This article has been
cited by other articles in ScienceCentral.
Abstract
Trichloroethylene (TCE) is an organic solvent that is used for degreasing and removing impurities from metal parts. However, this solvent's characteristics and hypersensitivity can produce clinical patterns and laboratory data that mimic drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Thus, exposure confirmation is critical to making an accurate diagnosis. This is a case of TCE-induced hypersensitivity syndrome (TCE HS) in a 24-year-old Indonesian man who was working in an electro-plating business. He was admitted to a referral hospital after one month of working, and exhibited a fever with skin symptoms. He was administered immunosuppressive therapy based on an assumed diagnosis of DRESS syndrome, although he subsequently experienced cardiac arrest and did not respond to resuscitation. An investigation into his disease history confirmed that he was prescribed medications one week before he developed the skin disease, and had been periodically exposed to TCE for the previous 4 weeks. Based on these findings, it was believed that his clinical course was caused by TCE HS, rather than DRESS syndrome.
Keywords: Trichloroethylene, Hypersensitivity Syndrome, DRESS Syndrome, Stevens-Johnson Syndrome, Toxic Epidermal Necrolysis
INTRODUCTION
Trichloroethylene (TCE) is a colorless non-flammable organic solvent, which has excellent degreasing abilities, and is mainly used to degrease and remove impurities from metal parts, as well as in various other processes, such as cleaning and dyeing fabrics.
1 Given its solvent characteristics, TCE can be absorbed through inhalation and skin contact, and can cause skin irritation because of its degreasing abilities. However, unlike other organic solvents, TCE can induce systemic symptoms and hyperreactivity accompanying severe dermatitis, such as Stevens-Johnson syndrome or toxic epidermal necrosis.
2 Moreover, the clinical pattern of TCE exposure is very similar to that of drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (i.e., drug-induced hyperreactivity). Hyperreactivity can occur in cases with even minor exposure, and cases of hyperreactivity because of persistent TCE exposure have been reported.
1 Unfortunately, TCE-induced hypersensitivity syndrome (TCE HS) can be misdiagnosed as DRESS syndrome because it has a relatively long latency and is a work-related illness, which makes it difficult for medical staff to identify the exposure history. These features can delay an accurate diagnosis and appropriate treatment. There are 6 reported Korean cases of TCE HS, and the most recent case was reported in 2016.
2345 In our case, the patient's clinical pattern and laboratory data were similar to those of DRESS syndrome, although the interval between drug contact and skin disease development was short. Therefore, this is a case of TCE HS in which the diagnosis was confirmed after examining the patient's work history.
CASE DESCRIPTION
Disease history
A 24-year-old Indonesian man was admitted to the emergency room (ER) of a tertiary referral hospital on August 9, 2015 for erythematous macules on his entire body and a sore throat. Approximately one month earlier, he had been treated at several clinics for itching, fever, and myalgia, although these conditions did not improve. One week before the admission, his condition worsened and he developed rash with generalized edema and exfoliative dermatitis. He was alert when he arrived at the ER, with a blood pressure of 100/70 mmHg, a heart rate of 110/min, a respiratory rate of 20/min, and a body temperature of 39.1°C. The initial laboratory data revealed a white blood cell (WBC) count of 22,170/mm
3 (segmented neutrophils: 32%, eosinophils: 36%, 7,910/mm
3), a red blood cell count of 578/mm
3, hemoglobin levels of 14.5 g/dL, hematocrit levels of 40.0%, a platelet count of 136,000/mm
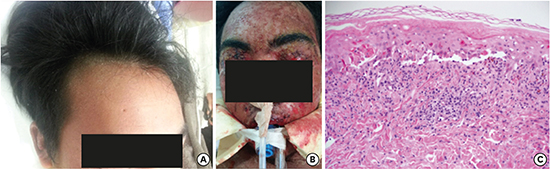
3, aspartate aminotransferase (AST) levels of 69 IU/L, and alanine aminotransferase (ALT) levels of 274 IU/L. The patient had a sore throat and exhibited erythema multiforme, desquamation, and generalized edema throughout his entire body (including the face and oral mucosa) (
Fig. 1). It was not possible to obtain detailed medical or prescription histories, as he was a foreigner, although he notified staff that he had visited clinics before his admission. The medical staff suspected DRESS syndrome, based on his systemic symptoms with exfoliative dermatitis and elevated eosinophil levels, and treated the patient using hydration, antihistamine, and a topically applied steroid ointment.
 | Fig. 1Clinical finding and histologic finding on admission. (A) The patient's forehead at the admission. Rash and scales were observed on his entire body. (B) Day 4 after the admission. His skin symptoms worsened and vesicular and petechial rashes developed on his entire body, with petechial skin lesion invading the eyelids and ocular mucosa. (C) Histologic examination of the skin biopsy. Sub-epidermal bullous change and many apoptotic keratinocytes were observed in the epidermis. These findings were consistent with cutaneous drug-induced reaction (hematoxylin and eosin staining, × 200). 
|
On day 2 after the admission, the patient's body temperature increased to 39.6°C and did not drop below 37°C. Additional testing revealed a WBC count of 13,300/mm
3 (eosinophils: 24.8%), AST levels of 102 IU/L, and ALT levels of 233 IU/L. Thus, the patient was treated using intravenous methylprednisolone (40 mg/day). Histopathologic examination of the skin biopsy revealed sub-epidermal cleft with bulla formation and vacuolar change in the basal layer (
Fig. 1). Characteristic apoptotic keratinocytes and lymphocytic exocytosis were easily observed in the epidermis. There are upper dermal lymphocytic infiltration accompany with abundant extravasated erythrocytes. Also pigment incontinence was identified. And there is no evidence of viral infection. All these histopathologic findings were compatible with cutaneous drug-induced reaction. On day 3, the patient's body temperature remained at > 37°C, and he exhibited worsened skin symptoms with conjunctivitis. Intravenous cyclosporine treatment (250 mg) was initiated with prophylactic antibiotics. On day 4, the desquamation worsened and his body temperature remained at > 39°C. The systemic steroid was discontinued, and cyclosporine was administered with intravenous immunoglobulin. However, the patient lost consciousness at approximately 1 PM, and exhibited worsened vital signs (blood pressure: 80/60 mmHg, pulse: 140/min, respiration rate: 30/min, and body temperature: 39.8°C). Oxygen was administered using a reservoir mask, although his oxygen saturation was 94%. He began receiving intensive care at approximately 3 PM, experienced cardiac arrest at midnight, and did not respond to resuscitation.
Medical history
To identify the occupation-related cause of death, an investigation of the patient's medical history was conducted, and statements were collected from colleagues at his work dormitory. The patient did not have a known medical history when he entered Korea in 2014. He performed polyester-related work for 6 months until March 2015, and was hired by a faucet manufacturer on June 25, 2015. He did not undergo a pre-placement medical examination or regular medical examinations when he joined the present industry. Employers are legally obliged to have their employees undergo a pre-placement medical examination when there is planned exposure to TCE during their work, and are also obliged to have them undergo a first regular health examination related to TCE exposure within six months of the pre-placement medical examination. It is unknown why these examinations did not take place. His TCE exposure resulted from soaking the product in a cleaning tank containing TCE during the electro-plating process. The electro-plating log revealed that he worked routinely each day between June 25 and July 17 in 2015, and he only completed 30 minutes of work and left during work hours on July 20. He subsequently worked on July 27 and 28 for each day. The TCE was frozen in a washing tub to prevent vaporization, and the cleaning process was performed under a ventilation hood. The company had completed air quality testing in the area around his ventilator space every 6 months, and the document revealed that TCE levels did not exceed the Korean permissible exposure limit (the 8-hour time-weighted average) of 10 ppm from 2013 to the first half of 2015. The time-weighted average values for TCE were 5.8224 ppm in July 2015 and 4.0556 ppm in December 2014. However, in the investigation for occupation-related cause of death, the 8-hour time-weighted average values for TCE were 6.294 and 14.770 ppm, respectively, and the maximum TCE concentration were 12.594 and 33.633 ppm, respectively.
According to his colleagues, the patient complained of whole-body itching, pain, and discomfort for weeks after starting the work. A subsequent investigation of his treatment history before the ER admission revealed that he had visited different clinics on July 13 and 14 because of persistent myalgia that had developed one week earlier. On July 13, Clinic A prescribed the patient oral talniflumate with streptokinase and tramadol (50 mg) injections. On July 14, Clinic B prescribed the patient oral acetaminophen, loxoprofen, and eperisone, with injections of a multi-vitamin (Pan-B-Comp; Daihan, Seoul, Korea) and tramadol (50 mg). It could not be verified whether he actually took the prescribed medications. His myalgia did not improve and he subsequently experienced new-onset systemic skin symptoms. He revisited Clinic A on July 20 and was prescribed prednisone, an antihistamine, and a dexamethasone injection (5 mg). On July 22, he revisited Clinic B and was prescribed an H2 blocker, an antihistamine, and prednisone. He took a one-week leave from work, although his systemic and skin symptoms worsened after returning to work on July 27 and 28. He subsequently visited Clinics B and C on August 1 and 3, although his condition continued to deteriorate and his colleagues subsequently brought him to the ER (
Fig. 2).
 | Fig. 2
The course of the exposures and illness. June 25: exposed to TCE. July 13: general symptom appeared and prescribed medication. July 20: systemic skin symptom appeared and prescribed a steroid and antihistamine. TCE exposure was discontinued. July 27: symptom worsened after re-exposure to TCE and treated for general dermatitis over a 10-day period with further TCE exposure. August 9: admitted to the ER with systemic skin symptoms, sore throat, and fever.
TCE = trichloroethylene, ER = emergency room.

|
DISCUSSION
A drug treatment history is critical when treating a patient with exfoliative dermatitis and systemic symptoms. For example, DRESS syndrome is likely if the patient took a drug 3–8 weeks before the symptom occurrence and blood testing reveals hepatotoxicity and eosinophilia. However, TCE HS exhibits similar characteristics and clinical patterns,
1 and TCE exposure should be considered if the patient handled chemical products and/or TCE (e.g., during degreasing, painting, printing, and electroplating).
In the present case, the patient had been exposed to TCE since June 25, and had received the first prescription for systemic symptoms at a clinic on July 13 (18 days post-exposure). On July 20 (25 days post-exposure), and one week after receiving the first prescription, he developed skin symptoms on his entire body. In this context, one week of drug exposure is a relatively short period for a drug-induced immune response, and his prescribed drugs are not commonly associated with DRESS syndrome.
1 Thus, we believe that the patient experienced TCE hypersensitivity.
TCE HS has features that are highly similar to those of DRESS syndrome
1 and the symptoms appear approximately 3–8 weeks after exposure. After the symptoms develop, immediate recurrence and worsening can be induced by even minor exposures.
6 In addition, Huang et al.
7 evaluated 59 patients with skin symptoms that first occurred at an average period of 27.9 ± 9.8 days post-exposure. Furthermore, a Japanese study reported that skin symptoms occurred at 3 weeks post-exposure.
8 Moreover, previous case reports regarding TCE HS have described immediate symptom recurrence and worsening after re-exposure to TCE.
91011 This condition is also greatly influenced by genetics, and a recent study revealed that a group of patients with TCE HS exhibited more HLA-B*1301 alleles, compared to the control group, which suggests a genetic association with the HLA allele (similar to drug hypersensitivity).
12
Given the similarity of clinical features between TCE HS and DRESS syndrome, TCE HS can be misdiagnosed if there is no suspicion of previous TCE exposure. However, if medical staff are aware of TCE HS and its skin symptoms, they can comprehensively examine the patient (or interview work colleagues) during the latency period between the exposure and symptom manifestations. This report focused on the time sequence of TCE exposure, clinic visit, and the symptom appearance because prompt and accurate treatment can prevent worsening of symptoms for both TCE HS and DRESS syndrome. While TCE HS and DRESS syndrome can exhibit different clinical features, early withdrawal of the causative agent(s) is essential for recovery in both scenarios, in addition to systemic corticosteroid therapy in some cases. In this case, there was no improvement with systemic steroids and the patient's condition became worse, ultimately resulting in death.
Therefore, work-related illnesses should be considered in cases of systemic skin symptoms with persistent myalgia or fever, and treatment should be administered promptly, even without a suspicion of drug exposure.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download