1. Corrigan FM, Broome H, Dorris L. A systematic review of psychosocial interventions for children and young people with epilepsy. Epilepsy Behav. 2016; 56:99–112.

2. Camfield P, Camfield C. Incidence, prevalence and aetiology of seizures and epilepsy in children. Epileptic Disord. 2015; 17(2):117–123.

3. Filippini M, Boni A, Giannotta M, Gobbi G. Neuropsychological development in children belonging to BECTS spectrum: long-term effect of epileptiform activity. Epilepsy Behav. 2013; 28(3):504–511.

4. Jackson DC, Dabbs K, Walker NM, Jones JE, Hsu DA, Stafstrom CE, et al. The neuropsychological and academic substrate of new/recent-onset epilepsies. J Pediatr. 2013; 162(5):1047–1053.e1.

5. Alfstad KA, Torgersen H, Van Roy B, Hessen E, Hansen BH, Henning O, et al. Psychiatric comorbidity in children and youth with epilepsy: an association with executive dysfunction? Epilepsy Behav. 2016; 56:88–94.

6. Bailet LL, Turk WR. The impact of childhood epilepsy on neurocognitive and behavioral performance: a prospective longitudinal study. Epilepsia. 2000; 41(4):426–431.

7. Hermann BP, Jones JE, Sheth R, Koehn M, Becker T, Fine J, et al. Growing up with epilepsy: a two-year investigation of cognitive development in children with new onset epilepsy. Epilepsia. 2008; 49(11):1847–1858.

8. Austin JK, Harezlak J, Dunn DW, Huster GA, Rose DF, Ambrosius WT. Behavior problems in children before first recognized seizures. Pediatrics. 2001; 107(1):115–122.

9. Oostrom KJ, Smeets-Schouten A, Kruitwagen CL, Peters AC, Jennekens-Schinkel A; Dutch Study Group of Epilepsy in Childhood. Not only a matter of epilepsy: early problems of cognition and behavior in children with “epilepsy only”--a prospective, longitudinal, controlled study starting at diagnosis. Pediatrics. 2003; 112(6 Pt 1):1338–1344.

10. Berg AT, Smith SN, Frobish D, Levy SR, Testa FM, Beckerman B, et al. Special education needs of children with newly diagnosed epilepsy. Dev Med Child Neurol. 2005; 47(11):749–753.

11. Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006; 59(1):35–41.

12. Scarpina F, Tagini S. The stroop color and word test. Front Psychol. 2017; 8:557.

13. Williams J, Rickert V, Hogan J, Zolten AJ, Satz P, D'Elia LF, et al. Children's color trails. Arch Clin Neuropsychol. 1995; 10(3):211–223.

14. DuPaul GJ. ADHD Rating Scale-IV: Checklists, Norms, and Clinical Interpretation. New York, NY: Guilford Press;1998.
15. Shin MS, Cho SC, Chun SY, Hong KE. A study of the development and standardization of ADHD diagnostic system. J Korean Acad Child Adolesc Psychiatry. 2000; 11(1):91–99.
16. Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatr. 1981; 46(5-6):305–315.
17. Spielberger CD. State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press;1973.
18. Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989; 30(4):389–399.
19. Berl MM, Terwilliger V, Scheller A, Sepeta L, Walkowiak J, Gaillard WD. Speed and complexity characterize attention problems in children with localization-related epilepsy. Epilepsia. 2015; 56(6):833–840.

20. Reilly C, Agnew R, Neville BG. Depression and anxiety in childhood epilepsy: a review. Seizure. 2011; 20(8):589–597.

21. Thome-Souza S, Kuczynski E, Assumpção F Jr, Rzezak P, Fuentes D, Fiore L, et al. Which factors may play a pivotal role on determining the type of psychiatric disorder in children and adolescents with epilepsy? Epilepsy Behav. 2004; 5(6):988–994.

22. Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998; 18(7):765–794.
23. Jones JE, Watson R, Sheth R, Caplan R, Koehn M, Seidenberg M, et al. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007; 49(7):493–497.

24. Riikonen R. Long-term outcome of patients with West syndrome. Brain Dev. 2001; 23(7):683–687.

25. Scheffer IE, Zhang YH, Jansen FE, Dibbens L. Dravet syndrome or genetic (generalized) epilepsy with febrile seizures plus? Brain Dev. 2009; 31(5):394–400.

26. Blume WT. Lennox-Gastaut syndrome: potential mechanisms of cognitive regression. Ment Retard Dev Disabil Res Rev. 2004; 10(2):150–153.

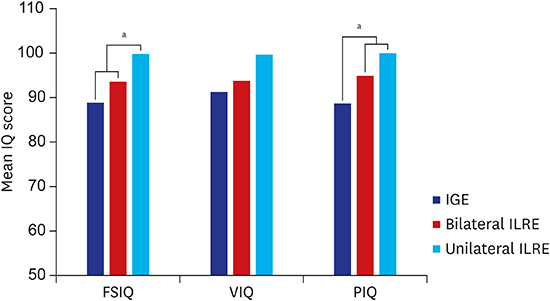
27. Jeong MH, Yum MS, Ko TS, You SJ, Lee EH, Yoo HK. Neuropsychological status of children with newly diagnosed idiopathic childhood epilepsy. Brain Dev. 2011; 33(8):666–671.

28. Sarkis RA, Pietras AC, Cheung A, Baslet G, Dworetzky B. Neuropsychological and psychiatric outcomes in poorly controlled idiopathic generalized epilepsy. Epilepsy Behav. 2013; 28(3):370–373.

29. Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006; 129(Pt 10):2609–2619.

30. Ebus S, Arends J, Hendriksen J, van der Horst E, de la Parra N, Hendriksen R, et al. Cognitive effects of interictal epileptiform discharges in children. Eur J Paediatr Neurol. 2012; 16(6):697–706.

31. Glennon JM, Weiss-Croft L, Harrison S, Cross JH, Boyd SG, Baldeweg T. Interictal epileptiform discharges have an independent association with cognitive impairment in children with lesional epilepsy. Epilepsia. 2016; 57(9):1436–1442.

32. Sánchez Fernández I, Loddenkemper T. Interictal epileptiform discharges and cognition. Dev Med Child Neurol. 2017; 59(1):13–14.

33. Schapiro AC, McClelland JL, Welbourne SR, Rogers TT, Lambon Ralph MA. Why bilateral damage is worse than unilateral damage to the brain. J Cogn Neurosci. 2013; 25(12):2107–2123.

34. Rohrer-Baumgartner N, Zeiner P, Egeland J, Gustavson K, Skogan AH, Reichborn-Kjennerud T, et al. Does IQ influence associations between ADHD symptoms and other cognitive functions in young preschoolers? Behav Brain Funct. 2014; 10:16.

35. Kang SH, Yum MS, Kim EH, Kim HW, Ko TS. Cognitive function in childhood epilepsy: importance of attention deficit hyperactivity disorder. J Clin Neurol. 2015; 11(1):20–25.

36. Gascoigne MB, Smith ML, Barton B, Webster R, Gill D, Lah S. Attention deficits in children with epilepsy: preliminary findings. Epilepsy Behav. 2017; 67:7–12.

37. Dunn DW, Kronenberger WG. Childhood epilepsy, attention problems, and ADHD: review and practical considerations. Semin Pediatr Neurol. 2005; 12(4):222–228.

38. Dunn DW, Austin JK, Harezlak J, Ambrosius WT. ADHD and epilepsy in childhood. Dev Med Child Neurol. 2003; 45(1):50–54.

39. Williams J, Phillips T, Griebel ML, Sharp GB, Lange B, Edgar T, et al. Factors associated with academic achievement in children with controlled epilepsy. Epilepsy Behav. 2001; 2(3):217–223.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download