INTRODUCTION
Distal digital replantation is a challenging procedure that has undergone revolutionary advances in microsurgical techniques and instruments since the successful replantation reported by Tamai in 1967.
1 There have been doubts about the necessity of distal digital replantation in the past because loss of a single digit except for the thumb has limited effect on the function of the hand.
23 However, due to the advances mentioned above, the goal of digital replantation surgery in this era is now focused on good functional and aesthetic outcome. One of the most important factors for successful outcomes is a shortened ischemia time. Although there have been reports of successful replantation with prolonged ischemia time, it is generally stated that successful digital replantation is associated with less than 12 hours of warm and 24 hours of cold ischemia time.
In other parts of medicine where optimal clinical course is associated with a shortened ischemia time, the concepts of ‘door-to-needle time’ and ‘door-to-balloon time’ have been developed to achieve a better outcome in morbidity and mortality. The purpose of this study was to present a concept of door-to-surgery time and test the hypothesis that success in distal digital replantation is associated with this time.
METHODS
Patients
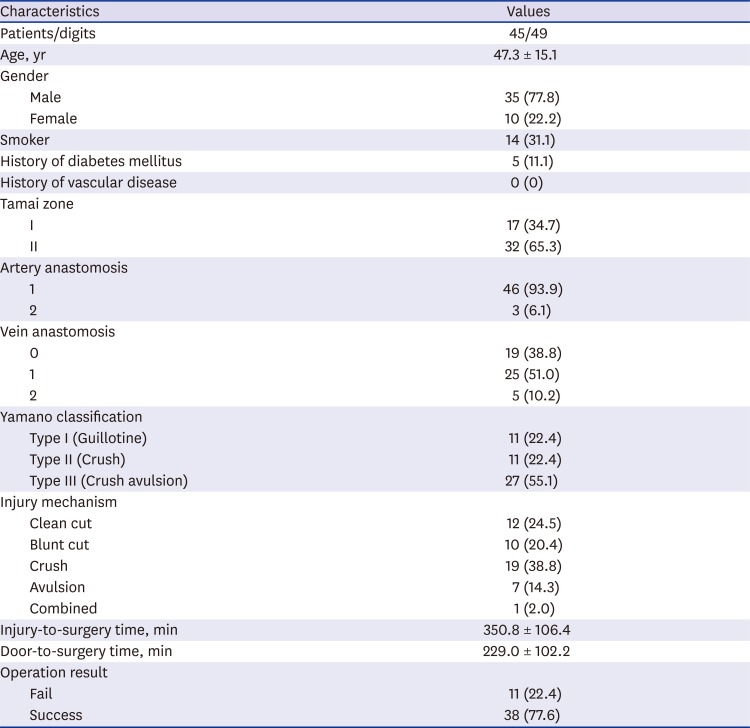
Between January 2007 and January 2016, 45 consecutive patients with 49 digital amputations at or distal to the distal phalanges were included in the study. Data regarding patient demographics, amputation characteristics, injury-to-surgery time, door-to-surgery time, and surgical outcome were collected. The injury-to-surgery time was defined as the period between the time of injury to the initiation of surgery. The door-to-surgery time was defined as the period between the time of arrival at the emergency room and the initiation of surgery.
Surgical method
Preoperative evaluation was done at the emergency room. Replantations were performed with the patients under general anesthesia or brachial plexus block. A pneumatic tourniquet was applied to the upper arm and the amputated part was prepared under the microscope. After adequate debridement and cleansing, the digital artery was anastomosed with 10-0 or 11-0 ethilon by simple interrupted suture. When venous repair was not possible due to the lack of available vein or severe soft-tissue damage, artery-only replantation was performed. A paraungual stab incision was made to prevent venous congestion and either topical dripping of heparinized saline or application of medical leeches was done immediately after operation. Systemic anticoagulation was achieved through administration of 20,000 units of heparinized saline and 500 mL of low-molecular-weight dextran for 7 days. The survival outcome was measured on the seventh day after surgery by visual assessment of circulation to the fingertip with normal skin color.
Statistical analysis
Baseline characteristics were summarized using descriptive statistics. Continuous variables were compared parametrically using Student's t-test or non-parametrically using the Mann-Whitney U-test. Categorical variables were compared using χ2 test or Fisher's exact test as appropriate. Univariate and multivariate analyses were done using logistic regression with backward conditional method to assess the significant factor associated with the surgical outcome. A two-sided P value < 0.05 was taken as statistically significant. All statistical analyses were performed using SPSS version 19.0 (SPSS, Inc., IBM Company, Chicago, IL, USA).
Ethics statement
This study was reviewed and approved by the Institutional Review Board of Chonnam National University Hospital (CNUH-2017-022). Informed consent was waived by the board.
DISCUSSION
Advances in microsurgery have greatly refined distal digital replantation. Hence, the goal of digital replantation in this era is now more focused on achieving good functional and aesthetic outcome. The purpose of this study was to present the concept of door-to-surgery time; a concept that has changed treatment goals in other parts of medicine where the outcome is associated with a shortened ischemia time, and test the hypothesis that success in distal digital replantation is associated with this time.
The overall success rate of 77.6% is comparable to the results of previous studies.
4567 One of the most important factors to a successful replantation is a shortened ischemia time. Although there have been reports of successful digital replantation after 94 hours of cold ischemia and 42 hours of warm ischemia time,
89 it is generally stated that irreversible ischemic injury occurs after 2–4 hours of warm ischemia and 6–8 hours of cold ischemia time.
10 Dec's analysis of ischemia time which included two studies demonstrated that the success rate was greater in patients with less than 12 hours of ischemia.
11 However, this ischemia time is not easily modifiable as the length is determined predominantly by the patient's arrival to the hospital.
The time to treatment greatly affects numerous clinical outcomes in other parts of medicine as well. In stroke patients, the Brain Attack Coalition recommends that the time from emergency room arrival to initiation of rt-PA (door-to-needle time) should be 60 minutes or less.
12 In acute myocardial infarction, the American College of Cardiology Foundation/American Heart Association recommended that the door-to-needle time and the door-to-balloon time (the time from emergency room arrival to primary percutaneous coronary intervention) be 30 minutes or less and 90 minutes or less, respectively.
13 The recommendation is based on the findings of decreased mortality with shortened door-to-balloon time.
14
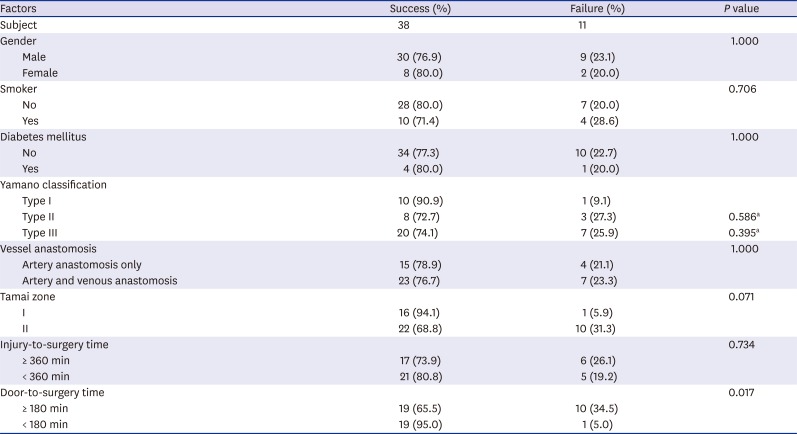
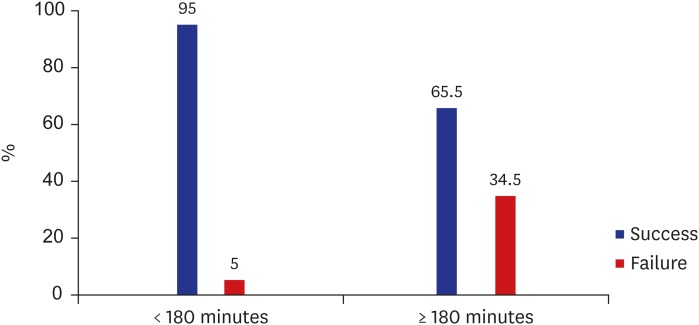
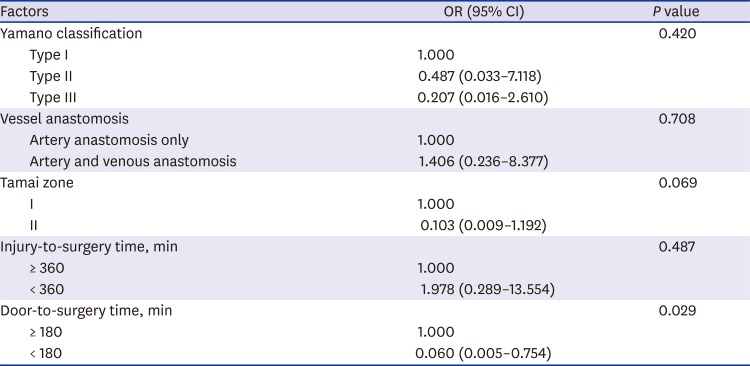
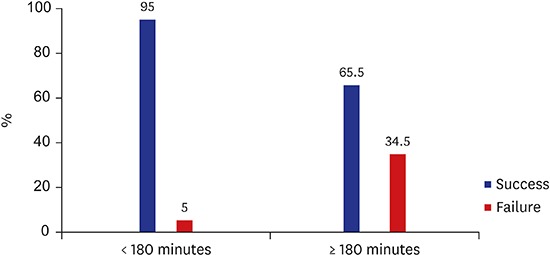
As the goal for digital replantation is good functional and aesthetic outcome, a modifiable time goal is needed for better surgical outcome. To our knowledge, there are no other reports analyzing the surgical outcome with the injury-to-surgery time or door-to-surgery time. In our study, patients with a door-to-surgery time less than 180 minutes resulted in a significantly better surgical outcome. The optimal door-to-surgery time in distal digital replantation can be prolonged compared to cerebral stroke or myocardial infarction patients, because digits lack muscle tissue and are much less susceptible to ischemic damage.
10 Nevertheless, this concept can present a modifiable time goal for optimal surgical outcome. Interestingly, the injury-to-surgery time was not a significant factor associated with surgical outcome. The results of our study suggest that even if the time from injury to the emergency room is short, if the door-to-surgery time is prolonged the surgical outcome may be worse. Also, the injury-to-emergency room time is not a factor that can be modified by the efforts of the medical staff. Therefore, the focus of efforts to modify the door-to-surgery time is a valid concept.
Previous reports comparing clean cut injury and crush type injury demonstrated a significant difference in success rate.
1115 Although there was a trend for a greater success rate in clean cut injury (Yamano type I, 90.9%) compared to the crush types (type II, 72.7%; type III, 74.1%), the difference in success rate was not statistically significant.
The success rate of digital replantation also depends on the availability of vessels at the level of the amputation. Venous anastomosis is particularly difficult in fingertip replantation due to the small size of the vessels and often leads to replantation failure.
16 Many surgical techniques have been developed to overcome this anatomical problem, including volar vein repair,
617 arteriovenous shunting,
61819 and external venous drainage using medical
20 or chemical leeches.
21 Sebastin et al.
15 reported that the repair of a vein improved overall survival in Tamai zone I and zone II classification. However, in a recent study by Huang and Yeong,
22 the success rate was not dependent on the presence of venous anastomosis. In our study, there was no difference in the success rate based on the availability of venous anastomosis in patients that underwent arterial anastomosis.
The meta-analysis reports of success rates based on the level of injury are contradicting. Dec
11 reported that the success rate of distal phalanx is significantly lower than digits amputated at proximal levels. Sebastin and Chung
15 reported no significant difference of success rates in Tamai zone I and zone II replantations. There was no significant difference in the success rates based on the Tamai zone in this study.
Randomized controlled trials are ethically not possible in testing the hypothesis of door-to-surgery time of digital replantation in real patients. However, our study proves the concept of door-to-surgery time is associated with the surgical outcome using multivariate regression analysis. There are several limitations to our study due to the retrospective design. First, overview of all known clinical factors related to success rates was not possible. The study is limited by the fact that the injury-to-the-emergency room time was extrapolated by the statement of the patient and the exact time of warm or cold ischemia is not known. Selection of patients that deem to have good surgical results may have undergone surgery and therefore selection bias cannot be excluded. Secondly, further studies are needed to confirm our finding due to the small sample size. Our hospital is located within the central district of the city and the injury-to-surgery time and door-to-surgery time of our study may not be feasible or applicable to other hospital settings. Thirdly, long-term data for functional and aesthetic outcome was limited. Although the door-to-surgery time is not a factor that can be modified by the sole efforts of a reconstructive surgeon, it is an important factor associated with successful outcome. Well-designed, large studies are needed to refine the door-to-surgery time considering strategies to shorten this time.
In conclusion, patients with digital replantation within 180 minutes of door-to-surgery time have significantly better success rates. As the door-to-surgery time is a modifiable factor, effort must be made to achieve this goal. Further studies are warranted to determine the optimal door-to-surgery time for better success rates.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download