Abstract
Background
We developed a modified proximal scarf osteotomy technique for moderate to severe hallux valgus in an attempt to obtain better correction of the deformity. In addition, we compared the clinical and radiographic results of this modified technique with those of the classic scarf osteotomy reported in other studies.
Methods
Between December 2004 and July 2009, 44 cases of modified proximal scarf osteotomy was performed in 35 patients with moderate hallux valgus. The American Orthopedic Foot and Ankle Society (AOFAS) score, visual analogue scale (VAS) score, range of motion of the first metatarsophalangeal joint, and radiographic results were evaluated.
Results
The mean hallux valgus angle and the mean first intermetatarsal angle improved from an average of 32.2° and 14.3°, respectively, to an average of 12.5° and 8.6°, respectively. The distal metatarsal articular angle improved from an average of 18.7° to 12.4°. The preoperative mean AOFAS and VAS scores were 47 points and 7 points, respectively, which improved to 86 points and 1 point, respectively, at the final follow-up. Limited range of motion occurred in two cases postoperatively. The height of the first metatarsal-cuneiform joint, which was an average of 15.9 mm preoperatively, did not change. The first metatarsal-talus angle increased from an average of 4.1° to 7.1°.
Conclusions
The modified proximal scarf osteotomy for the treatment of moderate hallux valgus showed similar results with the classic scarf osteotomy with regard to changes in the first intermetatarsal angle and postoperative satisfaction. Therefore, we suggest the modified proximal scarf osteotomy be considered as well as other proximal osteotomy in the treatment of moderate to severe hallux valgus.
Hallux valgus, which is characterized by medial transfer of the first metatarsal bone and lateral transfer of the hallux, refers to the subluxation of the first metatarsophalangeal joint. Surgical treatment of hallux valgus is considered when there is severe ache or deformity due to hallux valgus and it becomes uncomfortable to walk with shoes. Several surgical procedures have been introduced for hallux valgus, and according to the location of the osteotomy of the first metatarsal bone, they are divided into distal, shaft, and, proximal osteotomy. The most common procedure is the proximal osteotomy where the center of rotation of angulation (CORA) is moved to the proximal part and a greater correction is established when the distal area of the metatarsal bone is corrected outwardly. The proximal osteotomy has a greater advantage in terms of correction, but it causes inferior stability of the osteotomy site.1) However, in the scarf osteotomy (shaft osteotomy), screw fixation is performed, and the contact area is widened after correction, thereby resulting in higher stability of the osteotomy site.2) To completely utilize the advantages of the proximal osteotomy and the scarf osteotomy, we moved the existing scarf osteotomy site from the shaft to the proximal part and designated it as a modified proximal scarf osteotomy. In this study, we introduce this modified proximal scarf osteotomy and report the clinical and radiographic results of the technique compared to those of the scarf osteotomy reported in other studies.
From December 2004 to July 2009, 330 cases underwent the scarf osteotomy under the diagnosis of hallux valgus. Of those, 44 cases (35 patients) that underwent the modified proximal scarf osteotomy and were available for at least 2 years of follow-up were included in this study. In the remaining 286 cases (275 patients), the classic scarf osteotomy was performed. There were two males and 33 females. Their mean age was 46 years (range, 14 to 68 years). Nine patients had hallux valgus on both feet, 21 patients on the left foot, and 23 patients on the right foot. The average follow-up period was 65 months (range, 38 to 141 months). Patients who were taking medicine due to severe osteoporosis, those who had external factors such as trauma or tumors, or those who had undergone additional surgical treatment due to deformity of the lesser toe were excluded. We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Eulji Hospital (IRB No. 2017-04-008). Informed consent was waived because of the retrospective nature of the study.
American Orthopedic Foot and Ankle Society (AOFAS)3) first metatarsophalangeal score, visual analogue scale (VAS) score, and range of active motion of the first metatarsophalangeal joint were measured before the operation and at the last follow-up for clinical evaluation.
All patients underwent weight-bearing plain roentgenography of the anteroposterior and lateral sections of the feet before and after the operation. The hallux valgus angle (HVA), intermetatarsal angle (IMA), distal metatarsal articular angle (DMAA), height of the first metatarsal-cuneiform bone, and the first metatarsal-talar angle were measured and compared before and after operation. Patients who were unable to visit the clinic for the last follow-up were evaluated through telephone questionnaires. The changes in HVA and IMA were also measured in the patients with the classic scarf osteotomy and compared with the modified proximal scarf osteotomy group.
A skin incision of about 1.5 cm was made on the dorsal side of the first metatarsophalangeal joint. The superficial intermetatarsal ligament was incised, and the insertion site of the adductor pollicis was incised at the insertion site of the sesamoid and the proximal phalanx. Then, an incision was made in the deep first metatarsophalangeal ligament, and multiple perforation of the dorsal articular capsule was performed. The lateral ligament was released by loosening the external articular capsule. The first metatarsal head was pressed outward, and the hallux valgus was corrected. The medial side of the patients' feet was shifted upward, and a medial skin incision of about 5 cm was made between the first metatarsal-cuneiform joint and the first metatarsophalangeal joint on the medial side of the feet. A T-shaped incision was performed in the medial articular capsules of the first metatarsophalangeal joint and some of the relaxed articular capsules were removed, and then the first metatarsal head was exposed. The osteotomy was performed using an oscillating saw along the imaginary plane parallel to the medial surface of the first metatarsal bone from the sagittal groove of the medial protrusion, and the resected surface was cleaned. A Z-shaped osteotomy line was marked on the medial surface of the first metatarsal bone. The proximal osteotomy site was marked at 5 mm distal to the first metatarsal-cuneiform joint, and the distal osteotomy site was marked at 20 mm proximal to the articular surface of the first metatarsal head (Fig. 1). During the Z-shaped osteotomy, using an oscillating saw, the planes of osteotomy were made parallel to the plantar surface. The distal osteotomy fragment was transferred and rotated outward to reduce the first-second IMA. Two cortical screws were used to fix the two osteotomy fragments (Figs. 2 and 3). The alignment of the great toe was examined during operation, and a wedge-shaped osteotomy was performed in the proximal phalanx to reduce the HVA in 34 cases.4) The excised articular capsules were sutured, and the wound was sutured. A compression gauze bandage was used to maintain a fixed posture. In this study, a proximal chevron osteotomy was performed in patients with severe hallux valgus deformity in whom the first-second IMA was 20° or higher. Partial weight bearing was conducted from the fourth postoperative day using special shoes designed for patients with hallux valgus. Passive and active joint movement of the first metatarsophalangeal joint started 4 weeks after operation. Special shoes were worn for up to 8 weeks after operation, and normal shoes were worn thereafter.
The mean follow-up period was 65 months (range, 38 to 141 months). The average AOFAS score significantly improved from 47 points preoperatively to 86 points postoperatively (p = 0.000). The average VAS score significantly decreased from 7 points preoperatively to 1 point postoperatively (p = 0.000). The range of active motion of the first metatarsophalangeal joint was reduced in two cases (4.5%) after operation.
On the radiological evaluation, the average HVA significantly reduced from 32.2° (range, 20° to 43.6°) preoperatively to 12.5° (range, 18.4° to 10.5°) postoperatively (p = 0.000). The average IMA also significantly decreased from 14.3° (range, 11.9° to 20.9°) before operation to 8.6° (range, 11.4° to 5.5°) after operation (p = 0.000). The average preoperative DMAA of 18.7° significantly decreased to 12.4° postoperatively (p = 0.000). The average height of the first metatarsal-cuneiform joint remained unchanged postoperatively at 15.9 mm (range, 10.8 to 20.7 mm; p = 0.946). The average first metatarsal-talar angle significantly increased from 4.1° (range, 0.3° to 9.3°) preoperatively to 7.1° postoperatively (p = 0.000).
In the patients with the classic scarf osteotomy, the average HVA significantly was reduced from 30.4° (range, 21° to 41.5°) preoperatively to 13.7° (range, 17.5° to 9.8°) postoperatively (p = 0.000). The average IMA also significantly decreased from 13.8° (range, 9.9° to 16.8°) before operation to 8.4° (range, 10.8° to 6.8°) after operation (p = 0.000). There was no statistically significant difference in the changes of HVA and IMA between the patients with the classic scarf osteotomy and the modified proximal scarf osteotomy group.
On postoperative complications, troughing of osteotomy fragments was reported in one case, and three cases showed recurrence of hallux valgus and underwent the operation again. There was no wound infection, nonunion, and fatigue fracture at the osteotomy site. In nine cases (20%), the fixed screws were removed after operation. Of these, six patients' screws were removed while they were undergoing operation on the other feet without any complications. Three patients showed recurrence of hallux valgus, so screws were removed during reoperation.
The scarf osteotomy can be used for horizontal movement, medial rotation, and plantar transfer of the distal bone fragment in hallux valgus as well as shortening and lengthening of the metatarsal bone. It is widely used because it allows for firm screw fixation at the osteotomy site. Additionally, it requires a relatively short postoperative rehabilitation period because of rapid bone union at the large contact area of the osteotomy site.5)
The disadvantage of the scarf osteotomy is that the CORA, which is the correction point of the deformity, is located in the center of the first metatarsal shaft, thereby making the correction less effective than that in the proximal osteotomy.2) To overcome this disadvantage, we performed the osteotomy in the proximal area, not in the center of the first metatarsal shaft as in the conventional scarf osteotomy. The proximal osteotomy site of the classic scarf osteotomy is located at 20 mm distal to the first metatarsal-cuneiform joint,67) and the distal osteotomy site is located at 5 mm proximal to the articular surface of the head of the first metatarsal bone.678) In this study, the IMA improved from an average of 14.3° to an average of 8.6°, the HVA improved from an average of 32.2° to an average of 12.5°, and the AOFAS score improved from an average of 47 to an average of 86. Fuhrmann et al.9) reported midterm results of the scarf osteotomy in hallux valgus. In their study, the AOFAS score improved from an average of 45 to an average of 89, and the IMA improved from an average of 13.8° to an average of 10.7°. The clinical improvement was similar between the studies; however, the mean change in the IMA was higher in the current study. In this study, as the osteotomy was performed in the proximal area, the CORA was moved to the proximal area, and the correction power of the IMA increased. Other studies have reported increased correction power of the IMA using the rotational scarf osteotomy.810) These studies showed similar improvements in AOFAS scores: Adam et al.,8) from 61.5 to 90.3; Murawski et al.,10) from 52 to 92. However, the improvement in IMA was higher in these studies since they performed lateral translation and rotational scarf osteotomy: Adam et al.,8) from 15.8° to 7.2°; Murawski et al.,10) from 18° to 8° (Table 1).
In the current study, there was no statistically significant difference in the change of IMA between the patients with the classic scarf osteotomy and the modified proximal scarf osteotomy group. This may be because the modified proximal scarf osteotomy shifted the bone fragments laterally, not rotating them, although the CORA was moved to the proximal area. In addition, since the patients in this study had moderate to severe hallux valgus, the changes in IMA after operation were not different from those after the classic scarf osteotomy. The IMA may significantly change if the modified proximal scarf osteotomy is applied to patients with severe hallux valgus deformity.
In this study, the height of the first metatarsal-cuneiform joint did not differ before and after operation (average, 15.9 mm) because the Z-shaped osteotomy was performed parallel to the plantar surface, which prevented downward shifting of the metatarsal head. It is advantageous as it prevents any further complications resulting from the downward shifting of the metatarsal head.
The stability after the fixation of the scarf osteotomy was reported to be higher than that of the Chevron and Crescentic procedures.1) Because of the broad osteotomy performed on the metatarsal shaft, the scarf osteotomy is considered inherently stable.1) Barouk5) preferred using one fixation screw in the distal area after the scarf osteotomy, but other authors preferred two screws for stronger fixation. In our study, two screws were used to prevent rotational deformity and to obtain a strong fixation. Complications such as nonunion and loosening of the screws were not reported at the last follow-up. The incidence of the decreased range of motion of the first metatarsophalangeal joint, which is commonly reported as a complication of the scarf osteotomy, is 11%–41.7%.10) To prevent decrease in the range of motion of the first metatarsophalangeal joint, minimal soft tissue manipulation during operation is recommended, as it prevents postoperative adhesion, and also early manual joint motion is encouraged.11) In addition, the presence of arthritis of the first metatarsophalangeal joint is more likely to cause motion disturbance of the joint after hallux valgus operation.9) Because the distal osteotomy site of the existing scarf osteotomy is 5 mm proximal to the head of the first metatarsal bone, the osteotomy also involves the dorsal articular capsule. Some authors checked the articular cartilage by completely resecting the articular capsule or by performing lateral soft tissue dissection.
In this study, to minimize postoperative adhesion, the distal osteotomy site was moved to the proximal area of the articular capsule so that the dorsal articular capsule of the first metatarsophalangeal joint was preserved to the greatest extent. Furthermore, self-joint motion was allowed immediately after operation, and passive joint motion was performed within 4 weeks after operation. Most of the deformities were corrected by osteotomy, and to avoid the tightening of the medial articular capsule, the articular capsule was sutured without tension.
Troughing (penetration of bone fragments through each other) is reported as one of the common complications with an incidence of 1% to 35%.10) Murawski et al.10) presented a technique of rotating the metatatarsal head fragments laterally to reduce troughing. Moving the osteotomy line to the proximal area is considered as a method to reduce troughing because it makes parts of the cortical bone overlap each other in the upper and lower bone fragments. In this study, troughing during operation occurred in one case, but there was no complication such as nonunion after operation.
However, this study has some limitations. This study has a retrospective study design and a small number of cases, and the study results could not be applied to patients with severe hallux valgus deformity. Therefore, it is recommended to compare the results of the modified proximal scarf osteotomy and other proximal osteotomy in patients with severe hallux valgus deformity.
Our results suggest that the modified proximal scarf osteotomy could show excellent results in terms of the correction of the HVA, IMA, and postoperative satisfaction in patients with moderate hallux valgus. Further comparative studies are required to confirm the superiority of this procedure in patients with severe hallux valgus deformity.
Figures and Tables
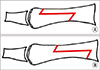 | Fig. 1(A) Osteotomy site in the original scarf osteotomy located at 20 mm distal to the first metatarsal-cuneiform joint and at 5 mm proximal to the first metatarsophalangeal joint. (B) Osteotomy site in the modified proximal scarf osteotomy located at 5 mm distal to the first metatarsal-cuneiform joint and at 20 mm proximal to the first metatarsophalangeal joint. |
 | Fig. 2(A) Anteroposterior X-ray of the foot before the modified proximal scarf osteotomy. (B) Anteroposterior X-ray of the foot after two cortical screw fixations in the modified proximal scarf osteotomy. |
 | Fig. 3Lateral view of the foot after two cortical screw fixations in the modified proximal scarf osteotomy. |
Table 1
Comparison of Results of the Modified Proximal Scarf Osteotomy and Traditional Scarf Osteotomy

| Study | No. of cases | Mean follow-up (mo) | AOFAS score change | IMA average change (°) | HVA average change (°) |
|---|---|---|---|---|---|
| Adam et al.8) | 34 | 18 | 61.5 → 90.3 | 15.8 → 7.2 | 34.6 → 14.9 |
| Fuhrmann et al.9) | 178 | 44 | 45.8 → 89.4 | 13.8 → 10.7 | 39.0 → 24.8 |
| Murawski et al.10) | 140 | 41 | 52 → 92 | 18 → 8 | 37 → 12 |
| This study | 44 | 65 | 47 → 86 | 14.3 → 8.6 | 32.2 → 12.5 |
References
1. Trnka HJ, Parks BG, Ivanic G, et al. Six first metatarsal shaft osteotomies: mechanical and immobilization comparisons. Clin Orthop Relat Res. 2000; (381):256–265.
2. Young KW, Lee KT, Kim JY, Lee HD. Scarf(Z) osteotomy of the first metatarsal shaft in the treatment of hallux valgus. J Korean Soc Foot Surg. 2003; 7(2):157–165.
3. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994; 15(7):349–353.

4. Mann RA. The great toe. Orthop Clin North Am. 1989; 20(4):519–533.
5. Barouk LS. Scarf osteotomy for hallux valgus correction: local anatomy, surgical technique, and combination with other forefoot procedures. Foot Ankle Clin. 2000; 5(3):525–558.
6. Bock P, Lanz U, Kroner A, Grabmeier G, Engel A. The Scarf osteotomy: a salvage procedure for recurrent hallux valgus in selected cases. Clin Orthop Relat Res. 2010; 468(8):2177–2187.

7. Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003; 24(1):29–33.

8. Adam SP, Choung SC, Gu Y, O'Malley MJ. Outcomes after scarf osteotomy for treatment of adult hallux valgus deformity. Clin Orthop Relat Res. 2011; 469(3):854–859.

9. Fuhrmann RA, Zollinger-Kies H, Kundert HP. Mid-term results of Scarf osteotomy in hallux valgus. Int Orthop. 2010; 34(7):981–989.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download