INTRODUCTION
Sending a message of hope, a famous Korean actor made a successful comeback after he had overcome complex regional pain syndrome (CRPS), a rare and intractable disorder. Treating CRPS is difficult because of the lack of objective diagnostic criteria, clarity in the pathophysiology of the disease, and awareness among not only the public but also the medical community.
1
CRPS is caused by an abnormality of the autonomic nervous system,
2 characterized by a chronic pain condition
3 that affects the peripheries typically after an injury.
4 In 1864, the disease was first termed as causalgia.
5 In 1994, the International Association for the Study of Pain established diagnostic criteria for reflex sympathetic dystrophy and causalgia, and renamed them as CRPS types I and II, respectively.
4 The signs, symptoms, and treatment methods are similar for both CRPS types I and II; the difference between the two is the evidence of nerve damage in the latter type.
6 There is a lack of a single accurate test method to diagnose CRPS. Clinical signs and symptoms are diagnosed when they meet certain criteria. Aside from these criteria, a three-phase bone scintigraphy, a simple radiograph, skin temperature measurement, quantitative sensory testing, and autonomic nerve function measurement are additionally used.
17 Although CRPS has not yet been clarified medically, the victims claim that CRPS is caused by trauma, such as traffic accidents.
8 In the United States, there are 5.5 CRPS patients per 100,000 patients per year,
9 and in the Netherlands, there 26.2 CRPS patients per 100,000 patients.
10 According to the Health Insurance Review and Assessment Service in Korea, there were 8,276 CRPS type I patients and about 10,000 patients complain of CRPS symptoms each year.
11
CRPS is not an uncommon side effect of an invasive medical procedure, such as surgery.
1213 In an invasive medical procedure, such as surgery, severe pain is common, and the degree of pain is proportional to the level of invasiveness of the medical treatment. However, CRPS is not proportional to the severity of the injury, and it is painful, unlike the degree of damage; it causes severe neuropathic pain not limited to the single peripheral nerve area.
814 Moreover, the annual amount of medical care expenses has increased, from KRW 3.8 billion in 2012 to KRW 5.5 billion in 2016.
11
CRPS is an important issue in the area of liability for medical malpractice lawsuit because the litigation costs of patient with CPRS caused by invasive treatment or trauma have risen dramatically, from several hundred million KRW to billions of KRW, unlike other existing disease.
8
In Korea, the first CRPS-related lawsuit for damage after a traffic accident was sentenced in 2005.
15 Legal issues related to the establishment of damage in lawsuits involving CRPS are hounded by controversy.
8
Therefore, this article aims to analyze medical malpractice lawsuits involving CRPS, which occurred after the disputed medical treatment, to provide baseline data on the courts' opinion and characteristics of the cases.
METHODS
This study analyzed 23 lawsuit judgments involving CRPS that were sentenced from January 1, 2005 to December 31, 2015.
The databases of the Supreme Court of Korea's Written Judgment Management System and each court's service, which provided copies of the judgment to any subscriber, were used to search and collect cases. Using the search terms “compensatory damage in medical practice” and “complex regional pain syndrome,” 402 lawsuit judgments were retrieved. Of these judgments, this study excluded those involving lawsuits: 1) alleging medical malpractice in the treatment the plaintiff received after diagnosis of CRPS, 2) against an offender in a traffic accident, and 3) for CRPS that occurred after the plaintiff underwent a treatment at an oriental medical clinic or a dental clinic. Consequently, 23 lawsuits, which involved the diagnosis of CRPS after the disputed medical treatment, were selected for this study. Subsequently, the authors examined the plaintiff's and defendant's claims, opinion of the court, amounts claimed and awarded damage, the type of CRPS, site of pain complaint, trauma (or event) prior to medical treatment, nerve injury, and treatment after diagnosis of CRPS.
RESULTS
This study analyzed 23 judgments in medical malpractice lawsuits involving CRPS. Of the 23 lawsuit judgments, 15 were concluded at the first trial, and 12 were partially ruled in favor of the plaintiff. The average amount (KRW) claimed was 470,638,385 ± 860,634,092 (21,000,000 to 4,020,000,000), and that awarded was 72,906,843 ± 53,389,367 (15,000,000 to 181,080,803). Fifteen of the 23 cases of medical malpractice occurred in the orthopedics department (
Table 1); these cases involved medical procedures for ligament rupture (four cases), arthroplasty-related surgery (two cases), bone fracture repair (two cases), disc surgery (two cases), nerve decompression surgery (two cases), arthroscopic surgery (one case), physical therapy (one case), and an incisional bone biopsy of the humerus (one case).
Table 1
General characteristics of the cases (n = 23)

|
Characteristics |
No. (%) of cases |
|
Progress of lawsuit |
First instance |
15 (65.2) |
|
Appeal |
7 (30.4) |
|
Reverse and remand |
1 (4.3) |
|
Sentence |
Partially awarded to plaintiff |
12 (52.2) |
|
Dismissal |
11 (47.8) |
|
Medical specialties |
Orthopedics |
15 (65.2) |
|
Urology |
2 (8.7) |
|
Plastic surgery |
1 (4.3) |
|
Cardiology |
1 (4.3) |
|
Thoracic and cardiovascular surgery |
1 (4.3) |
|
Anesthesiology and pain medicine |
1 (4.3) |
|
Not identified |
2 (8.7) |

Of the 23, there were also two cases in the urology department (involving dorsal neurectomy and penile augmentation by fat graft), and one each in the plastic surgery (fat harvesting from thigh), cardiology (transradial coronary angiography), thoracic and cardiovascular surgery (laser ablation and phlebectomy for lower extremity varicose veins), and anesthesiology and pain medicine (spinal anesthesia) departments. The department could not be identified in the two other cases, which were related to physical therapy.
The plaintiffs in 16 of the 23 cases had CRPS type I, and those in six cases had CRPS type II. In 11 of the 23 cases, the site of the pain was located in the lower limb, such as foot, ankle, and leg. In 14 of 23 cases, there was no presence of trauma (or event) prior to medical treatment, whereas in other cases, the plaintiffs encountered, traffic accidents (four cases), contusions (two cases), falls (two cases), and laceration (one case) (
Table 2).
Table 2
Characteristics of CRPS in the 23 lawsuit judgments

|
Characteristics |
No. (%) of cases |
|
Type of CRPS |
Type I |
16 (69.6) |
|
Type II |
6 (26.1) |
|
Unspecified |
1 (4.3) |
|
Pain site |
Upper limb |
9 (39.1) |
|
Lower limb |
11 (47.2) |
|
Both limbs |
1 (4.3) |
|
Penis |
2 (8.7) |
|
Nerve injury |
Yes |
7 (30.4) |
|
No |
16 (69.6) |
|
Presence of trauma (or event) prior to diagnosis of CRPS |
Traffic accident |
4 (17.4) |
|
Contusion |
2 (8.7) |
|
Fall |
2 (8.7) |
|
Laceration |
1 (4.3) |
|
None |
14 (60.9) |

Table 3 shows a detailed summary of the cases awarded to plaintiffs. In four of the six cases of CRPS type II, nerve damages comprised the main admitted malpractice according to the judgment.
Table 3
Detailed summary of awarded cases to plaintiffs

|
No. |
CRPS type |
Trauma before medical practice |
Medical practice |
Nerve damage |
Admitted violations of duty by judgment |
Not admitted |
Amount claimed (KRW) |
Amount awarded (KRW) |
|
1 |
I |
No |
Traction therapy of finger |
No |
Excessive external force during traction therapy |
Not applicable |
244,589,316 |
64,808,175 |
|
2 |
I |
No |
Repair for labrum tear and scapular glenoid fracture |
No |
Malpractice during surgery |
Lack of informed consent |
274,043,818 |
113,225,658 |
|
3 |
I |
Laceration |
Tenorrhaphy and neurorrhaphy for the second finger flexor digitorum profundus rupture |
No |
Diagnostic error |
Not applicable |
296,251,405 |
28,485,000 |
|
Malpractice about transferring patient to another hospital, lack of informed consent |
|
4 |
I |
No |
Total knee arthroplasty for osteoarthritis, meniscus resection for meniscus tear |
No |
Poor choice of treatment method, lack of informed consent |
Not applicable |
233,674,249 |
95,152,190 |
|
5 |
I |
No |
Total hip arthroplasty for femur head avascular necrosis, open reduction internal fixation for femur fracture |
No |
Performance error, malpractice in postoperative monitoring and treatment |
Not applicable |
207,168,195 |
75,139,653 |
|
6 |
I |
No |
Penile augmentation by autologous fat graft |
No |
Lack of informed consent |
Malpractice during surgery |
114,000,000 |
20,000,000 |
|
7 |
II |
Traffic accident |
Incisional bone biopsy of the humerus |
Axillary nerve |
Malpractice during biopsy |
Error in choice of treatment method |
310,956,648 |
79,037,357 |
|
8 |
II |
No |
Dorsal neurectomy |
Dorsal nerve of the penis |
Lack of informed consent for treatment method and generally possible side effect after surgery |
Not performing of preoperative evaluation, poor choice of treatment method, improper postoperative treatment |
602,676,695 |
30,000,000 |
|
9 |
II |
Contusion |
Arthroscopy under the spinal anesthesia for anterior cruciate ligament rupture |
Superficial peroneal nerve, sural nerve |
Negligence for nerve damage on spinal anesthesia, negligence for supervising physician as hospital manager |
Not applicable |
68,682,815 |
26,938,702 |
|
10 |
II |
No |
Anterior transposition of the ulnar nerve for cubital tunnel syndrome |
Ulnar nerve |
Negligence in nerve damage during surgery, lack of informed consent |
Diagnostic error, poor choice of treatment method, malpractice in monitoring patient |
942,082,238 |
181,080,803 |
|
11 |
II |
No |
Arthroscopic excision of the popliteal cyst and neurolysis |
Tibial, peroneal nerve |
Negligence during surgery |
Poor choice of treatment method |
250,328,450 |
146,014,579 |
|
12 |
II |
No |
Carpal tunnel release for carpal tunnel syndrome |
Median nerve |
Lack of informed consent |
Performance error |
41,985,330 |
15,000,000 |

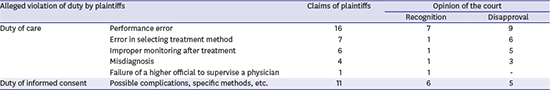
There were 16 cases in which the plaintiffs claimed performance error in, for example, a surgical procedure; in seven of these cases, the court found that the defendant was liable because of negligence (
Table 4). Of these seven cases, four were related to nerve injuries; two were related to rupture of the surgical site; and one was related to an injury due to excessive external force (
Fig. 1). There were 11 cases in which the plaintiffs claimed violation of the duty of obtaining informed consent. Of these, the court did not recognize the duty to explain the CRPS, because it is an unpredictable side effect, and recognized the violation of the duty of obtaining informed consent on only the general complications that may occur before and after the medical treatment, and specific methods of treatment.
Table 4
Alleged breaches of duties by plaintiffs and the courts' judgment

|
Alleged violation of duty by plaintiffs |
Claims of plaintiffs |
Opinion of the court |
|
Recognition |
Disapproval |
|
Duty of care |
Performance error |
16 |
7 |
9 |
|
Error in selecting treatment method |
7 |
1 |
6 |
|
Improper monitoring after treatment |
6 |
1 |
5 |
|
Misdiagnosis |
4 |
1 |
3 |
|
Failure of a higher official to supervise a physician |
1 |
1 |
- |
|
Duty of informed consent |
Possible complications, specific methods, etc. |
11 |
6 |
5 |

 | Fig. 1Performance errors during procedures/surgeries by judgment in cases with indemnity paid. 
|
In cases in which trauma occurred before the visit to the medical institution, six of the nine cases were dismissed. According to the court, three cases (traffic accident, fall, contusion) did not mention trauma relevance. In two of the six cases, the court held that it was not possible to exclude the occurrence of CRPS due to trauma; in one case, the court decided that CRPS was unlikely to be causally related to trauma. In the three cases in which the court ruled in favor of the plaintiffs, the medical staff was found to be negligent in the occurrence of CRPS, but the possibility of a traffic accident, bruising, or laceration could not be ruled out. The limitations of liability ratio of the defendants were from 30% to 60%.
DISCUSSION
After the analysis of the 23 medical malpractice lawsuits involving CRPS, the authors provided the results to physicians working in related fields in an attempt to propose preventive measures for avoiding medical malpractice lawsuits.
CRPS is a disease for which diagnosis and treatment is difficult.
1 The precipitating factors leading to the onset of CRPS are trauma, fracture, surgical procedure, and injection.
231016171819
The difference between CRPS types I and II can be identified based on nerve damage, although the symptoms, signs, and treatment are similar.
36 In this study, 16 of the 23 plaintiffs were diagnosed as CRPS type I, and the rest were CRPS type II. This result is similar to those of previous studies in Korea, which found that the ratio of CRPS types I to II was 7:3,
16 and 92.7% of all subjects had CRPS type I.
17
Although some studies have found that CRPS often occurs in the upper limb,
39101820 other studies have shown cases of symptoms in the lower limbs.
161719 The present study is consistent with these previous works, as 11 of the 23 cases involved CRPS occurring in the lower limbs and nine in the upper limbs. Further, this study found that the average period from disputed medical procedure to diagnosis was one year and two months. Cases in Korea showed that the mean duration from onset of symptoms to a diagnosis of CRPS is one year and one month. CRPS is a disease that affects the quality of life. Diagnosis within eight months is important for maintaining employment
17; thus, early diagnosis and treatment are also important.
1617
In summarizing the medical malpractice lawsuits involving CRPS, which were sentenced in courts from 2005 to 2015, this study found that more cases were sentenced after 2010 (4–5 cases/year) than before 2010 (1–2 cases/year).
Patients filed lawsuits claiming that CRPS was due to the negligence of physicians. Although CRPS is a poorly understood and unpredictable disease, there have been cases where the medical staff's negligence was recognized as the cause of CRPS. However, the court did not assign the medical staff's negligence only because CRPS occurred. In this study, plaintiffs mostly alleged performance error (16 cases), mostly recognized as negligence (7 cases). Of these seven cases, four involved negligence for nerve damage in the case of nerve injury.
The reason for the court's decision of negligence in the case of nerve damage is that the medical practitioners have a duty as care providers to avoid injuries to the nervous system. In the case of nerve damage, it is a complication that does not occur in most surgeries if caution is taken. Therefore, medical personnel need to be aware of the possibility of CRPS, despite its low probability, and care should be taken to avoid complications, including nerve damage. Looking at the recent trends in medical litigation, most of the plaintiffs claimed a breach of informed consent by medical personnel. This is presumed to be because the patient must prove medical personnel's negligence, in the case of violation of duty of care. Indeed, it is difficult to prove negligence in this case because of the nature of medical expertise. However, in case of violation of duty of informed consent, medical personnel are responsible for the verification.
21 In this study, 11 of the 23 cases claimed violation of duty of informed consent. The court's judgment is that the medical staff is liable if there is no explanation on, among others, the complications, aftereffects, and treatment methods, which may occur before practice. However, it was difficult to ascertain violations of duty of informed consent in case of side effects that are unpredictable or difficult to avoid even with the utmost care, as is the case of CRPS. It is thus necessary to explain CRPS as a complication that may occur during all upper extremity surgeries.
22 Explanations related to medical practice, such as surgery, general anesthesia, and transfusion, are now mandatory, not optional, and efforts must be made to clearly document patient descriptions and education.
Among the medical lawsuits analyzed in this study, nine were cases of trauma before medical practice. Of these, three cases ruled in favor of the plaintiff. In three cases, the trauma occurred before medical practice and was considered a limitation of the defendant's liability. The limitation was set because it was not possible to exclude the possibility that trauma contributes to the development of CRPS in the case of the coexistence of medical activities and trauma, such as traffic accidents or injuries.
Medical malpractice lawsuits are often filed because of patient complaints or lack of understanding of the negative outcomes, regardless of whether there is negligence.
23 Apart from the physician's acknowledgment of the fault mentioned, sufficient communication between the physician and the patient is needed to prevent medical disputes and litigation. One way is open disclosure (OD), which is the voluntary explanation of the incident to the patient and his/her caregiver when the incident occurs, communication of sympathy and regret, and investigation of the cause of the incident. This method includes apologizing if the cause of the incident is found to be a medical error, and then providing reasonable compensation and promising to strive to prevent recurrence.
24 OD can be used to reduce the number of medical litigation cases and related costs, moderate the intention to penalize medical staff, strengthen physician-patient relationships, increase the intention of recommendation and revisit of medical staff, improve the medical quality score, and diminish the physician's guilt. Healthcare providers and the public generally agree on such effects mentioned above.
25 In many countries, OD is encouraged, and related laws and systems are developed. In Korea, it is necessary to discuss public relations activities, guidelines and curriculum development, and the enactment of the Apology Law to encourage OD.
26
Unlike research through patient questionnaires or hospital medical records, judgment analysis is limited by missing information. There are also limitations in that the contents of the medical records and results of the tests are unknown. To overcome these limitations, the researchers analyzed not only the text but also the annexes and other contents to grasp all the information extractable from the rulings. Nonetheless, despite these limitations, this study, which analyzed the lawsuit judgments involving CRPS after treatment, provides useful information to related physicians and base data for preventing and coping with future medical lawsuits.
Physicians cannot be exempted from liability for intractable diseases of unknown origin. Nerve injury is the most common reason for liability in medical malpractice lawsuits related to the occurrence of the CRPS. Physicians must be careful of the possibility for the occurrence of this complication in every case in medical practice, including surgery, and recognize areas where practice and training can be improved, as well as the steps to be taken to prevent injury. Research and support should be made to prevent future medical accidents, disputes, and lawsuits.








 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download