This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The sagittal alignment of the spine and pelvis is not only closely related to the overall posture of the body but also to the evaluation and treatment of spine disease. In the last few years, the EOS imaging system, a new low-dose radiation X-ray device, became available for sagittal alignment assessment. However, there has been little research on the reliability of EOS. The purpose of this study was to evaluate the intrarater and interrater reliability of EOS for the sagittal alignment assessment of the spine and pelvis.
Methods
Records of 46 patients were selected from the EOS recording system between November 2016 and April 2017. The exclusion criteria were congenital spinal anomaly and deformity, and previous history of spine and pelvis operation. Sagittal parameters of the spine and pelvis were measured by three examiners three times each using both manual and EOS methods. Means comparison t-test, Pearson bivariate correlation analysis, and reliability analysis by intraclass correlation coefficients (ICCs) for intrarater and interrater reliability were performed using R package “irr.”
Results
We found excellent intrarater and interrater reliability of EOS measurements. For intrarater reliability, the ICC ranged from 0.898 to 0.982. For interrater reliability, the ICC ranged from 0.794 to 0.837. We used a paired t-test to compare the values measured by manual and EOS methods: there was no statistically significant difference between the two methods. Correlation analysis also showed a statistically significant positive correlation.
Conclusions
EOS showed excellent reliability for assessment of the sagittal alignment of the spine and pelvis.
Go to :

Keywords: Pelvis, Whole body imaging, Reproducibility of results, Postural balance
The sagittal alignment of the spine and pelvis is closely related to the overall posture of the body, and it is also important in the evaluation and treatment of spine disease. Thus, much research has been conducted on the sagittal alignment. The sagittal curvature is generally evaluated with whole spine standing lateral (LAT) radiographs.
1234) This method is standard in clinical practice because it is simple and easy to use. Some studies reported good intraobserver reliability of this method.
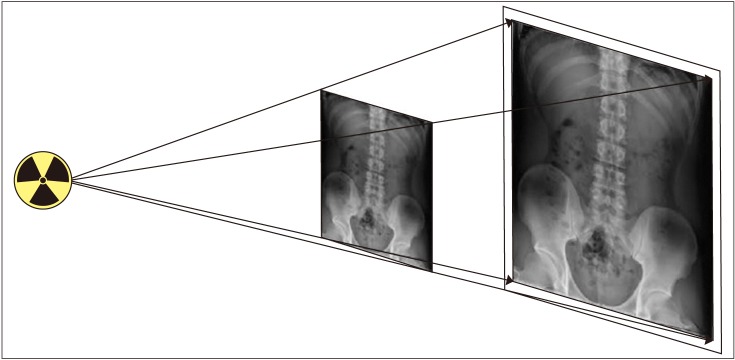
56) However, the conventional radiography system causes distortion between the center and the edges of the radiograph, which increases the risk of size measurement error for structures located far from the central region (
Fig. 1).
7) Also, it is difficult to pinpoint the hip center when measuring pelvic tilt (PT) or pelvic inclination because C7 and T1 vertebral bodies are difficult to identify.
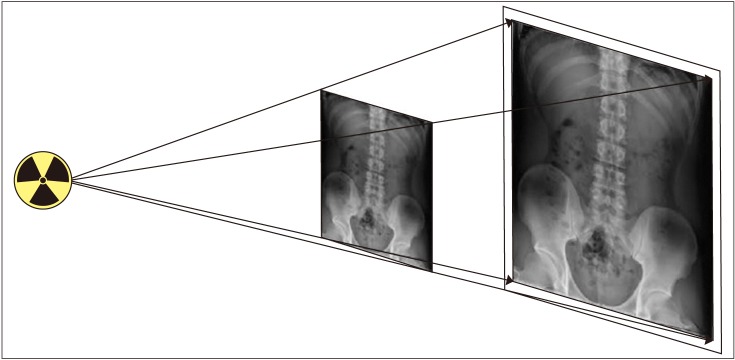 | Fig. 1Distortion caused by conical projection from the center to the edges of radiograph, which increases the scale of error for structures farther from the central region.
|
In the last few years, the EOS imaging system (EOS Imaging, Paris, France), a low-dose X-ray device, became available for orthopedic applications, based on an ultra-sensitive X-ray detection technology that was awarded the 1992 Nobel Prize in Physics.
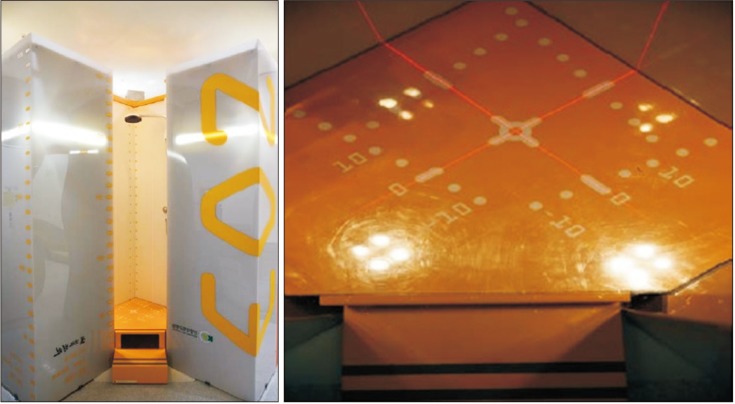
589) EOS is a low-dose biplanar digital radiographic imaging system. The device consists of a side-opening vertical Plexiglas cabin in which the patient is positioned standing erect. The two linear X-ray sources and two gaseous detector arrays move together within the cabin to scan the patient in a standing position in two orthogonal planes (
Fig. 2).
1011) The EOS image is reconstructed as if it was acquired in the patient's reference plane and limits the distortion to the patient's thickness instead of the whole distance between the source and the detector.
7) In particular, EOS is useful when measuring the sagittal alignment on spine and pelvis images by drawing a line along the whole vertebra or calibrating it to the center of both hip joints.
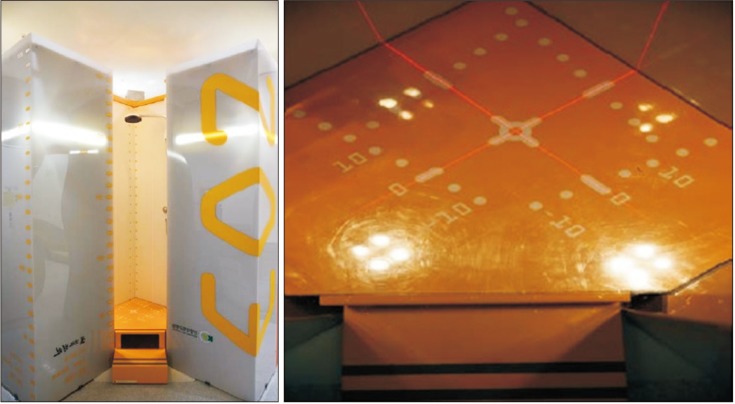 | Fig. 2EOS system cabin to scan the patient in a standing position in two orthogonal planes.
|
There are no gold standards for measurement of the sagittal alignment of the spine and pelvis. However, many researchers have explored methods for more reliable measurement. This study examined the reliability of EOS for measurement of the sagittal alignment of the spine and pelvis as follows: (1) interrater and intrarater reliability in the EOS measurements, (2) interrater and intrarater reliability in the manual measurements, and (3) comparison of the reliability of EOS and manual measurements.
METHODS
Records of 46 patients (17 females and 29 males; mean age, 34.6 years) who were examined from November 2016 to April 2017 by the EOS imaging system were randomly selected and retrospectively reviewed. Clinical records of the patients were also examined. Exclusion criteria were (1) congenital spinal anomaly or deformity and (2) previous history of spine/pelvis operation. Full-body standing orthogonal anteroposterior (AP) and LAT images were acquired using the EOS imaging system in a standard arm position for adequate visualization of the cervical and thoracic spine region.
The patient was asked to stand upright in a weight-bearing position with both hands placed under the eyes on the maxillary sinus and hold breath for 10 to 25 seconds after inhaling while the image of the entire body is taken.
Digital images were stored by the institutional picture archiving and communication system network (STEREOS ver. 1.6.4.7977, EOS imaging). Manual measurements were performed on AP and LAT EOS two-dimensional (2D) images, using the standard clinical picture archiving and communication system workstation software tool (M-view 5.4.10.68; Marotech Inc., Seoul, Korea).
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Konyang University Hospital (IRB No. KYUH 2018-01-022). Written informed consent was obtained.
EOS System
The EOS system is a new slot-scanning radiological device that allows simultaneous acquisition of AP and LAT images. It is composed of two X-ray sources, shaped as fan beams through collimation slits. The sources are coupled to linear detectors built using the micromesh gaseous structure technology.
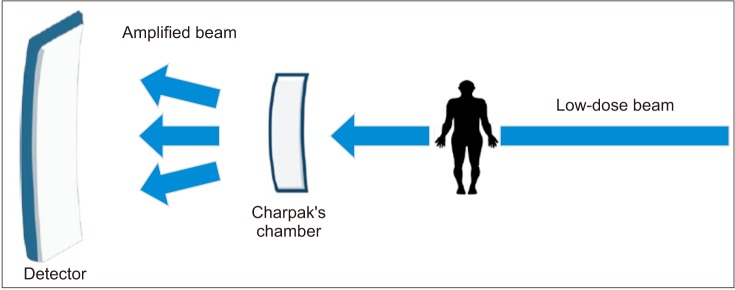
1213) In 1992, professor Georges Charpak was awarded the Nobel Prize for inventing a gas particle detector using a multiwire proportional chamber, and EOS was developed using this technology. In EOS, when a low-dose X-ray beam passes through the subject and the Charpak's chamber, the flow of photons increases in the chamber, amplifying the low-dose X-rays (
Fig. 3).
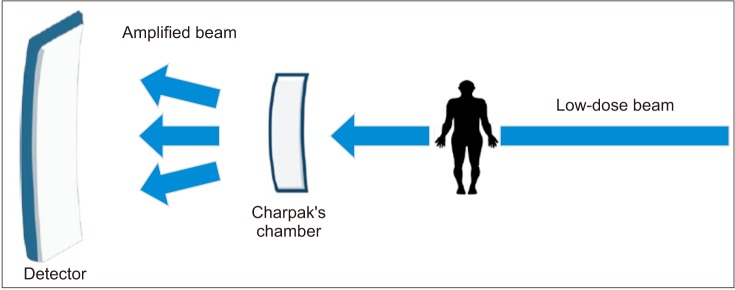 | Fig. 3In EOS, when a low-dose X-ray beam passes through the subject and Charpak's chamber, the flow of photons increases in the chamber, amplifying the low-dose X-rays.
|
The distance between the source and the detector is 1.3 m with the patient standing at approximately one m apart from both sources. The two source-detector pairs are positioned orthogonally, so the patient's frontal and profile images are generated line by line while the whole system is vertically translated. The system also offers the possibility to activate only one source for single view image acquisition. The user determines the starting and finishing heights of the vertical scan; this can minimize radiation exposure to body parts outside the region of interest. For spine examination, the scan time lasts from 8 to 15 seconds, depending on the patient's height. Patients are asked to hold their breath while placing both fingers on the cheek during the scan. Since images are taken simultaneously, there is no movement of the patient between each radiograph. This character benefits techniques such as three-dimensional (3D) reconstruction of bony structures from two radiographic views since their accuracy depends strongly on the spatial correspondence of the structures from one view to the other.
121415)
Selecting the Items of EOS Measurements
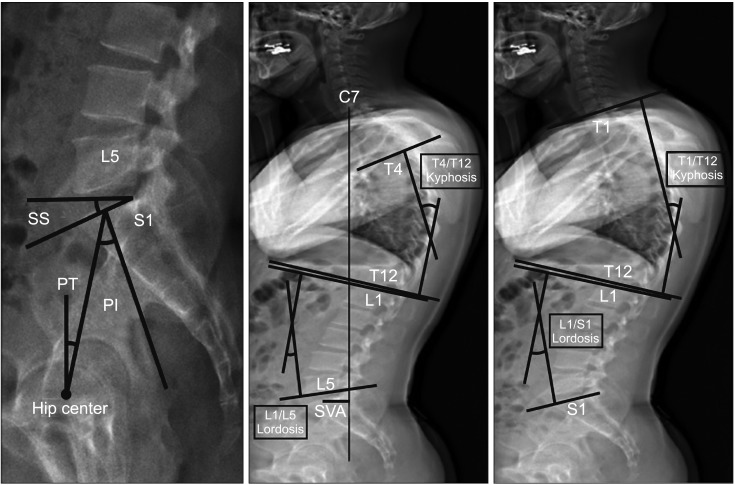
Measurement parameters were selected from basic EOS setting and consensus by the orthopedic surgeons (TGK and JSL) and a radiologist (SEL). We intended to include as many parameters as possible. To clearly assess the reliability, we decided that T1/T12 kyphosis and T4/T12 kyphosis are important pelvic parameters for the following reasons: (1) it is difficult to precisely capture the hip center on sagittal images because the images overlap each other and (2) T1 and T4 are difficult to measure because they overlap with surrounding chest wall structures. Overall, eight measurements were chosen for evaluation. The following eight items were measured through the EOS image system: pelvic incidence (PI), sacral slope (SS) and sagittal PT, sagittal vertical axis (SVA), T1/T12 and T4/T12 kyphosis, and L1/S1, and L1/L5 lordosis (
Fig. 4).
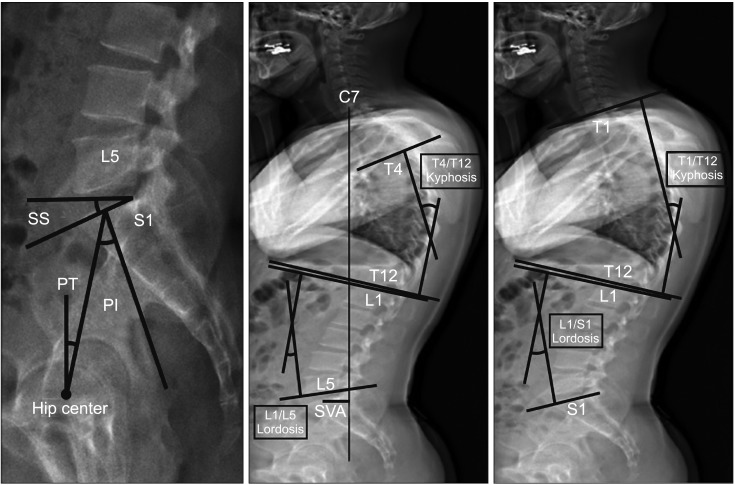 | Fig. 4The following eight items were measured using the EOS imaging system: pelvic incidence (PI), sacral slope (SS), sagittal pelvic tilt (PT), sagittal vertical axis (SVA), T1/T12 and T4/T12 kyphosis, and L1/S1 and L1/L5 lordosis.
|
Measurement Method of Each Parameter
We obtained standing AP and LAT images including the cervical/thoracic/lumbar spine and hip joint and created images by an EOS 2D/3D system (EOS Imaging). Digital images were stored in the institutional picture archiving and communication system network (Marosis v5.4.10.68; INFINITT Healthcare, Seoul, Korea).
On the manual measurement method, the researchers directly measure the obtained images using the standard picture archiving and communication system workstation software tool (Aspyra Access Net Med View v6.2; Aspyra LLC, Jacksonville, FL, USA). The C7, T1, and hip joint parts can be difficult to measure because there are overlapping points. On the EOS measurement method, the obtained EOS images are stored in the main computer inside the workstation. Then, an EOS radiologist adjusts images by the reference point of the EOS software. For images that overlap with each other at the hip joint, C7, and T1, calibration unction can be used for clear visualization.
We measured the following parameters in this study using the manual method and the EOS software tool method. Pelvic parameters were measured by the PI, SS, and sagittal PT. The sagittal balance was assessed by the SVA, T1/T12 and T4/T12 kyphosis, and L1/S1 and L1/L5 lordosis. The PI was defined as the angle between a line drawn from the center of the hip axis to the center of the superior endplate of S1 and a line perpendicular to the endplate.
1116) The SS was defined as the angle formed between the superior endplate of S1 and a horizontal line. The PT was defined as the angle between a vertical line and a straight line connecting the center of the superior endplate of S1 to the center of the femoral head.
The SVA was defined as the distance of the vertical axis between the center of C7 vertebral body and the posterior edge of the sacral plate. The SVA was positive when the vertical axis passing through C7 was anterior to the posterior edge of the sacral plate. T1/T12 kyphosis, T4/T12 kyphosis, L1/S1 lordosis, and L1/L5 lordosis were defined as the angle between the superior end plate of the upper vertebral body and the lower end plate of the lower vertebral body.
Intraobserver and Interobserver Reliability
Three examiners (orthopedic surgeon [TGK], resident [JSL], and radiologist [SEL] with 12, 2, 5 years of each department experience, respectively) measured the eight parameters to assess the intraobserver and interobserver reliability of the EOS. The measurements were performed by the three examiners in three sessions at weekly intervals. Each examiner was blinded to the other measurements and to all patient data. A person who had nothing to do with this study randomly mixed the patient lists and gave them to each of the examiners. Each image was presented to each examiner in random order.
Statistical Methods
The parameters for manual and EOS software measurement methods were analyzed using R package “irr.” The intraclass correlation coefficients (ICCs) and their 95% confidence intervals were used to determine the intrarater and interrater reliability. ICC values of more than 0.75 represent excellent reliability, values between 0.4 and 0.75 represent fair to good reliability, and values less than 0.4 represent poor reliability.
1215)
The relationships between manual measurements and EOS measurements were compared by correlation analysis (Pearson correlation coefficient) and paired
t-test. The Pearson correlation coefficient and the ICC were characterized as poor (0.00 to 0.20), fair (0.21 to 0.40), moderate (0.41 to 0.60), good (0.61 to 0.80), or excellent (0.81 to 1.00). A
p-value of < 0.05 was considered significant.
1217)
Go to :

RESULTS
A total of 46 patients (17 males and 29 females) with mean age of 34.6 years were included in the study.
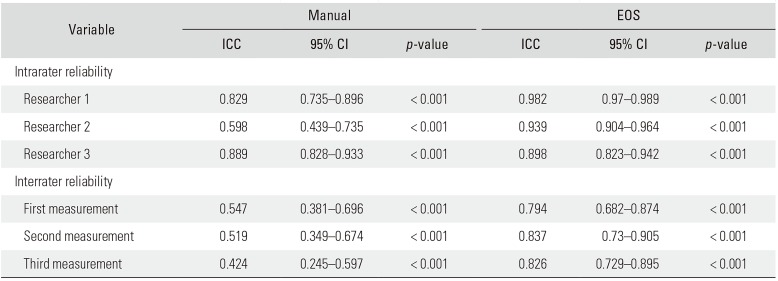
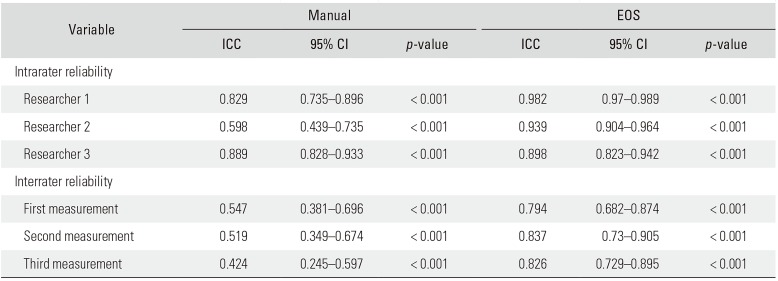
Intrarater Reliability
Except for the intrarater reliability of the manual measurement by the second examiner, the rest showed excellent reliability, with the ICC ranging from 0.598 to 0.889 for the manual measurement method and from 0.898 to 0.982 for the EOS method (
Table 1).
Table 1
Intrarater and Interrater Reliability
|
Variable |
Manual |
EOS |
|
ICC |
95% CI |
p-value |
ICC |
95% CI |
p-value |
|
Intrarater reliability |
|
|
|
|
|
|
|
Researcher 1 |
0.829 |
0.735–0.896 |
< 0.001 |
0.982 |
0.97–0.989 |
< 0.001 |
|
Researcher 2 |
0.598 |
0.439–0.735 |
< 0.001 |
0.939 |
0.904–0.964 |
< 0.001 |
|
Researcher 3 |
0.889 |
0.828–0.933 |
< 0.001 |
0.898 |
0.823–0.942 |
< 0.001 |
|
Interrater reliability |
|
|
|
|
|
|
|
First measurement |
0.547 |
0.381–0.696 |
< 0.001 |
0.794 |
0.682–0.874 |
< 0.001 |
|
Second measurement |
0.519 |
0.349–0.674 |
< 0.001 |
0.837 |
0.73–0.905 |
< 0.001 |
|
Third measurement |
0.424 |
0.245–0.597 |
< 0.001 |
0.826 |
0.729–0.895 |
< 0.001 |

Interrater Reliability
The interrater reliability was fair for the manual measurement method and excellent for the EOS method with the ICC ranging from 0.424 to 0.547 for the former method and from 0.794 to 0.837 for the EOS method (
Table 1).
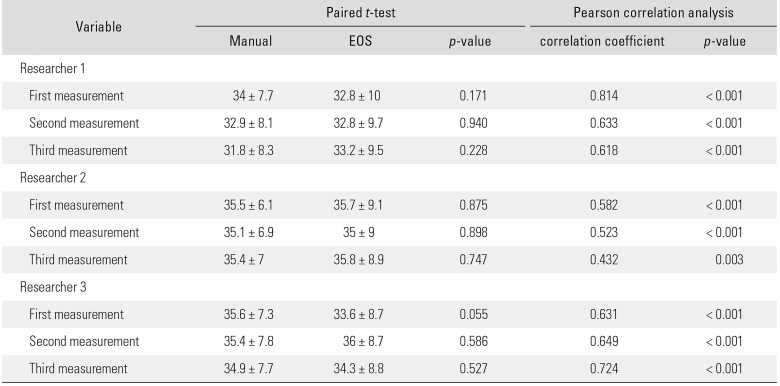
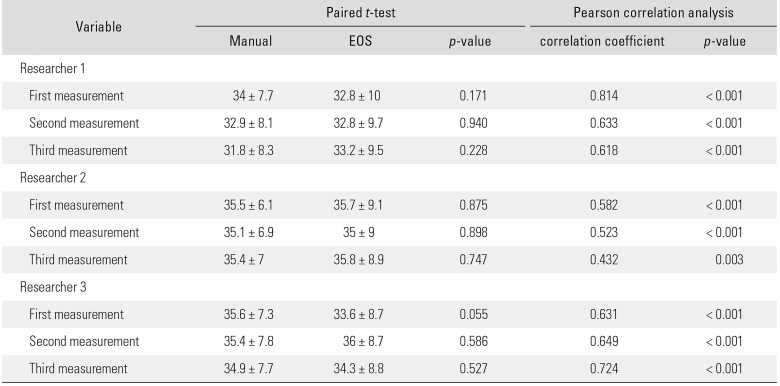
Correlation Analysis: Manual versus EOS
The examiners measured three times each using the manual and EOS methods for the assessment of eight spinal pelvic parameters. The paired
t-test was used to compare the sample size of the two groups. Regarding the spinal pelvic parameters of 47 candidates, there was no statistically significant difference between manual and EOS measurement values with
p-values exceeding 0.05. The examiner 1 and examiner 3 showed good correlations between manual and EOS methods for each parameter. The examiner 2 showed moderate correlations (
Table 2).
Table 2
Correlation Analysis: Manual Measurement versus EOS Measurement
|
Variable |
Paired t-test |
Pearson correlation analysis |
|
Manual |
EOS |
p-value |
correlation coefficient |
p-value |
|
Researcher 1 |
|
|
|
|
|
|
First measurement |
34 ± 7.7 |
32.8 ± 10 |
0.171 |
0.814 |
< 0.001 |
|
Second measurement |
32.9 ± 8.1 |
32.8 ± 9.7 |
0.940 |
0.633 |
< 0.001 |
|
Third measurement |
31.8 ± 8.3 |
33.2 ± 9.5 |
0.228 |
0.618 |
< 0.001 |
|
Researcher 2 |
|
|
|
|
|
|
First measurement |
35.5 ± 6.1 |
35.7 ± 9.1 |
0.875 |
0.582 |
< 0.001 |
|
Second measurement |
35.1 ± 6.9 |
35 ± 9 |
0.898 |
0.523 |
< 0.001 |
|
Third measurement |
35.4 ± 7 |
35.8 ± 8.9 |
0.747 |
0.432 |
0.003 |
|
Researcher 3 |
|
|
|
|
|
|
First measurement |
35.6 ± 7.3 |
33.6 ± 8.7 |
0.055 |
0.631 |
< 0.001 |
|
Second measurement |
35.4 ± 7.8 |
36 ± 8.7 |
0.586 |
0.649 |
< 0.001 |
|
Third measurement |
34.9 ± 7.7 |
34.3 ± 8.8 |
0.527 |
0.724 |
< 0.001 |

Go to :

DISCUSSION
The sagittal balance of the spine and pelvis should be assessed accurately because they are a very important part in the treatment of spinal diseases and outcomes of spinal surgery. So far, whole spine LAT radiography performed in the standing position has been mostly used in the evaluation of the sagittal balance of the spine and pelvis. However, this has been associated with various errors in the assessment of the spine and pelvis. First, there is a possibility of distortion in LAT radiography because split images need to be put together for assessment of the whole LAT view. In addition, depending on the distance between the X-ray light source and the subject, measurement errors can occur after enlargement of images. Thus, it is difficult to perform accurate assessment with general LAT radiography. Second, any movement of the patient during an X-ray may cause a change in the sagittal alignment. Sagittal image acquisition requires a long time during which the patient would have difficulty in holding breath and maintaining the proper posture. Third, the patient is required to raise arms or place them over the chest during LAT X-ray. This inevitably leads to a change in the sagittal alignment. Therefore, it is important to obtain X-ray images precisely and quickly for accurate assessment of the actual sagittal balance.
EOS, first developed in France in 2002, was introduced in Korea in 2017 for the first time. It is a device that allows single-shot X-ray imaging of the spine, pelvis, and lower legs under weight-bearing condition with low-dose radiation exposure. Image acquisition takes 10 to 15 seconds, and it is more accurate than split X-ray.
However, the reliability and accuracy of any new imaging equipment must be checked before use; if values change at each measurement point, the accuracy and reliability of the device is questionable. In addition, the validity of EOS should also be examined. For correct use of a new device, it is necessary to check not only the reliability but also validity. In spite of a high reliability, a low validity indicates meaningful information cannot be expected to be obtained from a device. Therefore, the validity of the EOS should be determined by an approved test that can accurately assess measurements under weight-bearing conditions. In a study by Park et al.,
18) the validity of the method of measuring the height of the patella was evaluated by comparing to magnetic resonance imaging which is a validated test. For EOS, however, no comparable test for determining the validity could be found.
In this study, three examiners performed measurement three times each using manual and EOS methods. The ICC values were higher for the EOS method than the manual method. This should be because C7, T1, and T4 overlap with the shoulder girdle and trunk and pelvic parameters are hidden in the hip center, which limits the accuracy of manual measurement. EOS is also performed at points of measurement selected by an examiner, but it is calibrated by the EOS's own software, so the ICC would be higher than manual measurement. The ICCs of examiner 1 and 3 were higher in manual measurement than examiner 2, which may be related to the measurement experience and proficiency: the examiner 2 had 2 years of orthopedic experience and was less experienced than the other examiners. However, EOS showed high ICC values, and the calibration function of EOS seems to have a significant effect on the reliability of the measurement.
On comparison of the EOS measurement method and manual measurement method with the paired t-test, the p-values for both were larger than 0.05, showing no significant difference between values obtained using the two methods. However, ICC values were higher for the EOS method, indicating it is more reliable than the manual measurement. The correlation coefficients between the two methods ranged from 0.432 to 0.814, and there was a strong positive correlation between the two methods with a p-value of < 0.001, except for one measurement result.
The limitations of this research can be largely categorized into the following two aspects: limitations of the EOS device itself and limitations of the study. EOS devices are helpful for assessment of the alignment of the skeleton in good resolution as well as the parts that are not visible in normal X-ray and measurement. However, measurement errors may occur depending on the skill of the measurer who determines positions and marks reference lines. In addition, EOS is not useful for soft tissues such as muscles, spinal cords, and nerves, and 3D configuration is not possible for the patella and ribs. For elderly patients or neurologically impaired patients, it is difficult to maintain a proper position during an X-ray. Unlike computed tomography, axially oriented fault surfaces cannot be identified. The limitations of the study include the small sample size, the short study period, and lack of a validity test.
We assessed the sagittal alignment of the spine and pelvis using the EOS system to determine the reliability of this new radiographic device. The EOS system showed a higher correlation than the manual method for each examiner and excellent reliability in measuring the sagittal alignment of the spine and pelvis.
Go to :

ACKNOWLEDGEMENTS
The authors are grateful to Seo Eun Lee (Department of Radiology, Konyang University Hospital, Daejeon, Korea) and Jae Sin Lee (Department of Orthopedic Surgery, Konyang University Hospital) for their dedicated help.
Go to :

Notes
Go to :

References
1. Lee CS, Chung SS, Kang KC, Park SJ, Shin SK. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976). 2011; 36(25):E1648–E1654. PMID:
21394071.

2. Korovessis PG, Stamatakis MV, Baikousis AG. Reciprocal angulation of vertebral bodies in the sagittal plane in an asymptomatic Greek population. Spine (Phila Pa 1976). 1998; 23(6):700–704. PMID:
9549792.

3. Van Royen BJ, Toussaint HM, Kingma I, et al. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur Spine J. 1998; 7(5):408–412. PMID:
9840475.

4. Vedantam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine (Phila Pa 1976). 1998; 23(2):211–215. PMID:
9474728.

5. Somoskeoy S, Tunyogi-Csapo M, Bogyo C, Illes T. Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J. 2012; 12(11):1052–1059. PMID:
23102842.
6. Kuklo TR, Potter BK, Polly DW Jr, O'Brien MF, Schroeder TM, Lenke LG. Reliability analysis for manual adolescent idiopathic scoliosis measurements. Spine (Phila Pa 1976). 2005; 30(4):444–454. PMID:
15706343.

7. Deschenes S, Charron G, Beaudoin G, et al. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976). 2010; 35(9):989–994. PMID:
20228703.
9. Dubousset J, Charpak G, Dorion I, et al. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005; 189(2):287–297. PMID:
16114859.
10. Escott BG, Ravi B, Weathermon AC, et al. EOS low-dose radiography: a reliable and accurate upright assessment of lower-limb lengths. J Bone Joint Surg Am. 2013; 95(23):e1831–e1837. PMID:
24306706.
11. Wybier M, Bossard P. Musculoskeletal imaging in progress: the EOS imaging system. Joint Bone Spine. 2013; 80(3):238–243. PMID:
23177915.

12. Lee KM, Chung CY, Park MS, Lee SH, Cho JH, Choi IH. Reliability and validity of radiographic measurements in hindfoot varus and valgus. J Bone Joint Surg Am. 2010; 92(13):2319–2327. PMID:
20926727.

13. McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996; 1(1):30–46.

14. Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002; 21(9):1331–1335. PMID:
12111881.

15. Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York, NY: Wiley;1981.
16. Dubousset J, Charpak G, Skalli W, de Guise J, Kalifa G, Wicart P. Skeletal and spinal imaging with EOS system. Arch Pediatr. 2008; 15(5):665–666. PMID:
18582707.
17. Campos S, Zhang L, Sinclair E, et al. The palliative performance scale: examining its inter-rater reliability in an outpatient palliative radiation oncology clinic. Support Care Cancer. 2009; 17(6):685–690. PMID:
18946683.

18. Park MS, Chung CY, Lee KM, Lee SH, Choi IH. Which is the best method to determine the patellar height in children and adolescents? Clin Orthop Relat Res. 2010; 468(5):1344–1351. PMID:
19629604.

Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download