This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Advances in surgical techniques, implant technology, radiotherapy, and chemotherapy have increased the recovery chances of patients with bone sarcomas. Accordingly, patients' expectations on life quality have also increased, highlighting the importance of objective evaluation of the functional results of reconstruction.
Methods
Thirteen patients with distal femoral endoprosthesis, who had been followed for an average of 2.9 years were evaluated. Postural stability, daily energy expenditure, muscle power, and range of motion were the four parameters analyzed in this study. The Musculoskeletal Tumor Society (MSTS) score and Toronto Extremity Salvage Score (TESS) were used to assess postoperative function and examine correlations with other parameters.
Results
Patients had sedentary activities in 84% of their daily lives. They exhibited a slower speed in the walk across test and a higher sway velocity in the sit-to-stand test (p = 0.005). MSTS scores were significantly correlated with the daily energy expenditure and walking speed.
Conclusions
Objective functional results acquired from various clinics will provide significant data to compare reconstruction techniques, rehabilitation protocols, and surgical techniques. In this way, it will be possible to satisfy the expectations of patients that increase in relation to enhanced recovery.
Go to :

Keywords: Endoprostheses, Femur, Range of motion, Energy expenditure
The distal femur is the area where primary malignant bone tumors such as osteosarcoma, chondrosarcoma, and local aggressive bone tumors like giant cell tumors are seen. Developments in surgical techniques and diagnostic visualization have highlighted the option of surgery for salvage of the extremity. Therefore, resection is the golden standard in surgical treatment of primary malignant bone tumors located in the distal femur, and it can also be performed for recurrent local aggressive bone tumors. Subsequent to distal femoral resection, biological methods such as vascularized fibula grafts, autografts, allografts, allograft-vascularized fibula combinations and endoprothesis for reconstruction can be used. The most preferred method among reconstruction techniques is endoprosthesis.
1)
Advances in surgical techniques, implant techniques, radiotherapy, and chemotherapy have increased the recovery chances of patients with bone sarcomas, which also lead to higher functional expectations of patients. For evaluation of functional results, Musculoskeletal Tumor Society (MSTS) Score and Toronto Extremity Salvage Score (TESS) are mostly used.
2) To satisfy the increased functional expectations, objective evaluation methods are required.
Postural stability is a parameter used for functional evaluation of endoprosthesis. For postural stability, it is required that musculoskeletal system and neurological system should work in coordination. Proprioceptive deficit, muscular weakness, and pain disturb postural stability and cause a shift in body balance on foot.
3) The objective of endoprosthesis is to facilitate early mobilization of the patient, to remove the pain, to protect postural stability, and to improve life quality eventually.
Physical activity is identified as body actions occurring after musculoskeletal activity, causing energy consumption. Surveys are frequently used as an indirect measurement method of activity, whereas accelerometers are used as a direct measurement method. Accelerometers are movement detectors used to measure physical activity by recording movements vertically, laterally, and horizontally minute by minute.
4)
Previous studies applied various approaches to evaluate the physical status of patients after endoprosthetic reconstruction.
5) These approaches involved walking analysis, measurement of oxygen consumption as well as calculation of the walking distance by using pedometers. However, these methods have limitations: walking analyses depend on the comments of an evaluator and are time-consuming; measurement of oxygen consumption is an expensive and invasive procedure; and pedometers record movement in only one plane. Therefore, application of additional evaluation methods is required, which will improve the objectivity of the present methods. The major objective of the present study was to introduce three approaches for the evaluation of functional status of patients after endoprosthetic reconstruction: (1) assessment of the range of motion (ROM) and the muscular strength, (2) detection of postural stability, and (3) measurement of daily energy consumption and physical activity level.
METHODS
Study Design and Participants
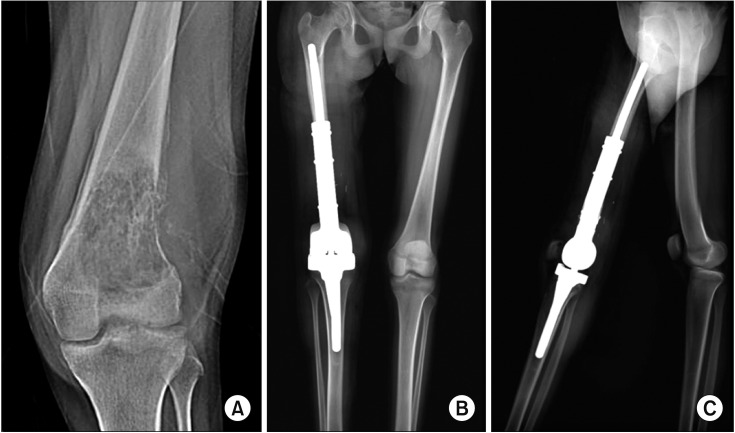
Upon approval of the Ethical Committee (Protocol No. 09.2015.359), data on 37 patients who underwent distal femoral resection and endoprosthetic reconstruction due to a primary bone sarcoma or a recurrent local aggressive bone tumor were retrieved from the orthopedic oncology archive. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The inclusion criteria were determined as patients (1) who are over 15 years old, (2) who have no diabetes, neurological, or cardiovascular disease, (3) who have no length difference over 2 cm between two lower extremities, (4) who can stand for 10 minutes, (5) who can walk at least 6 m without support, (6) who underwent treatment for distant metastasis (no cranial and spinal metastasis), and (7) who underwent the index surgery at least 1 year before the initiation of the study. In addition, the hemoglobin value was over 10 g/dL in the hemogram test of patients in the last 1 month prior to the study. Of the 37 patients, 13 patients met the inclusion criteria. A healthy control group consisted of 20 people who applied to work in outpatient clinics or worked in orthopedic inpatient clinics. Their age and body mass index (BMI) were similar with those of patients. They conformed to the criteria for study. The hinged, silver coated implantcast Modular Universal Tumour and Revision System (MUTARS; Implantcast, Buxtehude, Germany) tumor prosthesis was used without cement after distal femoral resection with the medial longitudinal approach by the same surgeon (BE) in the same center (
Fig. 1).
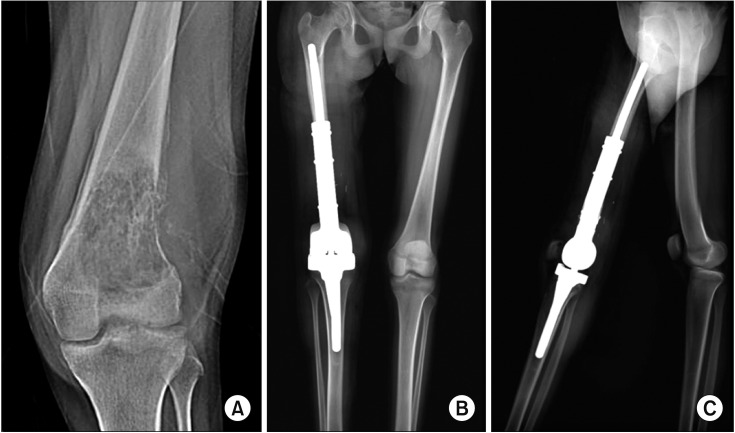 | Fig. 1Preoperative radiograph (A) and 2-year postoperative anteroposterior (B) and lateral (C) radiographs of a 17-year-old patient.
|
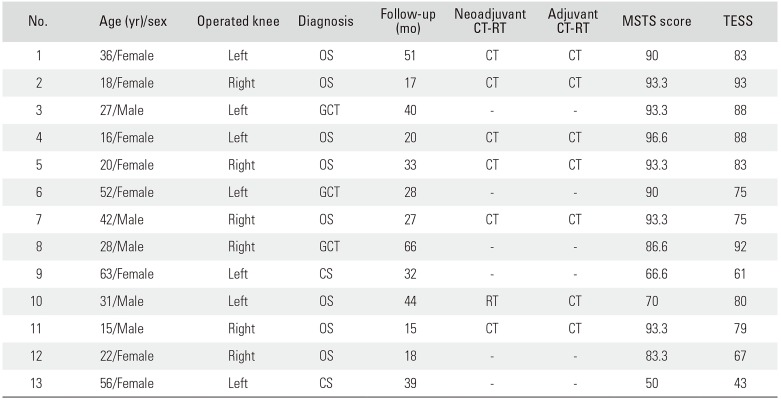
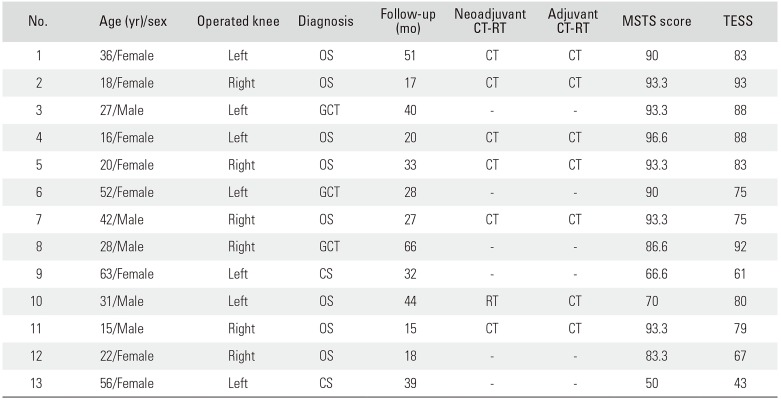
The study population was composed of 13 patients and 20 healthy subjects (control group). The patient group consisted of five males (38.5%) and eight females (61.5%). In the control group, five (25%) were male and 15 (75%) were female. The average age was 32.6 years (range, 14 to 63 years) in the patient group and 29.5 years (range, 15 to 52 years) in the control group. The average follow-up was 33 months (range, 15 to 66 months). The diagnosis was a giant cell tumor in three patients (23.1%), chondrosarcoma in two patients (15.4%), and osteosarcoma in eight patients (61.5%). Seven patients received neoadjuvant and adjuvant chemotherapy. One patient received neoadjuvant radiotherapy. No patient received adjuvant radiotherapy. The operated side was the left side in seven patients and right side in six patients. The dominant side was the right side in all patients and in the control group (
Table 1). There was no foot deformity in patients. At the end of physical examination, it was considered there was no spine deformity, such as scoliosis.
Table 1
Characteristics of Patients at the Time of Measurement
|
No. |
Age (yr)/sex |
Operated knee |
Diagnosis |
Follow-up (mo) |
Neoadjuvant CT-RT |
Adjuvant CT-RT |
MSTS score |
TESS |
|
1 |
36/Female |
Left |
OS |
51 |
CT |
CT |
90 |
83 |
|
2 |
18/Female |
Right |
OS |
17 |
CT |
CT |
93.3 |
93 |
|
3 |
27/Male |
Left |
GCT |
40 |
- |
- |
93.3 |
88 |
|
4 |
16/Female |
Left |
OS |
20 |
CT |
CT |
96.6 |
88 |
|
5 |
20/Female |
Right |
OS |
33 |
CT |
CT |
93.3 |
83 |
|
6 |
52/Female |
Left |
GCT |
28 |
- |
- |
90 |
75 |
|
7 |
42/Male |
Right |
OS |
27 |
CT |
CT |
93.3 |
75 |
|
8 |
28/Male |
Right |
GCT |
66 |
- |
- |
86.6 |
92 |
|
9 |
63/Female |
Left |
CS |
32 |
- |
- |
66.6 |
61 |
|
10 |
31/Male |
Left |
OS |
44 |
RT |
CT |
70 |
80 |
|
11 |
15/Male |
Right |
OS |
15 |
CT |
CT |
93.3 |
79 |
|
12 |
22/Female |
Right |
OS |
18 |
- |
- |
83.3 |
67 |
|
13 |
56/Female |
Left |
CS |
39 |
- |
- |
50 |
43 |

Postoperative Follow-up
Antibiotics were used until drains were pulled out postoperatively. On the first postoperative day, patients were permitted to sit on their beds. On the second postoperative day, they stood up and mobilized with a walker. The brace was locked between 0° and 30°. Passive flexion at 0°–30° was permitted. The drains were withdrawn when there was fluid of 50 mL or below on an average of 3 ± 0.7 days (range, 2 to 5 days) after surgery. After drainage removal, physical treatment was initiated with use of the continuous passive movement device (CPM). The physical treatment was continued until 90° of flexion was achieved with the CPM. In 1 week, active ROM exercises were commenced and progressively increased, which was followed by isometric quadriceps exercises. The average discharge time was 10 ± 1.3 days (range, 8 to 13 days). After discharge, patients were informed that they could continue postoperative rehabilitation with specific exercises. In the period of three months, patients were examined on a monthly basis; afterwards, they were examined semiannually. After 5 years, annual controls were performed. In the first 2 years, magnetic resonance imaging for local control, thorax and abdominal computerized tomography for systemic control were performed. These examinations were performed semiannually after 2 years and annually after 5 years.
Description of Study
This study is a multidisciplinary study conducted in a sport physiology lab, a physical treatment balance analysis room, and an orthopedic outpatient clinic. Patient demographics were recorded. Their BMI was calculated with the standard method: body weight (kg) / height (cm)2. Dominant sides in extremities were recorded. In the orthopedic clinic, the knee joint ROM and muscle power were assessed.
Range of Motion
Knee joint ROM was measured for each patient three times by the same clinician (BE) for both extremities with a universal goniometer with 30 cm arms. Triangulation points of measurements were determined in the manner of American Academy of Orthopedic Surgeons' suggestions.
67)
Muscle Strength
A hand-held dynamometer was used to evaluate the muscular strength of the knee flexor and extensor groups. Lower extremity muscular strengths were assessed separately. Prior to assessment, the requirements for the test were informed to participants. The patient was asked to make maximum muscular contraction against the evaluator's hand.
8) Measurements were made with the “make test” technique where the evaluator upholds the dynamometer in a fixed position, while the participant applies maximum muscular strength. After maximum contraction was acquired, they were asked to stay at that level for 5 seconds. The maximum muscular strength acquired was recorded.
9) The same measurement was iterated three times, and their average value was taken for analysis.
Then patients were sent to a balance laboratory. The MSTS survey was conducted by a physical therapist other than the surgeon to avoid bias. Patients filled out the TESS survey form. Then, four postural stability tests were performed using Balance Master (NeuroCom International, Clackamas, OR, USA).
Postural Stability with Balance Master
This device (dimension, 18″ × 60″) is used to measure the position of the gravity center and postural control caused by vertical forces directed from feet to the strength plate.
Clinical test of sensory interaction on balance
Patients stood up with open and closed eyes on the stable and unstable surface, respectively. In the four test position, computerized analysis of functional balance control and measurement of postural sway velocity was conducted. Duration in which patient stayed in each test position, postural sway velocity, and movement strategy were quantitatively evaluated.
Walk across test
Patients walked on a strength plate (they reached to a normal walking speed before 3 m to platform). The step width, average step length, walking speed and symmetry of step length were recorded. It was aimed to computerize the characteristics of walk with this test.
Step-up-and-over test
A ladder with one stair was deployed on a walking platform. Patients were asked to climb the ladder and stand on the platform again. Parameters (raising index, movement time, and impact index) were recorded separately in both lower extremities. The aim of this test was to computerize the characteristics of motor control (
Fig. 2).
 | Fig. 2Step-up-and-over test on a NeuroCom device. (A) The subject steps onto a stool on one foot. (B) The other foot is put down on the strength plate. (C) The foot on the stool is moved next to the other foot on the strength plate.
|
Sit-to-stand test
This test is to determine the balance capacity to specify the fixed point of the body gravity center of the patient who stands up after sitting. The parameters evaluated were the weight transfer time, raising index, weight center sway velocity, and left-right symmetry. Subsequent to completion of tests in the balance lab, patients were transferred to the sport physiology lab for tests using the Actical accelerometers (Philips Respironics, Bend, OR, USA).
Accelerometer
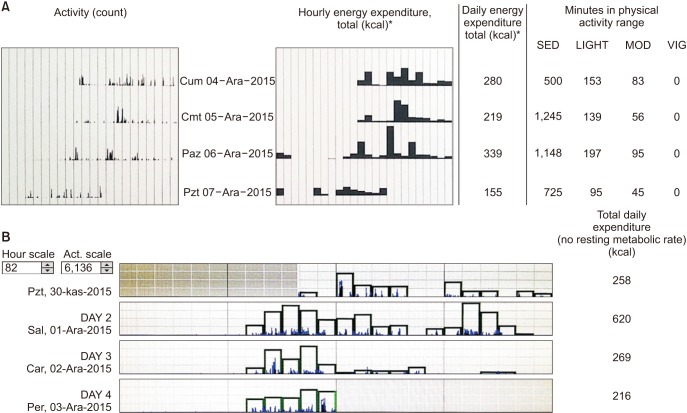
An accelerometer (3 × 3 cm and 16 g; Actical, Philips Respironics) was attached with Velcro around the waist. The patient was asked to hand in the device at the end of 4th postoperative day. Data in the device were transferred into a computer via ActiReader (Philips Respironics). Daily energy expenditure was defined as summation of the basal metabolic rate (calculated automatically by the device based on sex, weight, height, and age) and daily total physical activity. Physical activity and energy expenditure were computerized graphically and numerically (
Fig. 3). Factory defaults of the device were determined by the activity densities' limit values. Cut-off points of the device to differentiate light-moderate activity and moderate-vigorous activity were 0.031 kcal/min/kg and 0.083 kcal/min/kg, respectively. The sedentary state cut-off point was defined as below 0.031 kcal/min/kg. Factory defaults are specified in the literature.
10)
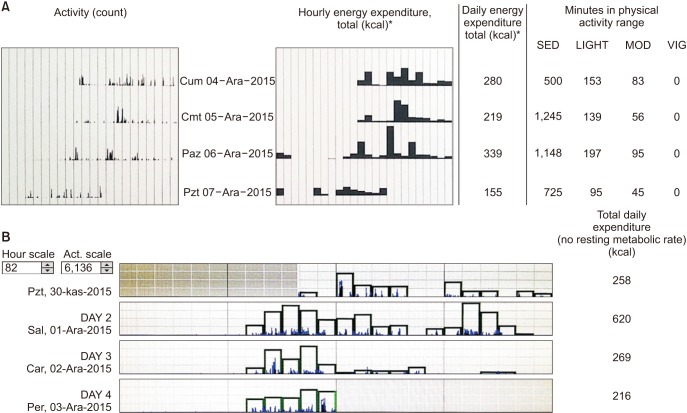 | Fig. 3Computerizing Actical data. (A) Graphical and numerical expression of daily energy expenditure and relationship between time consumed and activity density. (B) In the middle of the 1st day, the device is attached to the patient, and in the middle of the 4th day, the device is retrieved to determine activities and daily energy consumption. SED: sedentary activity, MOD: moderate activity, VIG: vigorous activity.
|
Statistical Analysis
As the data was not normally distributed, the difference between two averages was evaluated with Mann-Whitney U-test. In determination of correlation between constant variables, Spearman correlation was used. As the data was not normally distributed, median and standard deviation (SD) were given together. In the evaluation of data, IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA) was used. A p < 0.05 was considered statistically significant.
Go to :

RESULTS
The average BMI was 26.48 kg/m
2 (range, 17.28 to 32.86 kg/m
2) in the patient group and 24.13 kg/m
2 (range, 15.57 to 32.44 kg/m
2) in the control group, showing no statistically significant difference (
p = 0.074). The average MSTS and TESS scores were 84.5 (range, 50 to 96.6; SD, 13.90) and 77.4 (range, 43 to 93; SD, 13.92), respectively. It was observed that MSTS and TESS scores of patients were positively correlated with each other (
r = 0.61,
p = 0.027) (
Table 1) .
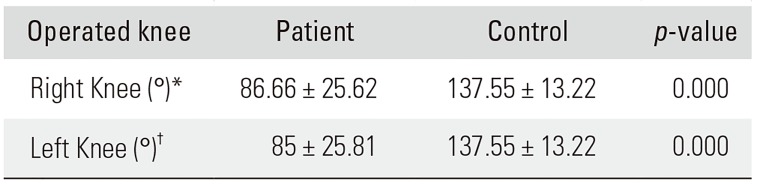
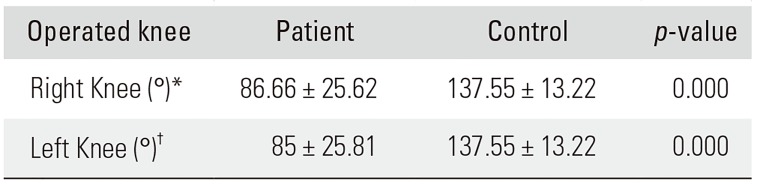
Measurement of ROM
The flexion angle of the right knee was 86.66° (SD, 25.62°) in patients whose right sides were operated and 137.55° (SD, 13.22°) in the control group. The flexion angle of the left knee was 85° (SD, 25.81°) in patients with their left sides operated and 137.55° (SD, 13.22°) in the control group. The extension angle of both knees was zero for patients and the control group. There was no flexion contracture. There was a significant statistical difference between the patient group and the control group in terms of the knee joint ROM (
p = 0.000) (
Table 2).
Table 2
Range of Motion of the Operated Knee in Patients Compared to Healthy Controls
|
Operated knee |
Patient |
Control |
p-value |
|
Right Knee (°)*
|
86.66 ± 25.62 |
137.55 ± 13.22 |
0.000 |
|
Left Knee (°)†
|
85 ± 25.81 |
137.55 ± 13.22 |
0.000 |

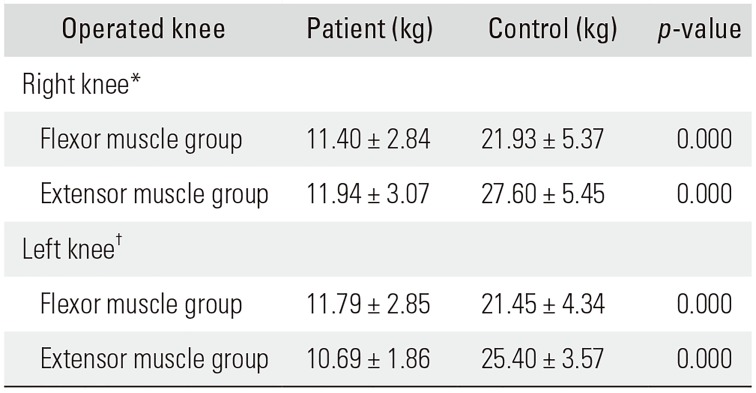
Muscle Strength
The average muscle strength of the right knee flexor group was 11.40 kg (SD, 2.84 kg) in patients whose right sides were operated, and it was 21.93 kg (SD, 5.37 kg) in the control group. The average muscle strength of the right knee extensor group was 11.94 kg (SD, 3.07 kg) in patients whose right sides were operated, and it was 27.60 kg (SD, 5.45 kg) in the control group. The average muscle strength of the left knee flexor group was 11.79 kg (SD, 2.85 kg) in patients whose left sides were operated, and it was 21.45 kg (SD, 4.34 kg) in the control group. The average muscle strength of the left knee extensor group was 10.69 kg (SD, 1.86 kg) in patients whose left sides were operated, and it was 25.40 kg (SD, 3.57 kg) in the control group. Strengths of knee flexor and extensor muscular groups of patients were statistically different from those of the control group (
p = 0.000) (
Table 3).
Table 3
Muscle Strength of the Operated Knee in Patients Compared to Healthy Controls
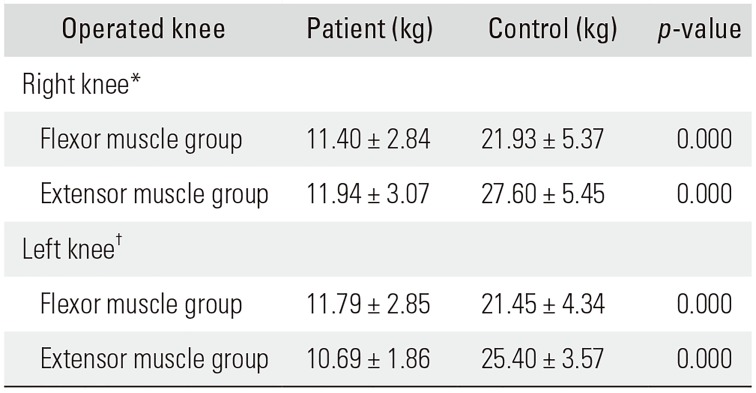
|
Operated knee |
Patient (kg) |
Control (kg) |
p-value |
|
Right knee*
|
|
|
|
|
Flexor muscle group |
11.40 ± 2.84 |
21.93 ± 5.37 |
0.000 |
|
Extensor muscle group |
11.94 ± 3.07 |
27.60 ± 5.45 |
0.000 |
|
Left knee†
|
|
|
|
|
Flexor muscle group |
11.79 ± 2.85 |
21.45 ± 4.34 |
0.000 |
|
Extensor muscle group |
10.69 ± 1.86 |
25.40 ± 3.57 |
0.000 |

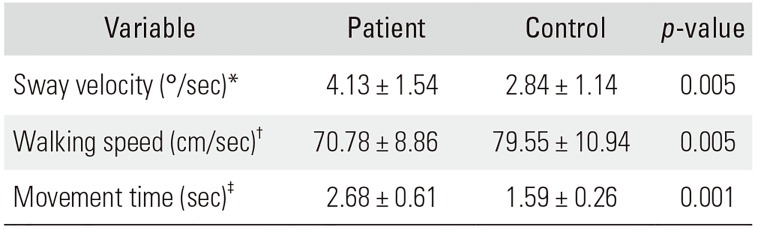
Evaluation of Postural stability
In the sit-to-stand test, sway velocity was significantly higher in the patient group (4.13°/sec ± 1.54°/sec) than the control group (2.84°/sec ± 1.14°/sec;
p = 0.005). In the walk across test, walking speed in the patient group (70.78 ± 8.86 cm/sec) was lower than in the control group (
p = 0.005). In the step-up-and-over test, the average movement time of patients (2.68 ± 0.61 seconds) whose right sides were operated was significantly different from the control group (1.59 ± 0.26 seconds). While one patient whose right side was operated could not perform the test, three patients whose left sides were operated could not perform the test (
Table 4).
Table 4
Postural Stability in Patients Compared to Healthy Controls
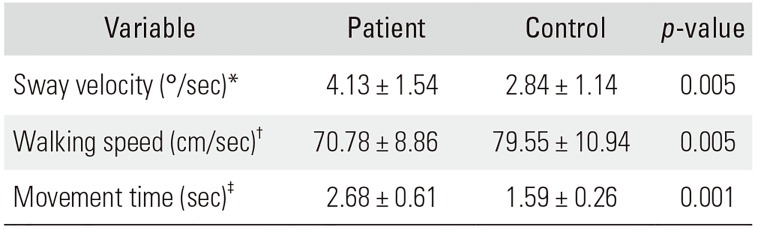
|
Variable |
Patient |
Control |
p-value |
|
Sway velocity (°/sec)*
|
4.13 ± 1.54 |
2.84 ± 1.14 |
0.005 |
|
Walking speed (cm/sec)†
|
70.78 ± 8.86 |
79.55 ± 10.94 |
0.005 |
|
Movement time (sec)‡
|
2.68 ± 0.61 |
1.59 ± 0.26 |
0.001 |

Evaluation of Physical Activity and Energy Expenditure
As the physical activity monitor device was attached to patients between the 1st and 4th days, the average of 2nd and 3rd days was used for analysis. Time passed as sedentary was 2,432.69 minutes on average (84%; SD, 163.59 minutes; range, 2,254 to 2,746 minutes). Duration passed with light activity was 343.84 minutes on average (13%; SD, 130.17 minutes; range, 115 to 572 minutes). Duration passed with moderate activity was 103.46 minutes on average (3%; SD, 69.38 minutes; range, 9 to 236 minutes). No vigorous activity was observed in patients. ActiReader gives two values for energy expenditure. One of them is the daily amount of energy required for a person according to age, sex, height, and weight. The other is the amount of energy spent by the patient in a specific period. These two values were proportional to each other: the energy consumption of patients was 61% (SD, 0.28%; range, 0.13% to 1.08%) of the calculated value for specific age, sex, height, and weight.
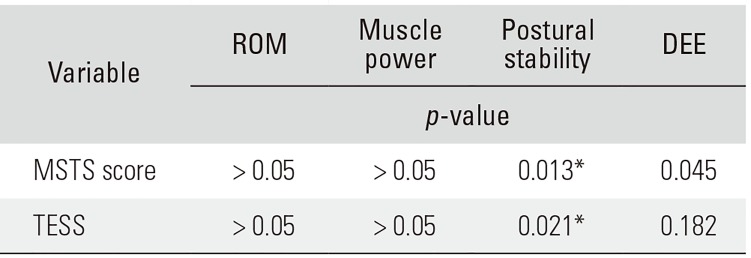
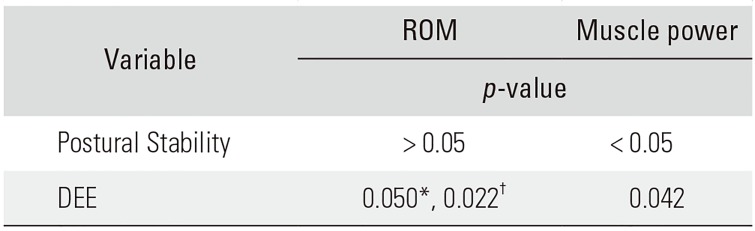
While no correlation was detected between MSTSTESS and ROM (
p > 0.05), muscular strengths were positively corralated with MSTS-TESS (
p > 0.05). When the correlation of MSTS-TESS with tests in which significant difference was observed between the patient group and the control group in the device of NeuroCom was evaluated, there was only positive correlation between MSTS-TESS and walking speed (
p = 0.013 and
p = 0.021, respectively). It was found out that MSTS score and daily energy expenditure was positively corralated (
r = 0.56 and
p = 0.045) (
Table 5). The ROM corralated with neither postural stability nor daily energy expenditure; however, muscle strength was positively corralated with both of them (
Table 6).
Table 5
Relationship between Objective and Subjective Parameters to Analyze Functional Results of Endoprosthetic Reconstruction
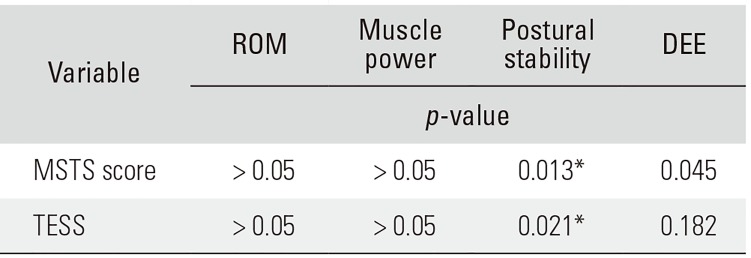
|
Variable |
ROM |
Muscle power |
Postural stability |
DEE |
|
p-value |
|
MSTS score |
> 0.05 |
> 0.05 |
0.013*
|
0.045 |
|
TESS |
> 0.05 |
> 0.05 |
0.021*
|
0.182 |

Table 6
Relationship between Objective Parameters to Analyze Functional Results of Endoprosthetic Reconstruction
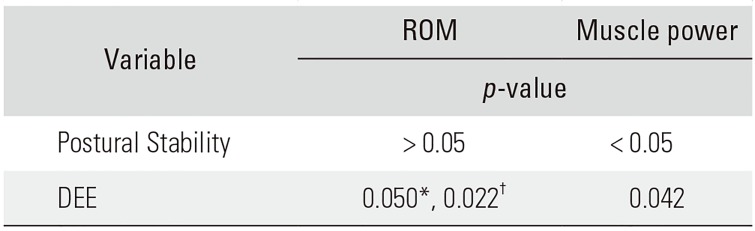
|
Variable |
ROM |
Muscle power |
|
p-value |
|
Postural Stability |
> 0.05 |
< 0.05 |
|
DEE |
0.050*, 0.022†
|
0.042 |

Go to :

DISCUSSION
To the best of our knowledge, this is the first study in the literature that used postural stability and daily energy consumption in the objective assessment of functional results after tumor resection and endoprosthesis. It also compared MSTS and TESS survey forms, frequently used in the evaluation of functional results with objective data.
Walk analysis, oxygen consumption, and pedometers were used in previous studies for objective evaluation.
511) Walk analysis is not a practical objective evaluation method due to intrarater and interrater variability, long evaluation period, and cost.
12) Similarly, pedometers do not fully reflect the daily physical activity by just recording the number of steps.
13) In our study, it was stated that at least 1 year should have passed after surgery for a subject to be included in the study. Various studies have also indicated that at least 1-year period is necessary to minimize inflammation and pain and achieve static balance.
141516)
In the step-up-and-over test, it was found that the patients whose right sides were operated needed more movement time than the control group (p = 0.001). Although the patients whose left sides were operated also needed more movement time than the control group, the difference was not statistically significant (p = 0.486); since three of the patients (43%) whose left sides were operated failed this test, this situation could not be evaluated statistically.
Walking speed was positively correlated with both MSTS (
p = 0.013) and TESS (
p = 0.021). There was a positive intermediate correlation between the MSTS score and daily energy consumption (
r = 0.56,
p = 0.045). Similarly, Rosenbaum et al.
17) has found that there was a low correlation between the MSTS score and the objective physical activity tests. No correlation was found with TESS. MSTS is a subjective evaluation method performed by a clinician. Subjective evaluation methods may not reflect the reality due to patient's expectation and clinician's direction given to the patient.
In the study of Harding et al.,
18) it was indicated that the patients' daily physical activity level after hip and knee arthroplasty was not significantly different from that in the preoperative assessment. The patients' activity level was sedentary for 82% of the time preoperatively; similarly, they were engaged in sedentary activities for 83% of the time in the postoperative period. However, patients subjectively reported that they had improvement in pain and function. In our study, we found that patients spent 84% of the time in sedentary activities after endoprothesis; however, there was no comparison with the preoperative period in the patient group. Similarly, when TESS scores were evaluated, patients said that they were functionally near normal.
In a review article of physical evaluation after knee arthroplasty, Paxton et al.
19) reported that the increase in physical activity was determined in eight of 13 studies; however, in half of them, physical activity was subjectively assessed with a survey. Three studies reported decreased physical activities and two studies reported no change occurred. The common feature of them is that the evaluation was made by an accelerometer. Vahtrik et al.
20) reported that there was no difference between pre- and postoperative leg extensor muscle strength in their patients. Extensor muscle strength of the operated knee was lower than that in the nonoperated side and healthy control group both preoperatively and 3 and 6 months postoperatively. In this study, however, it was not clearly described which side was compared. In patients with malignant bone tumors, measurement of muscular strength before surgery is actually impossible. A difference was detected in both postoperative flexor and extensor muscular strengths in our study. For the extensor group, this could be due to resection as part of the vastus medialis and vastus intermedius. One of the reasons of decrease in flexor muscle strength was coactivation of agonist and antagonist muscle pairs with the decrease in the extensor group muscle power. Another reason could be the use of the hinged type of prosthesis that allows maximum 90° of flexion and adaptation of the flexor muscle mass to these conditions.
In a study of Bernthal et al.,
5) there was a reduction in the knee extensor muscle strength of three groups of patients who underwent replacement surgery of the proximal femur, distal femur, or proximal tibia, for which resection was performed. There was a decrease in the knee flexor muscle strength in the group where only proximal tibial replacement was performed. These results were acquired by comparing with the nonoperated side of the patients. Muscle strength may be lower on the nondominant side. In our study, it was found that both extensor and flexor muscular strengths affecting the knee were low. Comparison for statistical analysis was made with the dominant side of the healthy group. The right side was the dominant side in both the patient group and control group.
In a study including eight patients and eight healthy controls, Okita et al.
21) reported that there was no difference in the walking speed between the resection prosthesis group and the healthy control group. Similar results were reported by Bernthal et al.,
5) in a study of walking analysis in 24 patients including nine who underwent distal femoral resection. In the study, the control group was also composed of eight people, which may be considered insufficient for was statistical analysis. In our study, the walking speed was statistically significantly reduced in the patient group in comparison with the control group. Since our study has 20 people in the healthy control group, our results may have higher statistical power.
In our study, it was found that there was correlation between the flexor and extensor muscular strength that affect knee and postural stability in the patient group, but there was no correlation between the ROM and balance. Therefore, we suggest more importance should be placed on increasing the muscular strength affecting the knee during the period of rehabilitation than on increasing the ROM of knee joint in the postoperative period.
Patients' expectation for recovery has increased in accordance with advances in oncologic treatment and their high expectation for the best adaptation to daily life in the postoperative period indicates the need for more objective evaluation of functional results. Objectively acquired data on functional outcomes will help patients to have proper expectations. Objective functional results acquired from various clinics, notably those related to rehabilitation protocols, will constitute significant data for comparison of reconstruction using various surgical techniques. In this way, it will be possible to satisfy the patients' expectations and increase their survival rates.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download