Guideline for Food Safety Regulation indicates that if consumption of histamine-contaminated food results in an outbreak, this is not an outbreak of food poisoning, as the latter is defined as an incident caused by bacteria, viruses, protozoa, natural compounds (vegetable, animal, and fungal toxins), certain chemicals (hazardous food additives, residual pesticides, metal compounds, and verdigris, lead, and arsenic from cooking utensils and packaging), and some other substances, such as methanol. Thus, scombroid fish poisoning could not be considered as a food poisoning although histamine is a recognized chemical poison. The current protocol for the prevention and management of scombroid fish poisoning clearly requires review.
In the USA, the Food and Drug Administration requires that histamine concentrations (an indicator of decomposition) to not exceed 50 mg/kg, and the European Union stipulates that levels not exceed 100 mg/kg.
12 The New Zealand cutoff is 200 mg/kg in fish or fish products,
13 which is the same as in Korea.
14 When histamine levels exceed these standards in fish or fish products before shipment or distribution, these items are discarded. In this outbreak, the levels in the leftover yellowtail steak were 293 mg/kg. In addition, the levels were above the standard in fish obtained from the supplier. The raw material and processed product were not left in the manufacturing company. According to the guidelines, the histamine test for the safe management of fishery products only applies to domestic fishery products at the pre-distribution stage (production and processing) and imported fishery products at the distribution stage; in addition, yellowtail fish are not included in the items to be inspected for histamine contamination. Therefore, the fish in this outbreak had already been distributed in domestic fishery products, and further testing was not conducted. Because yellowtail fish is a major food item in Korea, it is necessary to supplement the Korean Food Standards Codex so that histamine test items include yellowtail fish.
In this outbreak, the epidemic curve showed that the onset time in several students was longer than 2 hours after eating lunch. This may be because they slept after eating lunch and only noticed the symptoms after awakening. A similar observation was previously reported.
6 This can be explained by the fact that the lunch was discontinued because of the outbreak and the asymptomatic students were instructed to return home early on the day of the outbreak. Compared to previous reports, the attack rate in the present outbreak was very low, perhaps because the other outbreaks were associated with histamine levels > 500 mg/kg.
3 Moreover, yellowtail is rarely associated with scombroid fish poisoning.
4 All previous outbreaks of scombroid fish poisoning have occurred in countries other than Korea. Many countries continuously monitor such outbreaks and institute control measures when high histamine levels are detected in fish products.
1315 In Korea, it is necessary to improve the monitoring system so that outbreaks of scombroid poisoning are reported to the public health authorities.
Food poisoning caused by microorganisms or toxics is distinct from foodborne infectious disease, which has a longer incubation period and can be communicated to other people.
16 However, the initial symptoms may not be distinguishable by public health field workers and a common investigative approach is needed. As soon as the causative agent is identified or suspected, appropriate measures should be taken to prevent further cases. In Korea, the administrative responsibilities for foodborne disease outbreak control are shared by the KMFDS and Korea Centers for Disease Control and Prevention (KCDC). KMFDS restricts the distribution of contaminated food and enhances safety management. If an infectious disease is involved, KCDC conducts contact monitoring and patient management to prevent the spread of the infection.
In conclusion, we report the first outbreak of scombroid fish poisoning in Korea. In recent years, domestic consumption of fish products has increased, and scombroid fish products are supplied to school cafeterias. Therefore, all outbreaks of scombroid fish poisoning must be promptly reported and investigated and detailed food safety regulations are required.
Go to :