INTRODUCTION
Fibrous hamartoma of infancy (FHI) is a rare, benign, dermal and subcutaneous proliferation of fibrous tissue, which usually appears within the first 2 years of life.
1 Reye
2 first described this disease in 1956 as subdermal fibromatous tumors of infancy, but in 1965, it was renamed “fibrous hamartoma of infancy” by Enzinger.
3 It has been accepted worldwide that FHI is a hamartoma that consists of benign tissues of the site in which they arise.
4
Various skin changes concurrent with FHI have been reported. According to Grynspan et al.,
5 who featured cutaneous changes in FHI, the most common histopathological finding was eccrine gland hyperplasia. However, a review of the literature reveals only 2 cases of FHI presenting with hyperhidrosis in the world, and no case in Korea.
67 In this study, we report the first Korean case of FHI with hyperhidrosis and hypertrichosis.
CASE DESCRIPTION
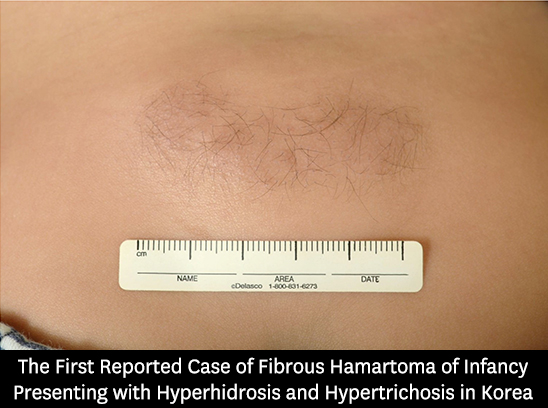
A 13-month-old male infant was brought to the Department of Dermatology of the Yeungnam University Hospital owing to a single asymptomatic plaque on March 7, 2016. His parents first noticed the lesion at approximately 4 months of age. At 6 months of age, the lesion was a normal skin-colored soft plaque on the lumbar area, with hypertrichosis (
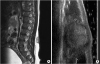
Fig. 1). In order to evaluate the internal characteristics of the tumor, imaging studies were performed. Magnetic resonance imaging (MRI) (
Fig. 2A) and ultrasonography (
Fig. 2B) revealed a 4 × 2-cm mass lesion in the subcutaneous fat layer at the lumbar spine 3–4 level. Furthermore, no visible connection between the spinal cord and the lesion was found in both studies, indicating a disease other than spinal dysraphism. During observation, the lesion became larger and firm, and intermittent sweating on the surface was noticed.
Fig. 1
A 4 × 2-cm normal skin-colored soft nodule on the lumbar area, showing hypertrichosis on the surface at 6 months of age.

Fig. 2
Imaging findings of the lesion. (A) T2-weighted MRI showed an abnormal mass, not connected to the spinal cord in the subcutaneous fat layer at the L3–4 level; (B) Ultrasonography of the lesion showed a 4 × 2-cm abnormal echogenicity in the subcutaneous fat layer at the L3–4 level.
MRI = magnetic resonance imaging.
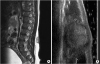
When the patient was 13 months of age, physical examination revealed a 5 × 3-cm firm, normal skin-colored plaque on the lumbar area, with localized prominent hypertrichosis and hyperhidrosis (
Fig. 3). We performed punch biopsy of the lesion. Histopathological findings revealed mature hair follicular structures and fat tissue (
Fig. 4A). Well-defined fibrous trabeculae that consist of spindle cells and increased number of eccrine glands, admixed with mature adipose tissue (
Fig. 4B), and primitive mesenchymal tissue were also noted in the lower reticular dermis (
Fig. 4C). Moreover, the spindle cells were positively stained for smooth muscle actin and negatively for calponin (
Fig. 4D). In conclusion, the histopathological findings were consistent with FHI with eccrine hyperplasia. After diagnosing this as a case of FHI, we decided to further observe the lesion and not perform surgery.
Fig. 3
A 5 × 3-cm normal skin-colored nodule on the lumbar area with localized prominent hypertrichosis at 13 months of age.

Fig. 4
Histopathological findings of the skin. (A) Mature hair follicular structures and fat tissue, (B) well-defined fibrous trabeculae that consist of spindle cells and increased number of eccrine glands, admixed with mature adipose tissue, (C) primitive mesenchymal tissue, and (D) positive staining for smooth muscle actin.

DISCUSSION
FHI usually occurs within the first 2 years of life, with approximately 23% of cases being detected at birth.
8 It shows a predominance in male patients and usually occurs on the trunk, especially the axilla, and on the upper extremities; it rarely presents on the distal extremities, head, neck, and scrotum.
9 Almost all the reported cases are solitary, movable nodules with ambiguous borders and are located in the deep dermis or subcutaneous layer.
10 In our case, FHI occurred within the first 2 years of life on the trunk of a male patient. Specifically, the condition was characterized by a solitary plaque with an ambiguous border and was located in the dermis.
Histopathology is the key method for the diagnosis of FHI, and biopsy should be performed to differentiate FHI from other clinically similar lesions, such as infantile fibromatosis, fibrolipoma, myofibroma, eccrine angiomatous hamartoma, and fibroblastic connective tissue nevus. Characteristic histological features for FHI lesion are as follows: 1) dense fiber bundles, formed by the spindle-shaped fibroblasts, myofibroblasts, and collagen fibers, 2) mesenchymal cells containing myxoid matrix or an asterism of small round-shaped primitive mesenchymal cells, and 3) mature adipose tissue interspersed between the other two structural elements.
10 In our case, histopathological findings showed well-defined fibrous trabeculae, mature adipose tissue, primitive mesenchymal cells, and spindle cells, positively stained for smooth muscle actin, which are indicative of FHI. Moreover, an increased number of eccrine glands in the dermis were observed.
Local excision is the treatment of choice for FHI management because no evidence of tumor regression has been identified, so far.
11 Even with incomplete excision, the recurrence rate is low, and it provides an excellent prognosis.
1 Local recurrences have been reported in up to 16% of cases owing to an inadequate primary excision, and in those cases, reoperation was sufficient to cure the disease.
1 Delayed surgery was not associated with an increased risk of operative complications or malignant changes. In contrast, it seemed to facilitate complete resection of the tumor, because an established tumor is more likely to be encapsulated, making the excision procedure easier.
11
FHI may present overlying skin changes, such as alterations in pigment,
12 hypertrichosis,
13 and hyperhidrosis.
7 Although eccrine hyperplasia is the most common skin change in FHI,
5 hyperhidrosis is extremely rarely reported. To our knowledge, only 2 cases of FHI with hyperhidrosis have been reported in the world. First, Weinberger et al.
7 reported a case of FHI presenting as a perspiring neck mass in 1993. Next, in 2015, Melnick et al.
6 reported a case of FHI presenting with hypertrichosis and hyperhidrosis, which is quite similar to our case. Both cases were reported in the US, and no case of FHI presenting with hyperhidrosis has been reported in Korea, until now.
The present case is the first Korean case of FHI with hyperhidrosis and hypertrichosis. FHIs with these features may be clinically confused with other diseases, such as spinal dysraphism, owing to its rarity. Misdiagnosis may lead to unnecessary consequences, such as concerns of the patient's family, and invasive procedures. Therefore, FHI should be considered in the differential of a solitary nodule in infants.