Abstract
Background
The purpose of our study was to evaluate the usefulness of hip arthroscopy including extensive capsulectomy for synovial chondromatosis of the hip.
Methods
From 2008 to 2016, 13 patients with synovial chondromatosis of the hip were treated with arthroscopic removal of loose bodies and synovectomy using three arthroscopic portals. An extensive capsulectomy was performed to allow the remaining loose bodies to be out of the extracapsular space, and the excised capsule was not repaired. All patients were assessed by clinical scores and the radiographs were reviewed to determine whether the remaining loose bodies disappeared at the last follow-up.
Results
Eight men and two women were followed up for a minimum of 1 year (mean, 3.8 years; range, 1 to 6.8 years) after hip arthroscopy. Clinical outcomes such as modified Harris hip score, University of California Los Angeles score, and Western Ontario and McMaster Universities Osteoarthritis Index score improved at the last follow-up. Although seven hips had remaining loose bodies after arthroscopic surgery, the remaining loose bodies disappeared in five hips (71.4%) at the last follow-up.
Synovial chondromatosis of the hip is a benign proliferative disease of synovium. It is characterized by many osteochondral loose bodies around the synovium.1234) While the pathogenesis of synovial chondromatosis is unknown,5) this condition presents with pain, mechanical locking, and stiffness of the involved joint.678) Furthermore, if untreated, mechanical damage of the articular cartilage leads to degenerative osteoarthritis of the hip.910) Therefore, surgical intervention is recommended for symptomatic patients with synovial chondromatosis of the hip. Surgical treatment is achieved either by open or arthroscopic removal of loose bodies.11) Open surgery allows for complete access to the joint12) for removal of loose bodies and complete synovectomy. However, open surgery has a risk of complications such as avascular necrosis of the femoral head, iatrogenic femoral neck fracture, and prolonged rehabilitation.1113141516)
Recently, arthroscopic surgery has been introduced to treat intra-articular pathologies including synovial chondromatosis of the hip. Compared to open surgery, arthroscopic surgery was associated with less invasiveness, decreased hospital stay, less postoperative pain, less surgical complications, and faster recovery.101718) Meanwhile, incomplete removal or recurrence is the concern of arthroscopic surgery because complete synovectomy is technically difficult.1119) When loose bodies remain, reoperation is possibly required for patients with persistent symptoms after the surgery.11520) However, there has been no study on the natural course of remaining loose bodies due to incomplete removal after arthroscopic surgery.
The purposes of this study were to evaluate the results of arthroscopic synovectomy and loose body removal for synovial chondromatosis of the hip and to present radiographic changes of the remaining loose bodies due to incomplete removal after arthroscopic surgery.
We retrospectively reviewed 13 patients in whom synovial chondromatosis of the hip were treated with arthroscopic synovectomy and removal of loose bodies at Seoul National University Bundang Hospital between 2008 and 2016. The diagnosis of synovial chondromatosis of the hip was confirmed by magnetic resonance imaging in patients who had characteristic appearance in radiography including numerous intra-articular radiopaque bodies and the absence of substantial arthritic changes.21)
Of the 13 patients, three patients were lost to follow up before a minimum follow-up of 1 year after the operation. The remaining 10 patients (10 hips) were available for complete clinical and radiographic analysis. There were eight males and two females with a mean age of 35.4 years (range, 21 to 58 years) at the time of hip arthroscopy. The mean body mass index was 23.0 kg/m2 (range, 18.3 to 25.9 kg/m2). The mean duration of follow-up was 3.8 years (range, 1 to 6.8 years).
All patients were placed in a supine position on a fracture table with the affected limb in traction. Under general anesthesia, gentle and sufficient traction was applied to the affected limb to distract the joint by 10–12 mm using an image intensifier. During traction, the hip was placed in approximately 5° of abduction and 20° of internal rotation such that the femoral neck was parallel to the ground. All hip arthroscopies were performed by one surgeon (YKL) via three portals (anterior, anterolateral, and posterolateral portals) using 70° angled 5.5-mm arthroscopes. For initial inspection of the hip joint, a 70° angled 5.5-mm arthroscope was inserted through the anterolateral portal, which was created 1 cm distal and 2 cm anterior to the tip of the greater trochanter. The posterolateral portal was placed 1 cm distal and 2 cm posterior to the tip of the greater trochanter. The anterior portal was placed at the intersection of a sagittal line drawn distally from the anterior superior iliac spine and a transverse line drawn from the tip of the greater trochanter. A banana knife or electrocautery was used to enlarge each portal to facilitate maneuvering of the instruments. After establishing the three portals, each portal kept the arthroscopic sheath for rapid interchanging of the arthroscope, various arthroscopic instruments, and an inflow cannula between portals. To obtain a more precise view, 1 mL 0.1% epinephrine solution mixed with every 3,000 mL irrigation fluid was injected via a 5.5-mm inflow cannula, and using a 4.2-mm motorized shaver, electrocautery was performed to resect the torn labrum.
An anterior capsulotomy was made between anterior and anterolateral portals to assess the central compartment. Mainly using a 70° angled arthroscope in the viewing portal, arthroscopic loose body removal and synovectomy were performed through the working portal, the anterior capsulotomy opening. After the traction was released, the arthroscope was moved toward the peripheral compartment through an anterior or anterolateral portal while the hip joint was flexed by around 45°. Then arthroscopic loose body removal and synovectomy were performed. When there were lesions in the medial anteroinferior region or posteroinferior region, anterior capsulotomy was more extended distally to remove any lesions as completely as possible. Most loose bodies could be removed using a probe or grasper, and smaller loose bodies were removed by lavage. In cases where the loose bodies were too large and thus could not be completely removed, the anterior capsule was more excised to get the loose bodies out of the extracapsular space. However, in cases where loose bodies were located at the posterior or posterolateral region of the peripheral compartment in the joint and thus fixed by the synovium, the loose bodies could not be removed. To allow the remaining loose bodies to flow out, the excised capsule was not repaired after the arthroscopic procedure. The removed loose bodies and synovium were sent for histopathological examination. Tolerable range of motion of hips and weight bearing were permitted immediately after surgery.
Routine objective follow-ups were performed at 6 weeks and 3, 6, 9, and 12 months after discharge. We asked all patients about pain, and visual analogue scale scores were used to measure pain. University of California Los Angeles (UCLA) activity scale scores were evaluated at each visit. All patients were assessed using a modified Harris hip score (HHS) preoperatively and at the final follow-up.22) This modified score excluded items of deformity (4 points) and range of motion (5 points) from the original HHS because neither of these is a principle indication for hip arthroscopy. Therefore, the modified HHS included only the pain (44 points) and function (47 points) portions of the original HHS and was adapted to evaluate outcomes of hip arthroscopy as described elsewhere.22) A multiplier of 1.1 provides a total possible score of 100.
Plain radiographs were reviewed for all the patients preoperatively, immediately postoperatively, and at the final follow-up. The preoperative plain radiographs were the anteroposterior views of the hip joint and frog-leg lateral views. We checked for the existence and locations of radiopaque loose bodies preoperatively, immediately postoperatively, and at the final follow-up. The degree of osteoarthritis was evaluated according to the Tönnis classification.23)
Descriptive analysis was used in this study. To compare pre- and postoperative clinical scores, the Wilcoxon signed-rank test was used to analyze statistical significance. A p < 0.05 was considered statistically significant. Statistical analyses were conducted using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol and design of this study were approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1810-499-106), which waived informed consent.
Preoperative radiographs demonstrated radiopaque loose bodies in nine of the 10 hips (90%). According to the Tönnis radiographic classification of hip osteoarthritis, four hips were grade 0, and six were grade 1. Magnetic resonance imaging confirmed intra-articular loose bodies in all 10 hips. All 10 patients underwent arthroscopic procedures including extensive capsulectomy as well as loose body removal. The mean operation time was 144 minutes (range, 75 to 185 minutes). No major complications including neurovascular injury occurred after the arthroscopic procedures. There was one patient with skin problem at the perineum after traction for 2 hours, which healed spontaneously.
The clinical outcomes such as modified HHS, UCLA score, and Western Ontario and McMaster Universities Osteoarthritis Index score improved at the time of the latest follow-up (Table 1). Among nine hips with preoperative radiopaque loose bodies, seven hips had the remaining loose bodies even after arthroscopic surgery. However, the remaining loose bodies disappeared in five hips (71.4%, 5/7) at the last follow-up (Fig. 1). Any osteoarthritic progression was not observed in all hips for the mean follow-up of 3.8 years (range, 1 to 6.8 years). There was no recurrence of synovial chondromatosis.
This study demonstrated that arthroscopic procedures including extensive capsulectomy as well as loose body removal can be effective for synovial chondromatosis of the hip in spite of some remaining loose bodies.
In the treatment of synovial chondromatosis of the hip, removal of loose bodies is essential to relieve pain, prevent recurrence, and delay progression or secondary joint arthritis.10111924) Traditionally, open surgery has been considered as the optimal treatment for synovial chondromatosis of the hip.25) Although arthroscopy has been introduced to treat this disorder, there has been some concern about the feasibility of radical synovectomy, high recurrence rates, and the frequent necessity of reoperation due to remaining loose bodies.18)
The recurrence rates after open surgical treatment for synovial chondromatosis ranged from 0% to 22%.141826) The recurrence rates after arthroscopic treatment for synovial chondromatosis ranged from 7.1% to 16.7%.1519) Although almost all regions of the synovium can be identified during the arthroscopic procedure, it is difficult to remove loose bodies located at the medial portion of the hip joint, as an arthroscope cannot easily reach this area.141527) To completely remove loose bodies, the arthroscopic procedure might require a prolonged traction time, which results in traction-related complications including neuropraxia of the pudendal nerve and perineal skin problems as in one of our patients.28) The mean operation time (144 minutes) in this study might be longer than that of open hip arthrotomy.
In this study, we arthroscopically removed loose bodies and performed synovectomy as completely as possible. To avoid remaining loose bodies, we additionally made an extensive opening at the anterior capsulotomy site. Inaccessible loose bodies located in the medial region could be effectively removed through the opening of the anterior capsulectomy site after surgery; five of seven hips (71.4%) with the remaining loose bodies did not have any loose bodies at the final follow-up. We could not explain the exact reason for disappearance of the remaining loose bodies at the final follow-up. The extensive capsulectomy and wide opening of the anterior capsule might have allowed the loose bodies to be out and absorbed in the extra-articular space. Recently, it has been recommended that the excised capsule be repaired after an arthroscopic procedure to reduce the risk of anterior instability of the hip.29) Fortunately, there was no patient with instability in this study.
There were some limitations in this study. First, this is a retrospective study and the number of patients is too small; however, synovial chondromatosis of the hip is rare condition. Second, we did not have any comparison with an open surgical procedure and arthroscopy with not-extensive capsulectomy. Despite these limitations, considering the reduced risk of serious complications and faster return to daily activities of life, hip arthroscopic procedures including extensive capsulectomy and loose body removal can be useful to treat synovial chondromatosis of the hip.
Figures and Tables
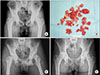 | Fig. 1(A) The preoperative radiograph of a 23-year-old male showed characteristic numerous intra-articular radiopaque bodies in the right hip which was compatible with synovial chondromatosis of the hip. (B) Photograph of removed loose bodies. (C) The immediate postoperative radiograph showed the presence of remaining loose bodies in the medial area of the hip joint. (D) The radiograph taken 6 years after hip arthroscopy including extensive capsulectomy showed that the remaining loose bodies noted on the immediate postoperative radiograph disappeared. |
References
1. Boyer T, Dorfmann H. Arthroscopy in primary synovial chondromatosis of the hip: description and outcome of treatment. J Bone Joint Surg Br. 2008; 90(3):314–318.
3. Raza A, Kailash K, Malviya A. Rare cause of hip pain in a young girl. BMJ Case Rep. 2014; 2014:bcr2014203802.

4. Kose MM, Durmus O, Ayhan MY, Batmaz AG. A rare cause of chronic hip pain: intraarticular synovial chondromatosis. Acta Reumatol Port. 2014; 39(4):349–350.
6. Bloom R, Pattinson JN. Osteochondromatosis of the hip joint. J Bone Joint Surg Br. 1951; 33(1):80–84.

7. Eisenberg KS, Johnston JO. Synovial chondromatosis of the hip joint presenting as an intrapelvic mass: a case report. J Bone Joint Surg Am. 1972; 54(1):176–178.

8. Hamada G. Osteochondromatosis of the hip joint: report of a case. J Bone Joint Surg Br. 1951; 33(1):85–86.
9. Hardacker J, Mindell ER. Synovial chondromatosis with secondary subluxation of the hip: a case report. J Bone Joint Surg Am. 1991; 73(9):1405–1407.

10. Duif C, von Schulze Pellengahr C, Ali A, et al. Primary synovial chondromatosis of the hip: is arthroscopy sufficient? A review of the literature and a case report. Technol Health Care. 2014; 22(5):667–675.

11. de Sa D, Horner NS, MacDonald A, et al. Arthroscopic surgery for synovial chondromatosis of the hip: a systematic review of rates and predisposing factors for recurrence. Arthroscopy. 2014; 30(11):1499–1504.e2.

12. Schoeniger R, Naudie DD, Siebenrock KA, Trousdale RT, Ganz R. Modified complete synovectomy prevents recurrence in synovial chondromatosis of the hip. Clin Orthop Relat Res. 2006; 451:195–200.

13. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001; 83(8):1119–1124.
14. Lim SJ, Chung HW, Choi YL, Moon YW, Seo JG, Park YS. Operative treatment of primary synovial osteochondromatosis of the hip. J Bone Joint Surg Am. 2006; 88(11):2456–2464.

15. Lee JB, Kang C, Lee CH, Kim PS, Hwang DS. Arthroscopic treatment of synovial chondromatosis of the hip. Am J Sports Med. 2012; 40(6):1412–1418.

16. Okada Y, Awaya G, Ikeda T, Tada H, Kamisato S, Futami T. Arthroscopic surgery for synovial chondromatosis of the hip. J Bone Joint Surg Br. 1989; 71(2):198–199.

17. Blitzer CM, Scarano KA. Arthroscopic management of synovial osteochondromatosis of the hip. Orthopedics. 2015; 38(6):e536–e538.

18. Zini R, Longo UG, de Benedetto M, et al. Arthroscopic management of primary synovial chondromatosis of the hip. Arthroscopy. 2013; 29(3):420–426.

19. Startzman A, Collins D, Carreira D. A systematic literature review of synovial chondromatosis and pigmented villonodular synovitis of the hip. Phys Sportsmed. 2016; 44(4):425–431.

20. Ferro FP, Philippon MJ. Arthroscopy provides symptom relief and good functional outcomes in patients with hip synovial chondromatosis. J Hip Preserv Surg. 2015; 2(3):265–271.

21. Robinson P, White LM, Kandel R, Bell RS, Wunder JS. Primary synovial osteochondromatosis of the hip: extracapsular patterns of spread. Skeletal Radiol. 2004; 33(4):210–215.

22. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2010; 468(3):741–746.

23. Tonnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin: Springer-Verlag Berlin Heidelberg;1987.
24. Krebs VE. The role of hip arthroscopy in the treatment of synovial disorders and loose bodies. Clin Orthop Relat Res. 2003; (406):48–59.

25. Marchie A, Panuncialman I, McCarthy JC. Efficacy of hip arthroscopy in the management of synovial chondromatosis. Am J Sports Med. 2011; 39:Suppl. 126S–131S.

26. Witwity T, Uhlmann RD, Fischer J. Arthroscopic management of chondromatosis of the hip joint. Arthroscopy. 1988; 4(1):55–56.

28. Byrd JW. Complications associated with hip arthroscopy. In : Byrd JW, editor. Operative hip arthroscopy. New York, NY: Springer;2005. p. 229–235.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download