1. Lee KH, Hwang SJ, Kim SH, Lee SH, Yu DK, Hwang JH, et al. Comparison of mortality and morbidity in multiple versus singleton very low birth weight infants in a neonatal intensive care unit. J Korean Med Sci. 2003; 18(6):779–782.

2. Ortibus E, Lopriore E, Deprest J, Vandenbussche FP, Walther FJ, Diemert A, et al. The pregnancy and long-term neurodevelopmental outcome of monochorionic diamniotic twin gestations: a multicenter prospective cohort study from the first trimester onward. Am J Obstet Gynecol. 2009; 200(5):494.e1–494.e8.

3. Russo FM, Pozzi E, Pelizzoni F, Todyrenchuk L, Bernasconi DP, Cozzolino S, et al. Stillbirths in singletons, dichorionic and monochorionic twins: a comparison of risks and causes. Eur J Obstet Gynecol Reprod Biol. 2013; 170(1):131–136.

4. Scher AI, Petterson B, Blair E, Ellenberg JH, Grether JK, Haan E, et al. The risk of mortality or cerebral palsy in twins: a collaborative population-based study. Pediatr Res. 2002; 52(5):671–681.

5. Wenstrom KD, Gall SA. Incidence, morbidity and mortality, and diagnosis of twin gestations. Clin Perinatol. 1988; 15(1):1–11.

6. Flenady V, Wojcieszek AM, Middleton P, Ellwood D, Erwich JJ, Coory M, et al. Stillbirths: recall to action in high-income countries. Lancet. 2016; 387(10019):691–702.

7. Heazell AE, Whitworth MK, Whitcombe J, Glover SW, Bevan C, Brewin J, et al. Research priorities for stillbirth: process overview and results from UK Stillbirth Priority Setting Partnership. Ultrasound Obstet Gynecol. 2015; 46(6):641–647.

8. Cheung YB, Yip P, Karlberg J. Mortality of twins and singletons by gestational age: a varying-coefficient approach. Am J Epidemiol. 2000; 152(12):1107–1116.

9. Refuerzo JS, Momirova V, Peaceman AM, Sciscione A, Rouse DJ, Caritis SN, et al. Neonatal outcomes in twin pregnancies delivered moderately preterm, late preterm, and term. Am J Perinatol. 2010; 27(7):537–542.

10. Committee on Practice Bulletins—Obstetrics. Society for Maternal–Fetal Medicine. Practice bulletin no. 169: multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2016; 128(4):e131–e146.
11. Reddy UM, Laughon SK, Sun L, Troendle J, Willinger M, Zhang J. Prepregnancy risk factors for antepartum stillbirth in the United States. Obstet Gynecol. 2010; 116(5):1119–1126.

12. Park YS, Choi SH, Shim KS, Chang JY, Hahn WH, Choi YS, et al. Multiple births conceived by assisted reproductive technology in Korea. Korean J Pediatr. 2010; 53(10):880–885.

13. Rosenstein MG, Snowden JM, Cheng YW, Caughey AB. The mortality risk of expectant management compared with delivery stratified by gestational age and race and ethnicity. Am J Obstet Gynecol. 2014; 211(6):660.e1–660.e8.

14. Smith GC. Life-table analysis of the risk of perinatal death at term and post term in singleton pregnancies. Am J Obstet Gynecol. 2001; 184(3):489–496.

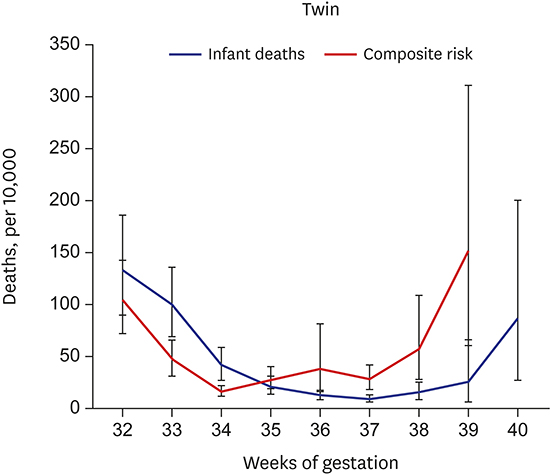
15. Page JM, Pilliod RA, Snowden JM, Caughey AB. The risk of stillbirth and infant death by each additional week of expectant management in twin pregnancies. Am J Obstet Gynecol. 2015; 212(5):630.e1–630.e7.

16. Unal ER. Fetal surveillance and timing of delivery for multiples. Clin Obstet Gynecol. 2015; 58(3):676–689.

17. Cheong-See F, Schuit E, Arroyo-Manzano D, Khalil A, Barrett J, Joseph KS, et al. Prospective risk of stillbirth and neonatal complications in twin pregnancies: systematic review and meta-analysis. BMJ. 2016; 354:i4353.

18. Lee HJ, Kim SH, Chang KH, Sung JH, Choi SJ, Oh SY, et al. Gestational age at delivery and neonatal outcome in uncomplicated twin pregnancies: what is the optimal gestational age for delivery according to chorionicity? Obstet Gynecol Sci. 2016; 59(1):9–16.

19. Rosenstein MG, Cheng YW, Snowden JM, Nicholson JM, Caughey AB. Risk of stillbirth and infant death stratified by gestational age. Obstet Gynecol. 2012; 120(1):76–82.

20. Kahn B, Lumey LH, Zybert PA, Lorenz JM, Cleary-Goldman J, D'Alton ME, et al. Prospective risk of fetal death in singleton, twin, and triplet gestations: implications for practice. Obstet Gynecol. 2003; 102(4):685–692.

21. National Collaborating Centre for Women's and Children's Health (GB). Multiple Pregnancy: the Management of Twin and Triplet Pregnancies in the Antenatal Period. London, United Kingdom: RCOG Press;2011.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download