Abstract
Background
Significant discrepancy exists between anatomical plate designs and the anatomy of the native distal radius, which may be attributable to considerable morphometric variations in the volar aspect of the distal radius. We aimed to evaluate the degree of variability in the morphometry of the distal radius and identify factors associated with this variability.
Methods
We measured the volar surface angle (VSA) of the intermediate and lateral columns and the volar surface width (VSW) in the distal radius from three-dimensional computed tomography scans acquired from 81 cadaveric forearms. These morphometric parameters were compared between the lateral and intermediate columns, between males and females, and between Koreans and Caucasians. Caucasian morphometric data were obtained and pooled from the previous studies. The coefficient of variation was used to assess the variability of the parameters and Cohen's d to estimate the effect size of the difference between groups.
Results
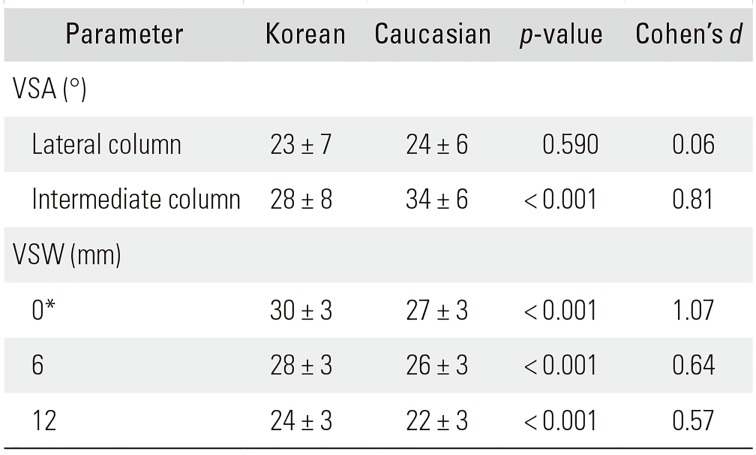
The average VSA of the lateral column was 22° ± 6°, and that of the intermediate column was 29° ± 8° in Koreans (p < 0.001). The variability was high for both VSAs. The VSA of the intermediate column was significantly larger in males than in females (p < 0.001) and in Caucasians than in Koreans (p < 0.001). The average VSW of distal radius was 30 ± 3 mm at the watershed line, and it became narrower proximally. The VSW was significantly larger in males than in females (p < 0.001) and in Koreans than in Caucasians (p < 0.001). The effect sizes of the difference for the VSA and VSW between sexes, races and columns were medium to large.
Conclusions
Considerable variability exists in the morphometry of the volar distal radius, with sex, race, and column as contributing factors. These results suggest that surgeons should carefully choose an anatomical volar locking plate with appropriate angulation characteristics for each patient to achieve patient-specific alignment of the distal radius.
The anatomy of the distal radius is complex. The columnar concept of the distal radius was proposed in 1996 by Dr. Rikli and Regazzoni to simplify the surgical planning of distal radius fractures by dividing the complex geometry of the distal radius into two columns with relatively simple geometry.1) In this conception, the lateral column includes the radial styloid and scaphoid fossa, while the intermediate column includes the lunate fossa and sigmoid notch. The application of two small dorsal plates, one to each column (in accordance with the columnar concept), provides improved outcomes over a single dorsal plate in terms of extensor-related complications.2)
The introduction of the innovative volar locking plate (VLP) in the late 1990s changed the landscape of the surgical treatment of distal radius fractures.3) The use of anatomical VLPs rapidly increased given its advantages over the dorsal counterpart, which include a simple anatomy in the volar distal radius and less tendon irritation because of a thicker soft tissue layer at the plate-tendon interface.4) Numerous studies have reported a fast recovery with good functional and radiographic outcomes after the stabilization of distal radius fractures with a VLP.5678) As VLPs are considered to be anatomically designed, the use of the VLP as a template for the reduction of displaced fracture fragments or the correction of the malunion of the distal radius is a widely employed technique among orthopedic surgeons.
However, several plate design related complications have been reported, such as suboptimal alignment following stabilization,910) with or without subsequent limited motion of the distal radioulnar joint,11) or flexor tendon ruptures.1213) Studies investigating the fit of anatomical VLPs have demonstrated an inadequate fit to the volar surface of the distal radius.1415) Recent anatomical studies employing Caucasian cadavers have demonstrated a significant angular difference between the lateral and intermediate columns, as well as between men and women.161718) It appears that the nonconformity of the plate to the distal radius is caused by inter-individual differences in the distal radius anatomy itself rather than the plate design. However, the degree of variability in the morphometry of the distal radius has not been studied. Understanding the morphometric variation in the distal radius may help surgeons avoid post-surgical complications related to the suboptimal alignment of the distal radius by encouraging surgeons to be prepared for a prompt modification of the anatomical plate during surgery and rely less on the plate design to achieve a patient-specific alignment of the distal radius. The purpose of this study was to evaluate the degree of variability in the morphometry of the distal radius and identify factors associated with the variability.
An anatomical study was performed, investigating the morphometric characteristics of the volar surface of the distal radius in Korean cadavers. A total of 81 Korean cadaveric radii (right, 41; left, 40) from 38 male and 43 female cadavers, with a mean age of 55.3 years (range, 39 to 68 years), were analyzed. All the cadavers had provided written consent during their lifetime to donate their body for research and educational purposes. Radiographs of the wrist were taken before a computed tomography (CT) scan to exclude any bone diseases or fractures. Subsequently, CT images were obtained (176 slices with a slice thickness of 0.75 mm) using a dual-source multidetector CT system (Somatom definition AS+, Siemens Healthcare, Forchheim, Germany). The raw data (in Digital Imaging and Communication in Medicine format) were reconstructed to three-dimensional (3D) images using a 3D software program (MIMICS 13.1; Materialise, Leuven, Belgium) and were converted to stereolithography (STL) files. The STL files were imported into the 3D CAD program (Solid-Works 2013; Dassault Systemes, Waltham, MA, USA) and the volar surface angle (VSA) and volar surface width (VSW) of the distal radius were measured. We chose the VSA and VSW because they were most frequently measured variables in the previous anatomical studies.171819)
To measure the VSA, we defined the centers of the scaphoid and lunate fossa as the meeting point of three curved surfaces, consisting of the volar, dorsal, and lateral/medial articular surfaces of each fossa, respectively. Sagittal section images were then reconstructed along the planes crossing the center of each fossa, which were parallel to the central axis of the distal radius (Fig. 1A and B). The VSA at the lateral column (Fig. 1A) was defined as the angle between the line along the volar surface of the radial shaft and the line along the volar surface of the radial metaphysis in the sagittal reconstruction images at the center of the scaphoid fossa of the radius. The VSA at the intermediate column (Fig. 1B) was similarly measured at the center of the lunate fossa of the radius.1)
The VSW was defined as the length of a line drawn on the volar surface of the radius from the ulnar to the radial margin, perpendicular to the central axis of the distal radius. The VSW was measured from the watershed line to a point 20 mm proximal to the watershed line, in increments of 2 mm (Fig. 1C).
All measurements were conducted twice by one researcher (JHS) and were averaged. The morphometric data of Caucasian radii were pooled from two previous studies,1718) and those of Korean radii were pooled from the present study and one previous study (Table 1).19)
Statistical analyses were performed using IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA). Each morphometric variable was confirmed to follow a Gaussian distribution; thus, parametric tests were performed. Paired sample t-tests were used to evaluate differences between the lateral and intermediate columns. Student t-tests were used to evaluate differences between males and females and between Koreans and Caucasians. Pearson correlation coefficients were calculated to evaluate relationships between demographic and morphometric data. The level of significance was set at p < 0.05. The coefficient of variation (CV) was used to assess the variability in morphometric parameters. The CV is obtained by calculating the standard deviation as a percentage of the group mean; a CV of < 10% is classified as low, 10%–20% is classified as medium, 21%–30% is classified as high, and > 30% is classified as very high.20) Cohen's d, which is the difference between two means divided by the standard deviation, was used to estimate effect sizes; a Cohen's d of ≥ 0.2 is considered small, ≥ 0.5 is considered medium, and ≥ 0.8 is considered large.21)
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (IRB No. 2016-I144). The informed consent was waived because this was a cadaveric study.
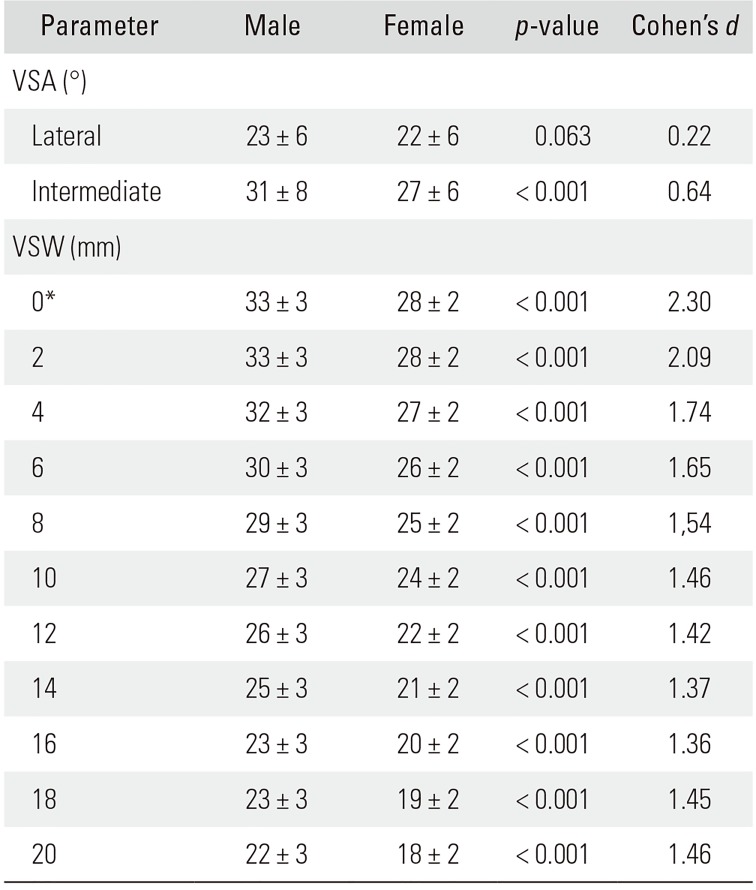
The VSA was significantly greater at the intermediate column than at the lateral column (29° ± 8° vs. 22° ± 6°, p < 0.001) (Table 2). Although males showed a significantly greater VSA than that in females at the intermediate column in Koreans (31° ± 8° vs. 27° ± 6°, p < 0.001) (Table 3), the sex difference was not significant for the VSA at the lateral column (p = 0.063). Caucasians had a significantly greater VSA than that in Koreans (34° ± 6° vs. 28° ± 8°, p < 0.001) (Table 4). The VSA showed high variability, as determined by the CV, and the differences in the VSA between columns and race were large, while the difference between the sexes was medium, as determined by the effect size.
The average VSW of the distal radius in Koreans was 30 ± 3 mm at the watershed line and became narrower proximally. The variability of the VSW was medium as determined by the CV (Table 2). Males had significantly larger VSWs than those in females (p < 0.001) (Table 3), and Koreans had significantly larger VSWs than those in Caucasians (p < 0.001) (Table 4). The differences in the VSW between sex and race were large and medium, respectively, as assessed by the effect size.
Age had a significant, but weak, negative correlation with the VSA at the intermediate column (r = −0.154, p = 0.041), but it did not correlate with the VSW (p > 0.05). Height was significantly correlated with the VSW (r = 0.576, p < 0.001), but it did not correlate with the VSA (p > 0.05).
The recently developed VLPs are considered to have an anatomical design and have been widely used to restore normal alignment following distal radius fractures or malunion. However, a significant discrepancy has been demonstrated between the plate design and the anatomy of the volar surface of the native distal radius.1415) This discrepancy may be attributable to morphometric variations in the volar aspect of the distal radius rather than the plate design. However, the variability in the morphometry of the distal radius is not well understood. In the current study, we demonstrated that the morphometry of the volar aspect of the distal radius has considerable variability, which is associated with column, sex, and race.
Previous studies found a poor fit of the anatomical VLPs to the volar surface of the distal radius. Buzzell et al.14) found that only 3%–6% of contact area existed between the volar surface and seven different types of volar fixed-angle plates when the plates were fixed in their best-fit position. Additionally, Oppermann et al.15) showed that a substantial gap (up to 4.8 mm) was present between the volar cortex of the distal radius and the VLPs when the plates were fixed proximally in their best-fit position. These discrepancies between the plate and distal radius can be explained by the large variability of the VSA demonstrated in the current study. For example, as the standard deviations of the VSA for the lateral and intermediate columns were 6° and 8°, the probability that an angle difference of at least 6° or 8° (which corresponds to a gap of approximately 2–3 mm between the plate and the native distal radius, assuming that the length was 2 cm for the portion of the plate distal to the volar angulation) occurs between the distal radius and the plate is estimated to be 31.8%. In other words, there can be malunion or significant plate protrusion-related complications in approximately one-third of cases, even when a perfect anatomical plate is used. A similar situation has been reported where the use of an anatomical VLP resulted in an excessive palmar tilt with a subsequent limitation of motion in the distal radioulnar joint.11) Therefore, our findings suggest that the multiple size options need to be available to effectively address the anatomical variations of the distal radius, or the plate alignment should be tailored to the patient's specific anatomy during surgery, even when anatomical VLPs are in use.
In the present study, the VSA at the intermediate column was significantly larger than that at the lateral column. This finding is consistent with that of prior studies, in which the VSA at the intermediate column was larger than that at the lateral column by an average of 3° to 10°.16171819) In addition, sex was found to be an important factor contributing to anatomical variation in the distal radius. Sex differences have been reported in previous studies as well; however, the pattern of the differences has been inconsistent. Oppermann et al.15) reported that only the VSA at the lateral column was significantly greater in males than in females, whereas Kwak et al.19) reported that the VSAs at the lateral and intermediate columns were larger in males than in females. In contrast, we found that only the VSA at the intermediate column was significantly greater in males than in females. This inconsistency may arise from heterogeneity in the study designs, racial differences, or type I errors; thus, further research is needed for clarification.
In the current study, we found that there were racial differences in the morphometry of the distal radius. Using the pooled data from three other studies and the present study, we found that Caucasians have a 6° greater VSA at the intermediate column than that in Koreans, which is a large difference. However, Koreans had a significantly greater width of the distal radius than that in Caucasians although the difference was only medium in size. Taken together, the results of the current study indicate that sex and race are significant factors contributing to variability in the anatomy of the distal radius, and these factors need to be considered in the preoperative planning and operating theater to achieve patient-specific alignment of the distal radius. For example, as the plate design is different across different manufacturers, a plate with more volar angulation may be a better choice for Caucasian patients.
The present study has several limitations. First, the mean age of the subjects was in the 50s; thus, the study population may not be representative of the broader Korean population. However, age did not substantially affect the anatomical variation of the distal radius in the present study; thus, aging does not appear to be a significant issue. Second, there could be other potential factors affecting the morphometric variations of the distal radius other than age, sex, or ethnicity. We could not analyze these factors because we could not obtain socioeconomic or medical data of the cadaveric donors. Third, the pooled data might differ from the population data within each race because of the heterogeneity of the study designs and the relatively small number of subjects. Fourth, although the morphometric variation of the volar distal radius was statistically significant and large, the clinical implications remain to be determined. Fifth, we could not provide any practical guidelines to effectively address the substantial morphometric variability in the volar surface of the distal radius. The most accurate method to predict a discrepancy between the plate and the distal radius may be probably to perform a CT scan of the contralateral normal wrist and measure the VSA and VSW. However, this postulation should be tested in the future study. Sixth, we could not find any study reporting on the morphometric variability in the other parts of the body in Koreans, and thus we could not judge whether the volar surface of the distal radius has a significantly different variability compared to the other parts of the body. However, even if the variation of the distal radius morphometry is within the range of natural variations of the body, this does not necessarily mean that the morphometric variation of the distal radius could not be a cause for discrepancy between the plate and the distal radius anatomy.
In conclusion, we found that considerable morphometric variation exists in the volar distal radius and that the factors of sex, race, and column significantly contribute to this variation. The presence of morphometric variation may be one of the causative factors for postoperative complications, such as over-reduction with a subsequent limitation of prosupination or flexor tendon rupture, following the use of anatomical VLPs. These results suggest that surgeons should carefully choose an anatomical VLP with appropriate angulation characteristics for each patient to achieve patient-specific alignment of the distal radius.
ACKNOWLEDGEMENTS
We thank the human data support provided by the Korea Institute of Science & Technology Information (KISTI), which produced these data in collaboration with the College of Medicine, The Catholic University of Korea.
References
1. Rikli DA, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function: a preliminary report of 20 cases. J Bone Joint Surg Br. 1996; 78(4):588–592. PMID: 8682826.
2. Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function: a prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000; 82(3):340–344. PMID: 10813166.
3. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002; 27(2):205–215. PMID: 11901379.

4. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009; 91(8):1868–1873. PMID: 19651943.

5. Richard MJ, Wartinbee DA, Riboh J, Miller M, Leversedge FJ, Ruch DS. Analysis of the complications of palmar plating versus external fixation for fractures of the distal radius. J Hand Surg Am. 2011; 36(10):1614–1620. PMID: 21849236.

6. Sammer DM, Fuller DS, Kim HM, Chung KC. A comparative study of fragment-specific versus volar plate fixation of distal radius fractures. Plast Reconstr Surg. 2008; 122(5):1441–1450. PMID: 18971728.

7. Osada D, Kamei S, Masuzaki K, Takai M, Kameda M, Tamai K. Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg Am. 2008; 33(5):691–700. PMID: 18590852.

8. Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate: a prospective randomized trial. J Bone Joint Surg Am. 2009; 91(7):1568–1577. PMID: 19571078.
9. Mignemi ME, Byram IR, Wolfe CC, et al. Radiographic outcomes of volar locked plating for distal radius fractures. J Hand Surg Am. 2013; 38(1):40–48. PMID: 23218558.

10. Knudsen R, Bahadirov Z, Damborg F. High rate of complications following volar plating of distal radius fractures. Dan Med J. 2014; 61(10):A4906. PMID: 25283615.
11. Jones CW, Lawson RD. One size does not fit all: distal radioulnar joint dysfunction after volar locking plate fixation. J Wrist Surg. 2014; 3(1):42–45. PMID: 24533245.
12. Casaletto JA, Machin D, Leung R, Brown DJ. Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur Vol. 2009; 34(4):471–474. PMID: 19395539.

13. Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011; 93(4):328–335. PMID: 21239658.

14. Buzzell JE, Weikert DR, Watson JT, Lee DH. Precontoured fixed-angle volar distal radius plates: a comparison of anatomic fit. J Hand Surg Am. 2008; 33(7):1144–1152. PMID: 18762111.

15. Oppermann J, Wacker M, Stein G, et al. Anatomical fit of seven different palmar distal radius plates. Arch Orthop Trauma Surg. 2014; 134(10):1483–1489. PMID: 25108754.

16. Evans S, Ramasamy A, Deshmukh SC. Distal volar radial plates: how anatomical are they? Orthop Traumatol Surg Res. 2014; 100(3):293–295. PMID: 24662604.

17. Gasse N, Lepage D, Pem R, et al. Anatomical and radiological study applied to distal radius surgery. Surg Radiol Anat. 2011; 33(6):485–490. PMID: 21136059.

18. Oppermann J, Bredow J, Beyer F, et al. Distal radius: anatomical morphometric gender characteristics. Do anatomical pre-shaped plates pay attention on it? Arch Orthop Trauma Surg. 2015; 135(1):133–139. PMID: 25388864.

19. Kwak DS, Lee JY, Im JH, Song HJ, Park D. Do volar locking plates fit the volar cortex of the distal radius? J Hand Surg Eur Vol. 2017; 42(3):266–270. PMID: 27803378.

20. Leal DH, de Faria Filho DE, Oliveira EM. Classification of the coefficients of variation of parameters evaluated in Japanese quail experiments. Braz J Poult Sci. 2014; 16(2):97–100.

21. Sedgwick P. Randomised controlled trials: understanding effect sizes. BMJ. 2015; 350:h1690. PMID: 25820302.

Fig. 1
Measurement methods of the volar surface angle (VSA) at the lateral column and the intermediate column, as well as the volar surface width (VSW) are shown. (A) The VSA at the lateral column is defined as the angle formed by the line along the volar surface of the radial shaft and the line along the volar surface of the radial metaphysis at the center of the scaphoid fossa. (B) The VSA at the intermediate column is defined as the angle formed by the lines drawn in the same fashion at the center of the lunate fossa. (C) The VSW is defined as the length of the line drawn from the lateral to the medial margin of the volar surface of the distal radius, perpendicular to the central axis of the radial shaft.
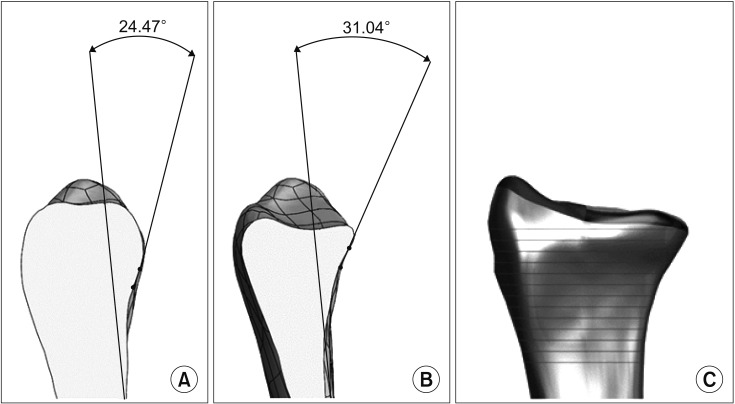
Table 1
Outcomes of Morphometric Studies Pooled for Comparison between Races
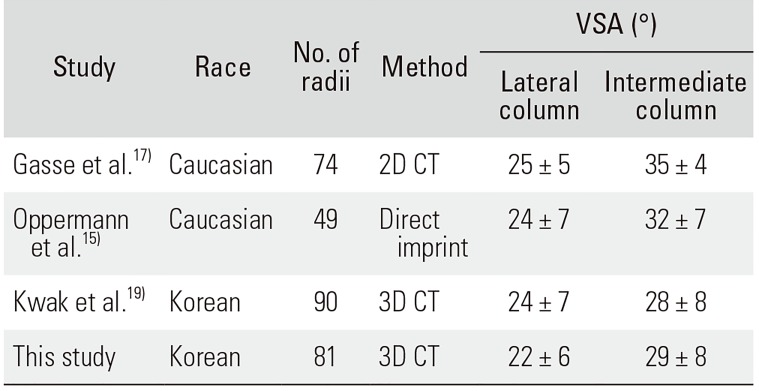
| Study | Race | No. of radii | Method | VSA (°) | |
|---|---|---|---|---|---|
| Lateral column | Intermediate column | ||||
| Gasse et al.17) | Caucasian | 74 | 2D CT | 25 ± 5 | 35 ± 4 |
| Oppermann et al.15) | Caucasian | 49 | Direct imprint | 24 ± 7 | 32 ± 7 |
| Kwak et al.19) | Korean | 90 | 3D CT | 24 ± 7 | 28 ± 8 |
| This study | Korean | 81 | 3D CT | 22 ± 6 | 29 ± 8 |
Table 2
Morphometric Parameters of the Distal Radius in Koreans
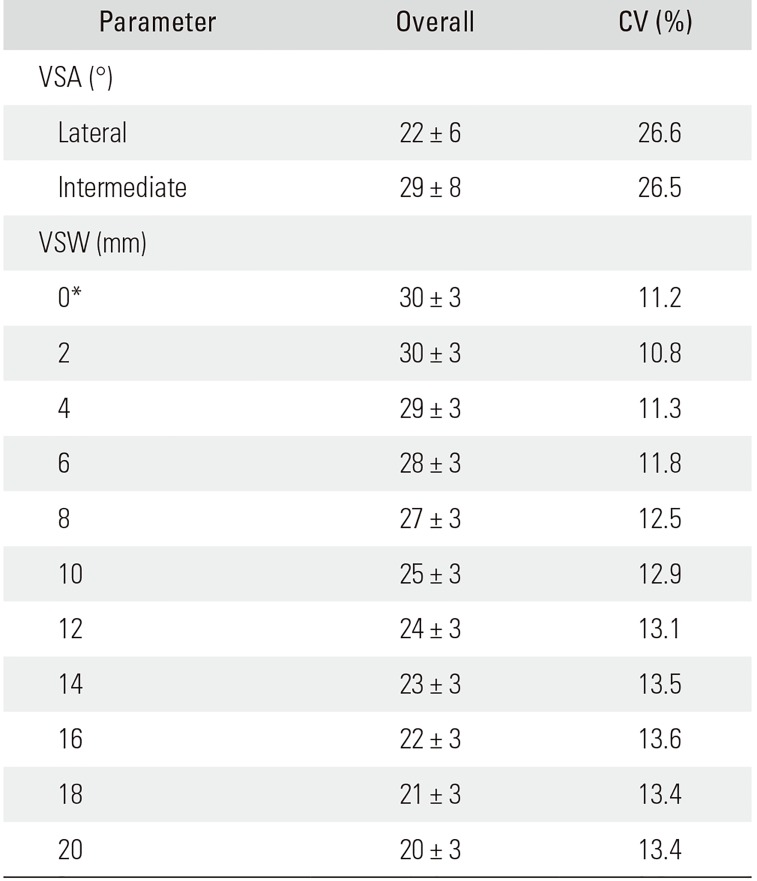
Table 3
Morphometric Parameters of the Distal Radius in Korean Males and Females




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download